Podcast
Questions and Answers
What does P.T. stand for in the context of the presentation?
What does P.T. stand for in the context of the presentation?
Physical Therapy
What are the therapeutic modalities and exercise regimens utilized by physical therapists in the management and treatment of stress urinary incontinence?
What are the therapeutic modalities and exercise regimens utilized by physical therapists in the management and treatment of stress urinary incontinence?
- Pelvic floor muscle training
- Biofeedback
- Electrical stimulation
- Behavioral strategies
- All of the above (correct)
Physical therapists only focus on treating stress urinary incontinence and do not collaborate with other healthcare professionals.
Physical therapists only focus on treating stress urinary incontinence and do not collaborate with other healthcare professionals.
False (B)
What are the two main muscles that make up the pelvic floor muscles?
What are the two main muscles that make up the pelvic floor muscles?
What is the definition of Stress Urinary Incontinence (SUI)?
What is the definition of Stress Urinary Incontinence (SUI)?
Which of the following factors can provoke or aggravate incontinence? (Select all that apply)
Which of the following factors can provoke or aggravate incontinence? (Select all that apply)
What are the three types of treatment for stress incontinence?
What are the three types of treatment for stress incontinence?
The ______ method aims to strengthen: pubococcygeus, gluteal, anal, and abdominal muscles.
The ______ method aims to strengthen: pubococcygeus, gluteal, anal, and abdominal muscles.
Match the following terms with their descriptions:
Match the following terms with their descriptions:
What are the various therapeutic modalities and exercise regimens utilized by physical therapists in the management & treatment of stress urinary incontinence?
What are the various therapeutic modalities and exercise regimens utilized by physical therapists in the management & treatment of stress urinary incontinence?
What muscles have a supportive function for the pelvic/ abdominal organs, elevate the pelvic floor, and resist increases in intra-abdominal pressure?
What muscles have a supportive function for the pelvic/ abdominal organs, elevate the pelvic floor, and resist increases in intra-abdominal pressure?
What does SUI stand for?
What does SUI stand for?
Stress Urinary Incontinence is caused by weakness of the pelvic floor muscles.
Stress Urinary Incontinence is caused by weakness of the pelvic floor muscles.
What are the etiologies of SUI? (Select all that apply)
What are the etiologies of SUI? (Select all that apply)
Which of these factors can provoke or aggravate incontinence? (Select all that apply)
Which of these factors can provoke or aggravate incontinence? (Select all that apply)
What is the degree of incontinence when it is only with mild stress such as standing, the patient is continent in the supine lying position?
What is the degree of incontinence when it is only with mild stress such as standing, the patient is continent in the supine lying position?
What are the 3 types of treatment for stress incontinence?
What are the 3 types of treatment for stress incontinence?
What is the goal of the PT treatment for stress incontinence?
What is the goal of the PT treatment for stress incontinence?
What are the types of PT treatment for stress incontinence (Select all that apply)?
What are the types of PT treatment for stress incontinence (Select all that apply)?
Explain the prophylactic treatment of PT?
Explain the prophylactic treatment of PT?
What is one thing to avoid during the first stage of labor to prevent stress incontinence?
What is one thing to avoid during the first stage of labor to prevent stress incontinence?
What is the recommended number of repetitions for PFMs exercises per day?
What is the recommended number of repetitions for PFMs exercises per day?
What are the steps of PFMs exercises?
What are the steps of PFMs exercises?
What is one of the possible benefits of strength training for PFMs?
What is one of the possible benefits of strength training for PFMs?
What is another term for Interferential therapy?
What is another term for Interferential therapy?
What are the techniques of Interferential therapy? (Select all that apply)
What are the techniques of Interferential therapy? (Select all that apply)
What is the mechanism of action of Interferential therapy?
What is the mechanism of action of Interferential therapy?
What are the types of PFMs re-education? (Select all that apply)
What are the types of PFMs re-education? (Select all that apply)
What is the biofeedback technique used for PFMs re-education?
What is the biofeedback technique used for PFMs re-education?
Explain the Cyriax method.
Explain the Cyriax method.
