Podcast
Questions and Answers
What is the primary structure of hemoglobin?
What is the primary structure of hemoglobin?
- The arrangement of chains in helices and non-helices
- The amino acid sequence of the polypeptide chains (correct)
- The pocket for heme formed by the globin chains
- The overall three-dimensional shape of the molecule
What causes hemoglobin to lose its ability to bind oxygen?
What causes hemoglobin to lose its ability to bind oxygen?
- Association with carbon dioxide molecules
- Reduction of ferrous iron to ferrous state
- Exposure to high temperatures
- Oxidation of ferrous iron to ferric state (correct)
Which of the following best describes the structure of heme?
Which of the following best describes the structure of heme?
- A non-helical segment connecting helices
- A linear chain of amino acids
- A ring of carbon, hydrogen, and nitrogen with a central iron atom (correct)
- A globular protein with multiple subunits
What changes to the amino acid sequences of the globin chains can result in?
What changes to the amino acid sequences of the globin chains can result in?
What is the significance of the pocket in the hemoglobin molecule?
What is the significance of the pocket in the hemoglobin molecule?
How many heme groups are present in a single hemoglobin molecule?
How many heme groups are present in a single hemoglobin molecule?
What kind of protein is hemoglobin classified as?
What kind of protein is hemoglobin classified as?
Which part of the hemoglobin structure is described as relatively rigid and linear?
Which part of the hemoglobin structure is described as relatively rigid and linear?
What is characteristic of macrocytes?
What is characteristic of macrocytes?
Which condition is associated with microcytes?
Which condition is associated with microcytes?
What does anisocytosis indicate?
What does anisocytosis indicate?
What causes echinocytes to form?
What causes echinocytes to form?
Which type of cells are described as having unevenly spaced projections?
Which type of cells are described as having unevenly spaced projections?
What is a common appearance of target cells?
What is a common appearance of target cells?
In which condition is anisocytosis seen?
In which condition is anisocytosis seen?
What type of anemia is characterized by a deficiency of vitamin B12 or folate?
What type of anemia is characterized by a deficiency of vitamin B12 or folate?
What is the primary function of erythropoietin in hematopoiesis?
What is the primary function of erythropoietin in hematopoiesis?
Which chromosome houses the gene for erythropoietin?
Which chromosome houses the gene for erythropoietin?
During erythroid precursor identification, what does the decreasing nuclear to cytoplasmic (N:C) ratio indicate?
During erythroid precursor identification, what does the decreasing nuclear to cytoplasmic (N:C) ratio indicate?
What is a characteristic feature of the pronormoblast stage in red blood cell maturation?
What is a characteristic feature of the pronormoblast stage in red blood cell maturation?
What overall change occurs in the cytoplasm color of red blood cells as they mature?
What overall change occurs in the cytoplasm color of red blood cells as they mature?
In normal hematopoiesis, what do you expect to observe in the chromatin pattern during cell maturation?
In normal hematopoiesis, what do you expect to observe in the chromatin pattern during cell maturation?
Which stage of red blood cell maturation has a size of up to 12 um and shows significant chromatin clumping?
Which stage of red blood cell maturation has a size of up to 12 um and shows significant chromatin clumping?
What specific characteristic defines the orthochromic normoblast stage?
What specific characteristic defines the orthochromic normoblast stage?
What percentage of hemoglobin synthesis occurs in reticulocytes?
What percentage of hemoglobin synthesis occurs in reticulocytes?
Which molecules are required for heme synthesis in the mitochondria?
Which molecules are required for heme synthesis in the mitochondria?
What is the main function of transferrin in hemoglobin synthesis?
What is the main function of transferrin in hemoglobin synthesis?
How many heme groups are attached to a complete hemoglobin molecule?
How many heme groups are attached to a complete hemoglobin molecule?
What is the role of aminolevulinate synthase in heme synthesis?
What is the role of aminolevulinate synthase in heme synthesis?
Which chromosome controls globin synthesis for alpha chains?
Which chromosome controls globin synthesis for alpha chains?
What is formed when Fe2+ combines with protoporphyrin IX in heme synthesis?
What is formed when Fe2+ combines with protoporphyrin IX in heme synthesis?
