Podcast
Questions and Answers
What process is initiated when a drug-receptor complex alters a cell's biochemical activity?
What process is initiated when a drug-receptor complex alters a cell's biochemical activity?
- Ion channel blocking
- Receptor desensitization
- Enzyme inhibition
- Signal transduction (correct)
If a drug binds to a receptor and activates it, initiating a series of reactions resulting in an intracellular response, it is termed what?
If a drug binds to a receptor and activates it, initiating a series of reactions resulting in an intracellular response, it is termed what?
- An enzyme
- An antagonist
- An agonist (correct)
- A ligand
The magnitude of a cellular response is proportional to what?
The magnitude of a cellular response is proportional to what?
- The number of drug-receptor complexes (correct)
- The number of available receptors on the cell surface
- The concentration of the drug in the bloodstream
- The rate of drug metabolism in the liver
Receptors exist in at least two states, inactive (R) and active (R*), that are in reversible equilibrium with one another, usually favoring which state?
Receptors exist in at least two states, inactive (R) and active (R*), that are in reversible equilibrium with one another, usually favoring which state?
Which type of drug stabilizes the fraction of inactive receptors (R) without increasing the fraction of active receptors (R*)?
Which type of drug stabilizes the fraction of inactive receptors (R) without increasing the fraction of active receptors (R*)?
Which receptor family involves a ligand-binding site that regulates the shape of a pore through which ions can flow across cell membranes?
Which receptor family involves a ligand-binding site that regulates the shape of a pore through which ions can flow across cell membranes?
Which of the following receptor families is known to directly influence DNA transcription?
Which of the following receptor families is known to directly influence DNA transcription?
Which of the following is a common effect of stimulating G protein-coupled receptors?
Which of the following is a common effect of stimulating G protein-coupled receptors?
Which type of receptor, upon activation, directly phosphorylates tyrosine residues on itself and other proteins?
Which type of receptor, upon activation, directly phosphorylates tyrosine residues on itself and other proteins?
Compared to the original agonist-receptor complex, about how long do activated G proteins persist?
Compared to the original agonist-receptor complex, about how long do activated G proteins persist?
What is tachyphylaxis in the context of drug-receptor interactions?
What is tachyphylaxis in the context of drug-receptor interactions?
What is the term for the phenomenon where repeated exposure to an antagonist results in an increase in receptor number?
What is the term for the phenomenon where repeated exposure to an antagonist results in an increase in receptor number?
What two important characteristics of a drug can be determined by graded dose-response curves?
What two important characteristics of a drug can be determined by graded dose-response curves?
In a graded dose-response curve, what does the EC50 represent?
In a graded dose-response curve, what does the EC50 represent?
Why is efficacy often considered a more clinically useful characteristic than potency?
Why is efficacy often considered a more clinically useful characteristic than potency?
What is the intrinsic activity of a full agonist?
What is the intrinsic activity of a full agonist?
How does a partial agonist behave when a receptor is already saturated with a full agonist?
How does a partial agonist behave when a receptor is already saturated with a full agonist?
What distinguishes inverse agonists from antagonists?
What distinguishes inverse agonists from antagonists?
How does a competitive antagonist affect the agonist dose-response curve?
How does a competitive antagonist affect the agonist dose-response curve?
What is the primary difference between competitive and noncompetitive antagonists?
What is the primary difference between competitive and noncompetitive antagonists?
How does an irreversible antagonist affect the Emax of an agonist?
How does an irreversible antagonist affect the Emax of an agonist?
What is functional antagonism (also known as physiologic antagonism)?
What is functional antagonism (also known as physiologic antagonism)?
In a quantal dose-response curve, what does the ED50 represent?
In a quantal dose-response curve, what does the ED50 represent?
What is the therapeutic index (TI)?
What is the therapeutic index (TI)?
What does a large therapeutic index indicate?
What does a large therapeutic index indicate?