What are the resistive exercises for PFMs? (Select all that apply)
What are the resistive exercises for PFMs? (Select all that apply)
What is the name of the device that is worn during the specific stressful activity such as jogging, volley ball, or tennis to eliminate SUI by preventing urethral hyper-mobility through supporting the proximal urethra?
What is the name of the device that is worn during the specific stressful activity such as jogging, volley ball, or tennis to eliminate SUI by preventing urethral hyper-mobility through supporting the proximal urethra?
What is the name of the device that acts as a barrier to the loss of urine?
What is the name of the device that acts as a barrier to the loss of urine?
What device fits over external meatus rather than within the urethra and may cause urethral prolapse?
What device fits over external meatus rather than within the urethra and may cause urethral prolapse?
Magnetic Stimulation (MS) is a new approach used to treat stress incontinence.
Magnetic Stimulation (MS) is a new approach used to treat stress incontinence.
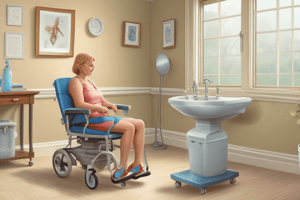
What is the key component of the MS treatment?
What is the key component of the MS treatment?
Flashcards
Stress Urinary Incontinence (SUI)
Stress Urinary Incontinence (SUI)
Involuntary leakage of urine triggered by increased intra-abdominal pressure, like coughing or laughing, in the absence of detrusor muscle contraction.
Pelvic Floor Muscles
Pelvic Floor Muscles
Muscle group supporting pelvic organs, including the bladder and vagina. They help control urination and childbirth.
Levator Ani Muscles
Levator Ani Muscles
Part of the pelvic floor, critical for supporting pelvic organs and controlling urination and bowel movements
Sphincteric Function of Pelvic Floor Muscles
Sphincteric Function of Pelvic Floor Muscles
Signup and view all the flashcards
Symptom of SUI
Symptom of SUI
Signup and view all the flashcards
Causes of SUI (Congenital)
Causes of SUI (Congenital)
Signup and view all the flashcards
Causes of SUI (Traumatic)
Causes of SUI (Traumatic)
Signup and view all the flashcards
Causes of SUI (Hormonal)
Causes of SUI (Hormonal)
Signup and view all the flashcards
Diagnosis of SUI (History)
Diagnosis of SUI (History)
Signup and view all the flashcards
Diagnosis of SUI (Tests)
Diagnosis of SUI (Tests)
Signup and view all the flashcards
Antenatal Care
Antenatal Care
Signup and view all the flashcards
Antenatal Period
Antenatal Period
Signup and view all the flashcards
Antenatal Education
Antenatal Education
Signup and view all the flashcards
Antenatal Care Team
Antenatal Care Team
Signup and view all the flashcards
Medical Antenatal Care
Medical Antenatal Care
Signup and view all the flashcards
Frequency of Examinations
Frequency of Examinations
Signup and view all the flashcards
Obstetric Examination
Obstetric Examination
Signup and view all the flashcards
Fetal Lie
Fetal Lie
Signup and view all the flashcards
Fetal Presentation
Fetal Presentation
Signup and view all the flashcards
Fetal Position
Fetal Position
Signup and view all the flashcards
Fetal Attitude
Fetal Attitude
Signup and view all the flashcards
Fetal Engagement
Fetal Engagement
Signup and view all the flashcards
Physical Therapy in Antenatal Care
Physical Therapy in Antenatal Care
Signup and view all the flashcards
Study Notes
Role of Physical Therapy in Stress Urinary Incontinence
- Stress urinary incontinence (SUI) is involuntary leakage of urine due to sudden increases in intra-abdominal pressure (e.g., coughing, sneezing, exercise). It occurs in the absence of detrusor muscle activity.
- Physical therapists use various modalities to manage SUI, including pelvic floor muscle training (PFMT), biofeedback, electrical stimulation, and behavioral strategies.
- Therapists provide patient education on lifestyle modifications to reduce SUI symptoms and improve quality of life.
- Interdisciplinary collaboration is crucial for comprehensive SUI care, involving physical therapists, physicians, nurses, and other healthcare professionals.