What is the molecular structure of hemoglobin?
What is the molecular structure of hemoglobin?
In which cellular location does the translation of globin mRNA to the globin polypeptide chain occur?
In which cellular location does the translation of globin mRNA to the globin polypeptide chain occur?
What is the predominant hemoglobin type at birth?
What is the predominant hemoglobin type at birth?
Which globin chain is produced by Hb F?
Which globin chain is produced by Hb F?
What happens to gamma chain production after 6 months of age?
What happens to gamma chain production after 6 months of age?
What refers to the reference range of hemoglobin types in a normal adult?
What refers to the reference range of hemoglobin types in a normal adult?
What is the role of haptoglobin in the breakdown of hemoglobin?
What is the role of haptoglobin in the breakdown of hemoglobin?
Which embryonic hemoglobin type consists of 2 zeta and 2 epsilon chains?
Which embryonic hemoglobin type consists of 2 zeta and 2 epsilon chains?
Which method can be used to test for the presence of Hb F?
Which method can be used to test for the presence of Hb F?
What is the primary indicator of bone marrow function among the options listed?
What is the primary indicator of bone marrow function among the options listed?
Which statement is true regarding the characteristics of mature erythrocytes?
Which statement is true regarding the characteristics of mature erythrocytes?
What role does erythropoietin play in erythropoiesis?
What role does erythropoietin play in erythropoiesis?
Which factor is NOT a regulator of erythropoiesis?
Which factor is NOT a regulator of erythropoiesis?
Which description best defines reticulocytes?
Which description best defines reticulocytes?
At what size do reticulocytes generally measure?
At what size do reticulocytes generally measure?
How long does hemoglobin continue to be produced by reticulocytes after exiting the bone marrow?
How long does hemoglobin continue to be produced by reticulocytes after exiting the bone marrow?
Which statement correctly describes the composition of an erythrocyte membrane?
Which statement correctly describes the composition of an erythrocyte membrane?
Flashcards
Hemoglobin Structure
Hemoglobin Structure
Hemoglobin is a protein with four heme groups, each holding an iron atom that binds oxygen.
Heme Group Structure
Heme Group Structure
A ring of carbon, hydrogen, and nitrogen atoms (protoporphyrin) with an iron atom in the center.
Globin Chains
Globin Chains
The protein chains surrounding the heme groups in hemoglobin.
Hemoglobin Function
Hemoglobin Function
Signup and view all the flashcards
Heme's Role in Color
Heme's Role in Color
Signup and view all the flashcards
Hemoglobin Polypeptide Chains
Hemoglobin Polypeptide Chains
Signup and view all the flashcards
Iron Oxidation
Iron Oxidation
Signup and view all the flashcards
Hemoglobin's Structure Levels
Hemoglobin's Structure Levels
Signup and view all the flashcards
Hemoglobin Synthesis Location
Hemoglobin Synthesis Location
Signup and view all the flashcards
Heme Synthesis Process - Step 1
Heme Synthesis Process - Step 1
Signup and view all the flashcards
Heme Synthesis Pathway - Cytoplasm
Heme Synthesis Pathway - Cytoplasm
Signup and view all the flashcards
Heme Finalization step
Heme Finalization step
Signup and view all the flashcards
Iron Transport (Transferrin)
Iron Transport (Transferrin)
Signup and view all the flashcards
Iron Release in Mitochondria
Iron Release in Mitochondria
Signup and view all the flashcards
Globin Chain Synthesis Locations
Globin Chain Synthesis Locations
Signup and view all the flashcards
Globin Synthesis Location
Globin Synthesis Location
Signup and view all the flashcards
Globin Gene Transcription
Globin Gene Transcription
Signup and view all the flashcards
Globin Translation
Globin Translation
Signup and view all the flashcards
Embryonic Hemoglobin Types
Embryonic Hemoglobin Types
Signup and view all the flashcards
Fetal Hemoglobin (Hb F) Function
Fetal Hemoglobin (Hb F) Function
Signup and view all the flashcards
Hgb A Composition
Hgb A Composition
Signup and view all the flashcards
Glycosylated Hgb A (Hb A1c)
Glycosylated Hgb A (Hb A1c)
Signup and view all the flashcards
Intravascular Hemolysis
Intravascular Hemolysis
Signup and view all the flashcards
Erythropoietin
Erythropoietin
Signup and view all the flashcards
Colony-Forming Unit-Erythrocytes (CFU-Es)
Colony-Forming Unit-Erythrocytes (CFU-Es)
Signup and view all the flashcards
How is the maturation of a red blood cell determined?