Why is the therapeutic index particularly important for drugs like warfarin?
Why is the therapeutic index particularly important for drugs like warfarin?
Which of the following drug characteristics relates to the magnitude of a drug's effect when interacting with a receptor?
Which of the following drug characteristics relates to the magnitude of a drug's effect when interacting with a receptor?
Which statement accurately describes the relationship between drug concentration, receptor occupancy, and pharmacologic effect?
Which statement accurately describes the relationship between drug concentration, receptor occupancy, and pharmacologic effect?
A drug that chemically neutralizes excess gastric acid to reduce stomach upset, such as an antacid, exerts effects by which mechanism?
A drug that chemically neutralizes excess gastric acid to reduce stomach upset, such as an antacid, exerts effects by which mechanism?
What cellular change is most directly promoted by agonist stimulation of the γ-aminobutyric acid (GABA) receptor?
What cellular change is most directly promoted by agonist stimulation of the γ-aminobutyric acid (GABA) receptor?
Which receptor type, when bound by insulin, triggers a cascade of protein phosphorylations, ultimately leading to increased glucose uptake by the cell?
Which receptor type, when bound by insulin, triggers a cascade of protein phosphorylations, ultimately leading to increased glucose uptake by the cell?
Regarding spare receptors, what is the functional implication of a tissue having a large proportion of spare receptors?
Regarding spare receptors, what is the functional implication of a tissue having a large proportion of spare receptors?
Which scenario exemplifies functional antagonism?
Which scenario exemplifies functional antagonism?
A researcher is studying a new drug that binds to a receptor but elicits no response on its own. However, when administered with an agonist, it diminishes the maximal effect that the agonist can produce, without altering the concentration that produces 50% of the maximal effect (EC50). What type of antagonist is this drug?
A researcher is studying a new drug that binds to a receptor but elicits no response on its own. However, when administered with an agonist, it diminishes the maximal effect that the agonist can produce, without altering the concentration that produces 50% of the maximal effect (EC50). What type of antagonist is this drug?
A pharmacologist discovers a new compound that binds to the same receptor site as the endogenous agonist but produces a weaker maximal effect, even at high concentrations. Furthermore, when this compound is administered alongside the endogenous agonist, it reduces the overall effect. Which term best describes this compound?
A pharmacologist discovers a new compound that binds to the same receptor site as the endogenous agonist but produces a weaker maximal effect, even at high concentrations. Furthermore, when this compound is administered alongside the endogenous agonist, it reduces the overall effect. Which term best describes this compound?
A drug is developed to selectively inhibit a specific subtype of G protein-coupled receptors (GPCRs) in the brain to reduce anxiety. After several weeks of treatment, patients require higher doses of the drug to achieve the same anxiolytic effect. Furthermore, imaging studies reveal an increased number of the targeted GPCRs in the patients' brains, what is the most likely mechanism responsible for these observations?
A drug is developed to selectively inhibit a specific subtype of G protein-coupled receptors (GPCRs) in the brain to reduce anxiety. After several weeks of treatment, patients require higher doses of the drug to achieve the same anxiolytic effect. Furthermore, imaging studies reveal an increased number of the targeted GPCRs in the patients' brains, what is the most likely mechanism responsible for these observations?
A clinical trial is conducted to evaluate a novel antihypertensive drug. The researchers observe that the drug lowers blood pressure in 50% of the patients at a dose of 10 mg, whereas a dose of 50 mg causes severe hypotension in 50% of the patients. Based on this information, what is the therapeutic index (TI) of this drug?
A clinical trial is conducted to evaluate a novel antihypertensive drug. The researchers observe that the drug lowers blood pressure in 50% of the patients at a dose of 10 mg, whereas a dose of 50 mg causes severe hypotension in 50% of the patients. Based on this information, what is the therapeutic index (TI) of this drug?