- The effectiveness of physical therapy interventions is assessed through research studies, clinical trials, and outcome measures focusing on patient satisfaction, symptom improvement, and functional status.
Anatomy of Pelvic Floor Muscles
- Diagrams and descriptions of the puborectalis, pubococcygeus, and coccygeus muscles are presented.
- These muscles are crucial for pelvic floor support and continence.
Anatomy of the Pelvic Floor
- Diagrams illustrate the pelvic floor, depicting the pelvic bones, bladder, uterus, vagina, urethra, rectum, and coccyx.
- The pelvic floor muscles are shown as supporting structures within this region.
Anatomy of Levator Ani Muscles
- Diagrams portray the pelvic floor muscles' structure, identifying parts of the levator ani group like the puborectalis, pubococcygeus, and iliococcygeus.
- These muscles are crucial for pelvic floor support.
Function of Levator Ani Muscles
- The levator ani muscles support the pelvic/abdominal organs by elevating the pelvic floor and resisting increases in intra-abdominal pressure.
- These muscles act as sphincters, relaxing and contracting to control urethral, vaginal, and rectal openings.
- In the birthing process, the muscles assist with the internal rotation of the fetal head during the second stage of labor.
Definition of Stress Urinary Incontinence (SUI)
- SUI is characterized by involuntary leakage of urine that usually happens with a sudden rise in intra-abdominal pressure, such as coughing, laughing, or physical activity.
- This leakage occurs in the absence of bladder contractions intended to expel urine.
Strong and Weak Pelvic Floor Muscles
- Diagrams illustrate the differences between strong and weak pelvic floor muscles' effect on the bladder neck and urethral sphincter.
- Weak muscles are associated with SUI.
Pathophysiology of SUI
- SUI occurs if the pelvic floor muscles weaken. The pelvic floor "sags" allowing the bladder neck to prolapse through a weakening pelvic floor.
- A lack of contraction of the pelvic floor during increases in intra-abdominal pressure results in the urethra failing to tighten, allowing urine to leak.
- The diagrams illustrate this process.
Etiology of SUI
- Congenital SUI may be inherited, relating to defects in intrinsic vesical sphincter or in muscular support in the bladder & urethra.
- Underlying conditions like spina bifida can affect the sphincter mechanism.
Traumatic and Hormonal Causes of SUI
- Traumatic SUI occurs due to childbirth trauma weakening pelvic supporting structures.
- Hormonal changes, such as post-menopausal atrophy, or pregnancy-related changes, might contribute to SUI.
Factors Aggravating Incontinence
- Excessive body weight, chronic cough, smoking, and bladder/urethral infections can trigger or worsen incontinence.
- Caffeine and diuretic medications also aggravate symptoms.
Grades of SUI
- Grade I involves leakage only during strenuous activities like coughing & sneezing.
- Grade II relates to leakage from moderate stress, like walking stairs.
- Grade III only causes leakage from mild stress with normal function in the supine position.
Symptoms of Stress Urinary Incontinence
- The primary symptom is involuntary urine leakage during physical activity, coughing, sneezing, or changing positions from sitting or lying down
Making the Diagnosis of SUI
- Thorough patient history regarding urinary symptoms, including frequency and nocturia, is essential.
- Factors like fluid intake, food items (spicy, acidic), and recent medication use are also considered.
- A full neurological examination might be necessary in cases of acute onset.
Tests for Diagnosing SUI
- Physical exam tests include cystoscopy (bladder examination), pad weight test (assessing urine loss during activity), and voiding diaries (tracking urine leakage & intake).
- Pelvic and abdominal ultrasounds, post-void residual (PVR) testing (final urine volume), urinalysis, urinary stress tests (stand with full bladder and cough), and urodynamic studies (pressure & flow) are also used.
- X-rays with contrast are also used to view the kidneys and bladder.
Genital Prolapse
- Genital prolapse involves the descent of one or more genital organs, such as the uterus, vagina, bladder, urethra, rectum, and Douglas pouch, below their normal position through the pelvic floor.
Types of Prolapse
-
Anterior Vaginal Wall Prolapse: This includes:
- Cystocele: Prolapse of the upper part of the anterior vaginal wall, which involves bladder tissue.