How is the maturation of a red blood cell determined?
Signup and view all the flashcards
What causes the blueness in developing red blood cells?
What causes the blueness in developing red blood cells?
Signup and view all the flashcards
What causes the pinkness in mature red blood cells?
What causes the pinkness in mature red blood cells?
Signup and view all the flashcards
Pronormoblast (Rubriblast)
Pronormoblast (Rubriblast)
Signup and view all the flashcards
Basophilic Normoblast (Prorubricyte)
Basophilic Normoblast (Prorubricyte)
Signup and view all the flashcards
Polychromatophilic Normoblast (Rubricyte)
Polychromatophilic Normoblast (Rubricyte)
Signup and view all the flashcards
What are normocytes?
What are normocytes?
Signup and view all the flashcards
What are macrocytes?
What are macrocytes?
Signup and view all the flashcards
What are microcytes?
What are microcytes?
Signup and view all the flashcards
Anisocytosis
Anisocytosis
Signup and view all the flashcards
What is poikilocytosis?
What is poikilocytosis?
Signup and view all the flashcards
What are echinocytes?
What are echinocytes?
Signup and view all the flashcards
What are acanthocytes?
What are acanthocytes?
Signup and view all the flashcards
What are target cells?
What are target cells?
Signup and view all the flashcards
Reticulocyte Count
Reticulocyte Count
Signup and view all the flashcards
Reticulocyte Size
Reticulocyte Size
Signup and view all the flashcards
Reticulocyte Hemoglobin Synthesis
Reticulocyte Hemoglobin Synthesis
Signup and view all the flashcards
Mature Red Blood Cell Size
Mature Red Blood Cell Size
Signup and view all the flashcards
Central Pallor (RBC)
Central Pallor (RBC)
Signup and view all the flashcards
Erythropoiesis Regulation
Erythropoiesis Regulation
Signup and view all the flashcards
Erythrocyte Energy Source
Erythrocyte Energy Source
Signup and view all the flashcards
Erythrocyte Membrane Composition
Erythrocyte Membrane Composition
Signup and view all the flashcards
Study Notes
Hemoglobin Metabolism
- Hemoglobin is an oxygen-transporting protein found in red blood cells (erythrocytes).
- The heme portion of hemoglobin gives red blood cells their characteristic red color.
- Hemoglobin's structure is a globular protein made of four heme groups and two different polypeptide chains.
Hemoglobin Structure
- X-ray crystallography was used to describe hemoglobin's structure for the first time.
- The molecule is a tetramer of four globin polypeptide chains, with one heme group imbedded in each chain.
- The four heme groups are positioned in a pocket of the polypeptide chain near the surface of the hemoglobin molecule.
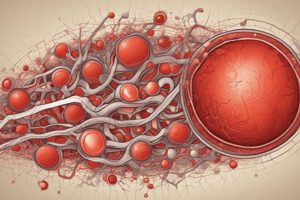
Heme Structure
- Heme consists of protoporphyrin IX, a ring of carbon, hydrogen, and nitrogen atoms, with a central divalent ferrous iron (Fe2+) atom.
- Each heme group reversibly combines with one oxygen molecule, via the ferrous iron.
- When the ferrous iron oxidizes to the ferric state (Fe3+), it can no longer bind to oxygen.
Globin Structure
- Each hemoglobin molecule consists of four globin chains (two alpha chains and two beta chains) totaling 141 to 146 amino acids each.
- Variations in amino acid sequences result in different types of polypeptide chains.
- Each globin chain is designated by a Greek letter (alpha, beta, gamma, delta, epsilon, zeta, and theta).
- Each globin chain is divided into eight helices separated by seven non-helical segments.
- Flexible nonhelical segments connect the helices.