A research team is investigating a new drug that is hypothesized to act as an inverse agonist on a constitutively active receptor. What would be the expected effect of this drug on receptor activity and downstream signaling?
A research team is investigating a new drug that is hypothesized to act as an inverse agonist on a constitutively active receptor. What would be the expected effect of this drug on receptor activity and downstream signaling?
A patient is administered a muscarinic receptor agonist to treat postoperative ileus (reduced bowel motility). However, the patient experiences significant bradycardia (slowed heart rate) as an unintended side effect. Which of the following strategies would be most effective in selectively blocking the muscarinic receptors in the heart without affecting those in the gastrointestinal tract?
A patient is administered a muscarinic receptor agonist to treat postoperative ileus (reduced bowel motility). However, the patient experiences significant bradycardia (slowed heart rate) as an unintended side effect. Which of the following strategies would be most effective in selectively blocking the muscarinic receptors in the heart without affecting those in the gastrointestinal tract?
What is the term for the specialized target macromolecules on or within cells that drugs interact with to exert their effects?
What is the term for the specialized target macromolecules on or within cells that drugs interact with to exert their effects?
Which of the following best describes signal transduction?
Which of the following best describes signal transduction?
If a drug binds to a receptor and triggers a series of reactions within the cell, leading to a specific response, what term is used to describe it?
If a drug binds to a receptor and triggers a series of reactions within the cell, leading to a specific response, what term is used to describe it?
Which of the following molecules are NOT membrane-bound proteins that transduce extracellular signals into intracellular responses and act as rich sources of receptors?
Which of the following molecules are NOT membrane-bound proteins that transduce extracellular signals into intracellular responses and act as rich sources of receptors?
What determines a drug's ability to fully or partially activate receptors?
What determines a drug's ability to fully or partially activate receptors?
Which type of ligand typically interacts with intracellular receptors?
Which type of ligand typically interacts with intracellular receptors?
How does stimulation of the nicotinic receptor by acetylcholine affect ion flow across the cell membrane?
How does stimulation of the nicotinic receptor by acetylcholine affect ion flow across the cell membrane?
Which of the following is a direct effect of Gq activation?
Which of the following is a direct effect of Gq activation?
After binding to its receptor, insulin increases glucose uptake in cells by what mechanism?
After binding to its receptor, insulin increases glucose uptake in cells by what mechanism?
What is the function of transcription factors after being activated by a ligand-receptor complex?
What is the function of transcription factors after being activated by a ligand-receptor complex?
What is the term for the phenomenon where receptors become unresponsive due to continuous exposure to an agonist, often due to phosphorylation?
What is the term for the phenomenon where receptors become unresponsive due to continuous exposure to an agonist, often due to phosphorylation?
In the context of drug administration, what does the rate of drug absorption, distribution, metabolism, and elimination collectively determine?
In the context of drug administration, what does the rate of drug absorption, distribution, metabolism, and elimination collectively determine?
Which parameter is commonly used to quantify the potency of a drug?
Which parameter is commonly used to quantify the potency of a drug?
What is the Emax of an antagonist?
What is the Emax of an antagonist?
How does a partial agonist behave when administered to a receptor already saturated with a full agonist?
How does a partial agonist behave when administered to a receptor already saturated with a full agonist?
What distinguishes inverse agonists from antagonists in terms of receptor activity?
What distinguishes inverse agonists from antagonists in terms of receptor activity?
Which of the following is characteristic of a competitive antagonist?
Which of the following is characteristic of a competitive antagonist?
What effect does an irreversible antagonist have on the Emax of an agonist?
What effect does an irreversible antagonist have on the Emax of an agonist?
Epinephrine causing bronchodilation by acting on β2-adrenoceptors while histamine causes bronchoconstriction by acting on H1 receptors is an example of what?
Epinephrine causing bronchodilation by acting on β2-adrenoceptors while histamine causes bronchoconstriction by acting on H1 receptors is an example of what?