- Urethrocele: Prolapse of the lower part of the anterior vaginal wall, involving the urethra.
- Cysto-urethrocele: This is a combined prolapse of the anterior vaginal wall, involving both the bladder and urethra.
-
Posterior Vaginal Wall Prolapse: This includes:
- Rectocele: Prolapse of the middle portion of the posterior vaginal wall, often involving the rectum.
- Enterocele: This is a hernia of the Douglas pouch, where tissue containing loops of intestine protrudes into the posterior wall.
-
Vault Prolapse: A descent or inversion of the vaginal vault (top portion of the vagina) after a hysterectomy
-
Uterine Prolapse: Descending uterus, sometimes followed by the vagina due to either congenital weakness of the cervical ligaments (in nulliparous women) or obstetric trauma.
Degrees of Uterine Prolapse
- 1st degree: Descent of the cervix, but it doesn't extend outside the vagina.
- 2nd degree: Cervix protrudes into the vagina.
- 3rd degree: The entire uterus descends outside the vagina, a complete procidentia.
Treatment of SUI
- Three types of treatment exist for SUI:
- Behavior changes and bladder training: These include modifying fluid intake, avoiding strenuous activities, preventing constipation, and managing weight. Avoiding caffeine and spicy/acidic food can also help.
- Physical therapy: This involves PFMT, biofeedback, electrical therapies, exercises and may use resistance devices (e.g., vaginal cones, pelvic floor exercises etc).
- Surgery: This is often a last resort, involving procedures to strengthen pelvic floor support or correct prolapses structurally.
PFMs Exercises
- Graduations of exercises for PFMs include:
- Quick Flicks: Rapid contractions/relaxations (10-20 times); hold & relax for 10 seconds.
- Slow contractions: Tighten & hold muscles as hard as possible (10-20 times); hold & relax for 10 seconds.
- Sustained contractions: Tighten & hold muscles halfway (60 seconds); relax for 20 seconds
Frequency of Pelvic Floor Exercises
- Different studies recommend varying numbers of PFMs contractions (8-12-200 max).
- A method called "progression model" can achieve this. It involves repetitions, controlled speed, and short breaks.
- Initial sessions might be 2-3 times a week that get increased to 4-5 times per week
Biofeedback
- Biofeedback provides sensory and visual cues to help patients understand pelvic floor muscle activity.
- Kegel perineometers are a common example; this measures intra-vaginal pressure during contraction and relaxation of the pelvic floor.
- Other methods (e.g. EMG) use electrodes to provide sensory feedback.
Mid-Stream Urine Flow (Stop test)
- A technique involves interrupting and stopping the flow of urine during urination at set points in the process (beginning or end).
Cyriax Method
- A physical therapy technique focuses on strengthening pelvic floor, gluteal, anal, and abdominal muscles using breathing and visualization.
- Patients lie in a specific position and contract these muscles as they breathe in, visualizing the viscera rising toward the diaphragm, before relaxing and exhaling.
Resistive Exercises Using Vaginal Cones
- Vaginal cones, increasing in weight, are used as resistance for PFMs exercises.
- The patient contracts the PFMs to maintain the cone in place.
Palliative Treatments for SUI (Mechanical Devices)
- Vaginal Pessaries: Worn to address SUI from activities such as excessive exercise, and hypermobility that cause urethral issues.
- Intra-urethral inserts (urethral plugs): Acting as a barrier to help retain urine by fitting over the external urethral opening; however, such treatment has possible side effects like hematuria or bacterial cystitis.
- Fem Assist devices: A different device that fits over the external urethral meatus for support; risk of prolapse because of suction action is present.
Magnetic Stimulation
- Magnetic stimulation (MS) is a relatively new approach using a special chair that generates magnetic fields.
- The magnetic fields stimulate (and increase awareness of the function/contraction of) underlying tissues. It is often used to increase awareness of pelvic floor muscle activity.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz examines key concepts in physical therapy relating to stress urinary incontinence. It covers definitions, therapeutic modalities, and the importance of collaboration among healthcare professionals. Test your knowledge on pelvic floor muscles and treatment strategies for managing this condition.