- The iron atom of heme is linked to the F8 proximal histidine on one side of the plane and oxygen binds to the iron atom on the other side, close to the E7 distal histidine.
Hemoglobin Molecule
- Hemoglobin's primary structure is the amino acid sequence of the polypeptide chains.
- The secondary structure describes how the chains are arranged in helices and non-helices.
- Globin chains loop to form a cleft pocket for the heme group.
- Each chain has a heme group that is suspended between the E and F helices of the polypeptide chains.
- Globin chain amino acids on the outside are hydrophilic, which makes the molecule water-soluble.
- Those in the cleft are hydrophobic, helping to keep the iron in a usable divalent ferrous form, whether the hemoglobin is oxygenated or deoxygenated.
Hemoglobin Synthesis
- 65% of hemoglobin is synthesized in immature red blood cells (reticulocytes).
- The remaining 35% is synthesized in reticulocytes.
- Heme synthesis occurs in the mitochondria of normoblasts and depends on glycine, succinyl coenzyme A, aminolevulinic acid synthetase, and vitamin B6.
- Globin synthesis occurs in ribosomes and is controlled on chromosome 16 for alpha chains and chromosome 11 for all other chains.
- Each globin chain binds to a heme molecule in the immature red blood cell cytoplasm.
Heme Synthesis
- Heme synthesis starts in mitochondria with the condensation of glycine and succinyl-CoA, catalyzed by aminolevulinic acid synthetase.
- This forms aminolevulinic acid (ALA).
- In the cytoplasm, ALA dehydratase (also known as porphobilinogen synthase) converts ALA to porphobilinogen.
- Further transformations occur, including hydroxylmethylbilane and coproporphyrinogen III development.
- The process continues in the mitochondria until, in the final step, Fe2+ combines with protoporphyrin IX in the presence of ferrochelatase (heme synthase) to form heme.
Globin Synthesis
The globin chains are synthesized from the pronormoblast stage through the polychromatic erythrocyte stage in the bone marrow.
- It involves DNA transcription in the nucleus to produce mRNA, which is then translated into polypeptide chains on ribosomes in the cytoplasm.
- The chains are released into the cytoplasm once complete.
Hemoglobin Ontogeny
- The z- and ε-globin chains appear only during the first three months of embryonic development by forming the embryonic hemoglobins.
- During the second and third trimesters of fetal life, and at birth, Hb F (α2γ2) predominates.
- Hb A (α2β2) becomes the predominant hemoglobin by six months of age and continues through adulthood, with small amounts of Hb A2 (α2δ2) and Hb F persisting.
Hemoglobin Types
- Fetal hemoglobin (Hb F) has alpha and gamma chains.
- Adult hemoglobin (Hb A) has alpha and beta chains.
- Adult hemoglobin A2 (Hb A2) has alpha and delta chains.
- Embryonic hemoglobins consist of specific combinations of zeta, epsilon, and gamma chains.
Hemoglobin/Erythrocyte Breakdown
- Intravascular hemolysis occurs when hemoglobin breaks down within the blood.
- Hemoglobin is released into plasma and binds to haptoglobin.
- This complex, along with hemopexin and albumin, is phagocytized by liver macrophages.
- Extravascular hemolysis occurs when senescent RBCs are phagocytized in the liver or spleen by macrophages.
- Protoporphyrin is metabolized to bilirubin and urobilinogen.
- Globin chains are recycled.
- Iron binds to transferrin and is transported to bone marrow for new red blood cell production, or it is stored as ferritin or hemosiderin.
- Intravascular hemolysis results in elevated plasma hemoglobin, serum bilirubin, and urine urobilinogen, and decreased serum haptoglobin.
- Extravascular hemolysis results in the same consequences, but with decreased plasma hemoglobin.
Hemoglobin and Iron
- Most body iron is in hemoglobin in its ferrous state (Fe2+), necessary for oxygen transport.
- Ferric iron (Fe3+) cannot bind to hemoglobin; it binds to transferrin.
- Serum iron (SI): measures the amount of Fe3+ bound to transferrin.
- Total iron-binding capacity (TIBC): measures the total iron-binding capacity of transferrin.
- Serum ferritin: measures stored iron in tissues and bone marrow.