A drug has a TD50 of 100 mg/kg and an ED50 of 10 mg/kg. What is its therapeutic index?
A drug has a TD50 of 100 mg/kg and an ED50 of 10 mg/kg. What is its therapeutic index?
Why is the therapeutic index (TI) an important consideration in drug development?
Why is the therapeutic index (TI) an important consideration in drug development?
For a drug like penicillin with a large therapeutic index, what is a common and safe practice regarding dosing?
For a drug like penicillin with a large therapeutic index, what is a common and safe practice regarding dosing?
Drug X binds to a receptor subtype that is constitutively active, leading to a basal level of signaling even in the absence of an agonist. Compound Y, when administered, decreases the basal level of activity of this receptor subtype. Which best describes Compound Y?
Drug X binds to a receptor subtype that is constitutively active, leading to a basal level of signaling even in the absence of an agonist. Compound Y, when administered, decreases the basal level of activity of this receptor subtype. Which best describes Compound Y?
A researcher is studying a new drug, “NeuromodX”, intended to enhance cognitive function by acting on a specific receptor in the brain. In preclinical trials, they observe that as they increase the concentration of NeuromodX, the cognitive enhancement plateaus, and giving higher doses does not result in any further improvement in cognitive function, even though the drug occupies all available receptors. Based on these observations, which of the following characteristics of NeuromodX can be inferred?
A researcher is studying a new drug, “NeuromodX”, intended to enhance cognitive function by acting on a specific receptor in the brain. In preclinical trials, they observe that as they increase the concentration of NeuromodX, the cognitive enhancement plateaus, and giving higher doses does not result in any further improvement in cognitive function, even though the drug occupies all available receptors. Based on these observations, which of the following characteristics of NeuromodX can be inferred?
Flashcards
Pharmacodynamics
Pharmacodynamics
Describes the actions of a drug on the body and the influence of drug concentrations on the magnitude of the response.
Receptors
Receptors
Specialized target macromolecules on the cell surface or within the cell that drugs interact with to exert their effects.
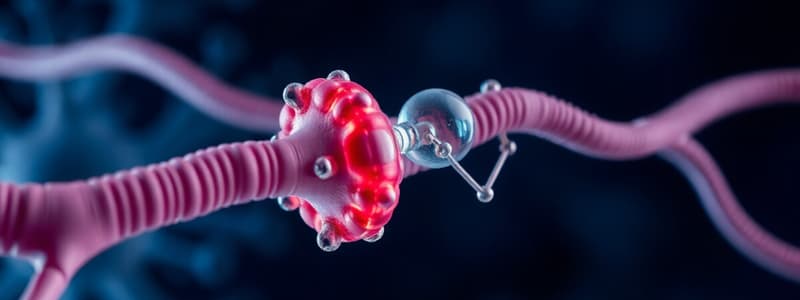
Signal Transduction
Signal Transduction
The process by which a drug-receptor complex initiates alterations in the biochemical and/or molecular activity of a cell.
Agonist
Agonist
Signup and view all the flashcards
Second Messenger
Second Messenger
Signup and view all the flashcards
Receptor States
Receptor States
Signup and view all the flashcards
Antagonists
Antagonists
Signup and view all the flashcards
Partial Agonists
Partial Agonists
Signup and view all the flashcards
Membrane Bound Receptors
Membrane Bound Receptors
Signup and view all the flashcards
Ligand-Gated Ion Channels
Ligand-Gated Ion Channels
Signup and view all the flashcards
G Protein-Coupled Receptors
G Protein-Coupled Receptors
Signup and view all the flashcards
Enzyme-Linked Receptors
Enzyme-Linked Receptors
Signup and view all the flashcards
Intracellular Receptors
Intracellular Receptors
Signup and view all the flashcards
Signal Transduction Characteristics
Signal Transduction Characteristics
Signup and view all the flashcards
Signal Amplification
Signal Amplification
Signup and view all the flashcards
Desensitization and Down-Regulation
Desensitization and Down-Regulation
Signup and view all the flashcards
Tachyphylaxis
Tachyphylaxis
Signup and view all the flashcards
Down-Regulation
Down-Regulation
Signup and view all the flashcards
Up-Regulation of Receptors
Up-Regulation of Receptors
Signup and view all the flashcards
Dose-Response Relationship
Dose-Response Relationship
Signup and view all the flashcards
Graded Dose-Response Relationship
Graded Dose-Response Relationship
Signup and view all the flashcards
Potency
Potency
Signup and view all the flashcards
EC50
EC50
Signup and view all the flashcards
Efficacy
Efficacy
Signup and view all the flashcards
Intrinsic Activity
Intrinsic Activity
Signup and view all the flashcards
Full Agonists
Full Agonists
Signup and view all the flashcards
Partial Agonists
Partial Agonists
Signup and view all the flashcards
Inverse Agonists
Inverse Agonists
Signup and view all the flashcards
Antagonists
Antagonists
Signup and view all the flashcards
Competitive antagonists
Competitive antagonists
Signup and view all the flashcards
Irreversible antagonists
Irreversible antagonists
Signup and view all the flashcards
Allosteric antagonists
Allosteric antagonists
Signup and view all the flashcards
Functional antagonism
Functional antagonism
Signup and view all the flashcards
Quantal Dose-Response Curve
Quantal Dose-Response Curve
Signup and view all the flashcards
ED50 (Quantal)
ED50 (Quantal)
Signup and view all the flashcards
TD50
TD50
Signup and view all the flashcards
Therapeutic Index
Therapeutic Index
Signup and view all the flashcards
Study Notes
- Pharmacodynamics describes drug actions on the body and how drug concentrations influence the response magnitude.
- Most drugs interact with receptors, specialized target macromolecules on or within cells, to exert beneficial and harmful effects.
- The drug-receptor complex initiates alterations in a cell's biochemical or molecular activity through signal transduction.
Signal Transduction
- Drugs act as signals, and receptors act as signal detectors.
- An agonist binds to a receptor protein site and activates it, initiating a series of reactions resulting in a specific intracellular response.
- Second messenger or effector molecules are part of the cascade translating agonist binding into a cellular response.
The Drug-Receptor Complex
- Cells contain various receptors, each specific to a particular agonist and producing a unique response.
- Cardiac cell membranes contain β-adrenergic receptors for epinephrine or norepinephrine and muscarinic receptors for acetylcholine.
- These receptors interact dynamically to control heart functions with the magnitude of the cellular response proportional to the number of drug-receptor complexes.
- Not all drugs exert effects by interacting with a receptor, antacids neutralize excess gastric acid chemically.
Receptor States
- Receptors exist in inactive (R) and active (R*) states in reversible equilibrium, usually favoring the inactive state.
- Agonists shift the equilibrium from R to R* to produce a biologic effect.
- Antagonists bind to the receptor but do not increase the fraction of R*, instead, they stabilize the fraction of R.
- Partial agonists shift the equilibrium from R to R*, but the fraction of R* is less than that caused by an agonist.
- The magnitude of biological effect is directly related to the fraction of R*.
- Agonists, antagonists, and partial agonists bind to the activation site on the receptor and can affect the fraction of R*.
Major Receptor Families
- A receptor is any biologic molecule a drug binds to and produces a measurable response.
- Enzymes, nucleic acids, and structural proteins can act as receptors.
- Membrane-bound proteins transduce extracellular signals into intracellular responses.
- Receptors are divided into four families: ligand-gated ion channels, G protein-coupled receptors, enzyme-linked receptors, and intracellular receptors.
- Hydrophilic ligands interact with receptors on the cell surface, while hydrophobic ligands interact with receptors inside cells.
Transmembrane Ligand-Gated Ion Channels
- The extracellular portion contains the ligand-binding site, regulating the pore shape for ion flow across cell membranes.