Different Forms of Normal Hemoglobin
- Oxyhemoglobin: Hemoglobin with Fe2+ + O2, found in arterial circulation.
- Deoxyhemoglobin: Hemoglobin with Fe2+ but no O2, found in venous circulation.
- Carboxyhemoglobin: Hemoglobin with Fe2+ and carbon monoxide (CO). CO binds to hemoglobin more strongly than O2.
- Methemoglobin: Hemoglobin with Fe3+; cannot transport oxygen and can result in cyanosis and anemia.
- Sulfhemoglobin: Hemoglobin with sulfur (S); cannot transport O2; generally not fatal but caused by drugs and chemicals.
Oxygen Dissociation Curve
- Oxygen affinity is the ability of hemoglobin to bind or release oxygen.
- Expressed as the oxygen tension at which hemoglobin is 50% saturated with oxygen.
- The relationship between oxygen tension and hemoglobin saturation is described by the oxygen dissociation curve.
- Factors like the 2,3-DPG/BPG level, body temperature, and pH influence the curve, affecting oxygen release to tissues.
Disorders Related to Hemoglobin Biosynthesis
- Inherited defects include congenital erythropoietic porphyria.
- Acquired defects include lead poisoning (inhibits heme synthesis at multiple points).
Porphyria
- A disease of heme metabolism, marked by accumulation of porphyrins or precursors in the body.
- Classifications are based on clinical presentation (acute vs. chronic), the source of enzyme deficiency, and the site of enzyme deficiency in the heme biosynthetic pathway.
- Clinically, patients experience either neurological complications or skin problems. Some patients have no symptoms.
Porphyrin Synthesis Disorders
- Inherited defects involve a rare autosomal recessive condition called congenital erythropoietic porphyria.
- Acquired defects include lead poisoning, which inhibits heme synthesis at various points leading to abnormal reactions in the heme biosynthetic pathway.
Iron Metabolism Disorders
- Genetic variations affecting iron plasma concentrations are linked to conditions like transmembrane protease serine 6.
- Associated with lower hemoglobin levels, smaller red cells, and a high red blood cell distribution width (RDW).
- Primary overload disorders result from increased iron absorption from a normal diet.
- Secondary overload can arise from conditions like chronic disorders or hemolytic anemias, and iron therapy.
- Sideroblastic anemia involves excess iron accumulation in the cytoplasm of immature erythrocytes due to the ratio between plasma iron level and the iron required by the cell.
- Causes of sideroblastic anemia include congenital defects and acquired defects, such as primary (myelodysplastic syndrome) or secondary (drug-induced, toxin-induced) causes.
Erythrocyte Production and Destruction
- General characteristics of erythrocytes: biconcave shape, presence of hemoglobin for oxygen transport, loss of nucleus during maturation, limited lifespan (120 days).
- Erythropoiesis: The process of red blood cell production, beginning with hematopoietic stem cells (HSCs), transitioning through various stages (pronormoblast, basophilic normoblast, polychromatophilic normoblast, orthochromic normoblast, reticulocyte, erythrocyte) in the bone marrow.
- Regulation of erythropoiesis: Controlled partly by actions of cytokine signaling pathways and transcription factors, predominantly erythropoietin released in the kidneys.
- Erythrocyte function: Transport oxygen and removal of metabolic wastes.
Erythrocyte Physiology
- Energy production: Early red blood cells obtain energy via oxidative phosphorylation, which is later replaced by glycolysis as mitochondria are lost during maturation.
- Volume ratio and flexibility: Erythrocytes maintain a proper volume ratio to facilitate gas exchange through capillaries. The cation pump regulates the internal potassium (K+) and external sodium (Na+) ion concentrations to maintain flexibility.
- Membrane composition: The erythrocyte membrane is composed of approximately 50-60% lipids (phospholipids, cholesterol, and glycolipids) and 40-50% proteins.
Substances needed for erythropoiesis
- Iron (Fe2+): essential for oxygen transport.
- Amino acids: necessary for globin chain synthesis.
- Folic acid/vitamin B12: crucial for DNA replication and cell division.
- Erythropoietin,
- Vitamin 65 (pyridoxine): required for certain enzymatic reactions.