- The channel is usually closed until activated by an agonist, opening briefly for a few milliseconds.
- These receptors mediate neurotransmission and cardiac or muscle contraction.
- Nicotinic receptor stimulation by acetylcholine results in sodium influx and potassium outflux, generating an action potential.
- Agonist stimulation of the γ-aminobutyric acid (GABA) receptor increases chloride influx and hyperpolarization of neurons.
- Voltage-gated ion channels also possess ligand-binding sites that can regulate channel function.
- Local anesthetics bind to the voltage-gated sodium channel, inhibiting sodium influx and decreasing neuronal conduction.
Transmembrane G Protein–Coupled Receptors
- The extracellular domain contains the ligand-binding area, and the intracellular domain interacts with a G protein or effector molecule when activated.
- G proteins (Gs, Gi, and Gq) are composed of three protein subunits.
- The α subunit binds guanosine triphosphate (GTP), and the β and γ subunits anchor the G protein in the cell membrane.
- Agonist binding increases GTP binding to the α subunit, causing dissociation of the α-GTP complex from the βγ complex.
- These complexes interact with cellular effectors, enzymes, proteins, or ion channels, for further actions within the cell lasting seconds to minutes.
- Activated effectors produce second messengers, causing a signal cascade effect.
- Adenylyl cyclase, activated by Gs and inhibited by Gi, produces cyclic adenosine monophosphate (cAMP).
- Gq activates phospholipase C, generating inositol 1,4,5-trisphosphate (IP3) and diacylglycerol (DAG).
- DAG and cAMP activate different protein kinases, leading to physiological effects.
- IP3 regulates intracellular free calcium concentrations and some protein kinases.
Enzyme-Linked Receptors
- These receptors form dimers or multisubunit complexes.
- When activated, receptors undergo conformational changes resulting in increased cytosolic enzyme activity.
- The response lasts minutes to hours.
- Common enzyme-linked receptors possess tyrosine kinase activity.
- The activated receptor phosphorylates tyrosine residues on itself and other specific proteins, modifying their structure.
- Insulin binding to receptor subunits causes autophosphorylation of the receptor, which then phosphorylates other peptides or proteins, activating cellular signals.
Intracellular Receptors
- Receptors are entirely intracellular, requiring ligands to diffuse into the cell.
- Ligands must have sufficient lipid solubility.
- Primary targets are transcription factors in the cell nucleus.
- Ligand binding activates the receptor via dissociation from binding proteins.
- The ligand–receptor complex translocates to the nucleus, dimerizes, and binds to transcription factors, regulating gene expression.
- Intracellular receptors take hours to days.
- Steroid hormones exert their action on target cells via intracellular receptors.
- Other targets of intracellular ligands include structural proteins, enzymes, RNA, and ribosomes.
- Tubulin is the target of antineoplastic agents (paclitaxel), dihydrofolate reductase is the target of antimicrobials (trimethoprim), and the 50S subunit of the bacterial ribosome is the target of macrolide antibiotics (erythromycin).
Characteristics of Signal Transduction
- Signal transduction has two important features including, the ability to amplify small signals and mechanisms to protect the cell from excessive stimulation.
Signal Amplification
- G protein-linked and enzyme-linked receptors amplify signal intensity and duration via the signal cascade effect.
- Activated G proteins persist longer than the original agonist-receptor complex.
- The binding of albuterol may only exist for milliseconds, but the subsequent activated G proteins may last for hundreds of milliseconds.
- Amplification is mediated by the interaction between G proteins and their respective intracellular targets.
- Only a fraction of the total receptors for a specific ligand may need to be occupied to elicit a maximal response because of this amplification.
- Systems exhibiting this behavior are said to have spare receptors.
- About 99% of insulin receptors are "spare” ensuring that adequate amounts of glucose enter the cell.
- About 5% to 10% of the total B3-adrenoceptors in the heart are spare, with little functional reserve in the failing heart.
Desensitization and Down-Regulation of Receptors
- Repeated or continuous administration of an agonist or antagonist often leads to changes in the responsiveness of the receptor.
- The receptor may become desensitized due to too much agonist stimulation, resulting in a diminished response which is called tachyphylaxis.
- Desensitization is often due to phosphorylation and renders receptors unresponsive to the agonist.
- Receptors may be internalized within the cell, making them unavailable for further agonist interaction (down-regulation).
- Some receptors, particularly ion channels, require a finite time following stimulation before they can be activated again.
- During this recovery phase, unresponsive receptors are said to be "refractory."
- Repeated exposure of a receptor to an antagonist results in up-regulation of receptors.
- Up-regulation makes cells more sensitive to agonists and/or more resistant to effects of the antagonist.
Dose-Response Relationship
- Agonist drugs mimic the action of the endogenous ligand for the receptor.
- The magnitude of the drug effect depends on receptor sensitivity to the drug and the drug concentration at the receptor site.
- Drug concentration is determined by the dose of drug administered and by the drug's pharmacokinetic profile.
Graded Dose-Response Relationship
- As the concentration of a drug increases, its pharmacologic effect gradually increases until all the receptors are occupied.
- Plotting the magnitude of response against increasing doses of a drug produces a graded dose-response curve.
- Potency and efficacy can be determined by graded dose-response curves.
Potency
- Potency is a measure of the amount of drug necessary to produce an effect.
- The concentration of drug producing 50% of the maximum effect (EC50) is often used to determine potency.
- A lower EC50 indicates higher potency.
- Semilogarithmic plots are used to graph the complete range of doses.
Efficacy
- Efficacy is the magnitude of response a drug causes when it interacts with a receptor.
- Efficacy is dependent on the number of drug receptor complexes formed and the intrinsic activity of the drug.
- Maximal efficacy of a drug (Emax) assumes that the drug occupies all receptors.
- The maximal response differs between full and partial agonists, even when the drug occupies 100% of the receptors.
- Even though an antagonist occupies 100% of the receptor sites, no receptor activation results and Emax is zero.
- Efficacy is a more clinically useful characteristic than potency, since a drug with greater efficacy is more therapeutically beneficial than one that is more potent.
Intrinsic Activity
- Intrinsic activity determines its ability to fully or partially activate the receptors.
- Drugs may be categorized according to their intrinsic activity and resulting Emax values.
Full Agonists
- A full agonist binds to a receptor and produces a maximal biologic response that mimics the response to the endogenous ligand.
- Full agonists stabilize the receptor in its active state and have an intrinsic activity of one.
- All full agonists for a receptor population should produce the same Emax.
Partial Agonists
- Partial agonists have intrinsic activities greater than zero but less than one.
- Partial agonists cannot produce the same Emax as a full agonist even when all the receptors are occupied.
- A partial agonist may have an affinity that is greater than, less than, or equivalent to that of a full agonist.
- When a receptor is exposed to both a partial agonist and a full agonist, the partial agonist may act as an antagonist of the full agonist.
- The Emax of a receptor saturated with an agonist in the presence of increasing concentrations of a partial agonist would decrease until it reached the Emax of the partial agonist.
- Partial agonists can act as both an agonist and antagonist
- Aripiprazole has the ability to improve symptoms of schizophrenia, with a small risk of causing extrapyramidal adverse effects.
Inverse Agonists
- Some receptors show a spontaneous conversion from R to R* in the absence of an agonist.
- Inverse agonists stabilize the inactive R form and cause R* to convert to R.
- Inverse agonists decrease the number of activated receptors to below that observed in the absence of drug.
- Inverse agonists have an intrinsic activity less than zero, reverse the activity of receptors, and exert the opposite pharmacological effect of agonists.
Antagonists
- Antagonists bind to a receptor with high affinity but possess zero intrinsic activity.
- An antagonist has no effect on biological function in the absence of an agonist, but can decrease the effect of an agonist when present.
- Antagonism may occur either by blocking the drug's ability to bind to the receptor or by blocking its ability to activate the receptor.
Competitive Antagonists
- A competitive antagonist binds to the same site on the receptor as the agonist in a reversible manner.
- A competitive antagonist interferes with an agonist binding to its receptor and maintains the receptor in its inactive state.
- Increasing the concentration of agonist relative to antagonist can overcome this inhibition.
- Competitive antagonists shift the agonist dose-response curve to the right (increased EC50) without affecting Emax.
Irreversible Antagonists
- Irreversible antagonists bind covalently to the active site of the receptor.
- Reducing permanently reduces the number of receptors available to the agonist.
- An irreversible antagonist causes a downward shift of the Emax with no shift of EC50 values.
- Addition of more agonist does not overcome the effect of irreversible antagonists.
- Irreversible antagonists and allosteric antagonists are both considered noncompetitive antagonists.
- Competitive antagonists reduce agonist potency (increase EC50) and noncompetitive antagonists reduce agonist efficacy (decrease Emax).
Allosteric Antagonists
- An allosteric antagonist binds to a site (allosteric site) other than the agonist-binding site.
- An allosteric antagonist prevents receptor activation by the agonist.
- It causes a downward shift of the Emax of an agonist, with no change in the EC50 value.
- Picrotoxin binds to the inside of the GABA-controlled chloride channel so no chloride can pass through the channel, even when GABA fully occupies the receptor.
Functional Antagonism
- An antagonist may act at a completely separate receptor, initiating effects that are functionally opposite those of the agonist.
- Epinephrine causes functional antagonism to histamine-induced bronchoconstriction.
- Histamine binds to H1 histamine receptors on bronchial smooth muscle, causing bronchoconstriction of the bronchial tree.
- Epinephrine is an agonist at B2-adrenoceptors on bronchial smooth muscle, which causes the muscles to relax.
- Functional antagonism is also known as "physiologic antagonism."
Quantal Dose-Response Curve
- This is the relationship between the dose of the drug and the proportion of a population of patients that responds to it.
- Quantal responses, because, for any individual, either the effect occurs or it does not.
- Graded responses can be transformed to quantal responses.
- Quantal dose-response curves are useful for determining doses to which most of the population responds.
- The ED50 is the drug dose that causes a therapeutic response in half of the population.
Therapeutic Index
- The therapeutic index (TI) of a drug is the ratio of the dose that produces toxicity in half the population (TD50) to the dose that produces a clinically desired or effective response (ED50) in half the population: TI = TD50/ED50
- The Tl is a measure of a drug's safety with a larger value indicates a wide margin between doses that are effective and doses that are toxic.
Clinical Usefulness of the Therapeutic Index
- The Tl of a drug is determined using drug trials and accumulated clinical experience.
- These reveal a range of effective doses and a different (sometimes overlapping) range of toxic doses.
- Although high Tl values are required for most drugs, some drugs with low therapeutic indices are routinely used to treat serious diseases.
- The responses to warfarin, an oral anticoagulant with a low TI, and penicillin, an antimicrobial drug with a large Tl.
Warfarin
- As the dose of warfarin is increased, a greater fraction of the patients responds (for this drug, the desired response is a two- to threefold increase in the international normalized ratio [INR]) until, eventually, all patients respond.
- At higher doses of warfarin, anticoagulation resulting in hemorrhage occurs in a small percent of patients.
- Agents with a low Tl are those drugs for which dose is critically important with bioavailability critically alters the therapeutic effects.
Penicillin
- For drugs such as penicillin, it is safe and common to give doses in excess of that which is minimally required to achieve a desired response without the risk of adverse effects.
- Bioavailability does not critically alter the therapeutic or clinical effects.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.