- Trace minerals: important for overall function.
Abnormal RBC distribution
• Rouleaux: Stacking or "coin-stacking" of erythrocytes due to abnormal or increased plasma proteins (e.g., in hyperproteinemia, multiple myeloma, Waldenstrom macroglobulinemia, or conditions with increased fibrinogen). • Agglutination: Clumping of erythrocytes without a specific pattern, occurring when erythrocytes are coated with IgM antibodies (e.g. in cold autoimmune hemolytic anemia).
Erythrocyte Morphology and Associated Diseases
- Normocytes: Normal size and shape (discocytes) of erythrocytes equivalent to the nucleus of a small lymphocyte.
- Macrocytes: RBCs larger than 8 µm in diameter (MCV >100 fL); seen in megaloblastic anemias, liver disease, or accelerated erythropoiesis.
- Microcytes: RBCs smaller than 6 µm in diameter (MCV <80 fL); seen in iron deficiency, thalassemia, sideroblastic anemia, or chronic disease.
- Anisocytosis: Variation in RBC size (dimorphism/heterogeneity). Common after treatment or post-transfusion or when multiple deficiencies are present(e.g. iron and B12).
- Poikilocytosis: Variation in RBC shape.
- Echinocytes (crenate or burr cells): Short, evenly spaced projections on the cell surface; often seen in liver disease, uremia, heparin therapy, pyruvate kinase deficiency.
- Acanthocytes (spur cells): Irregular, unevenly spaced projections on the cell surface; often seen in alcoholic liver disease, post-splenectomy, and abetalipoproteinemia.
- Target cells (codocytes or Mexican hat cells): Increased surface-to-volume ratio; central pallor area is surrounded by a ring; seen in liver disease, some hemoglobinopathies, thalassemia, iron-deficiency anemia.
- Spherocytes: Disk-shaped but small cells without central pallor; increased osmotic fragility; seen in hereditary spherocytosis, immune hemolytic anemia, and G6PD deficiency.
- Teardrop cells (dacryocytes): Pear-shaped cells often with a single blunt projection; seen in extramedullary hematopoiesis (e.g., myelofibrosis, myelophthisic anemia).
- Helmet cells (horn cells, keratocytes, schizocytes): Fragmented RBCs with a hollow interior; seen in microangiopathic hemolytic anemias like DIC, thermal injury, prosthetic implants.
- Schistocytes (RBC fragments): Small, irregular fragments of RBCs with pointed projections; common in microangiopathic hemolytic anemias, DIC, thermal injury.
- Stomatocytes (mouth cells): Elongated, slit-like central pallor; associated with osmotic changes due to altered cation balance (Na+ /K+); seen in liver disease, acute alcoholism, conditions affecting red cell membrane integrity.
- Elliptocytes (ovalocytes): Cigar- to egg-shaped cells, representing loss of red blood cell membrane integrity; common in hereditary elliptocytosis, iron deficiency anemia, and megaloblastic anemia.
Erythrocyte Inclusions and Associated Diseases
- Nucleated RBCs (nRBCs): Presence of nuclei in immature red blood cells; often indicate increased bone marrow activity.
- Howell-Jolly bodies: Small, round, DNA fragments; normally removed by the spleen; seen in sickle cell anemia, beta-thalassemia major, or other severe hemolytic anemias, megaloblastic anemia, or post-splenectomy.
- Basophilic stippling: Multiple, evenly dispersed, tiny inclusions in the cytoplasm; represent remnants of ribosomal RNA; often seen in thalassemia, megaloblastic anemia, lead poisoning, and alcoholism.
- Pappenheimer bodies: Small, irregular, dark-staining iron granules clustered at the cell periphery; found in sideroblastic anemia, hemoglobinopathies, and myelodysplastic syndromes.
- Cabot rings: Thin, red-violet ringlike structures, often in loop or figure-eight shapes; composed of fragmented nuclear material; seen in megaloblastic anemia, lead poisoning, and myelodysplastic syndromes.
- Hemoglobin C crystals: Condensed, intracellular, rodshaped crystals; found in hemoglobin C or SC disease.
- Hemoglobin SC crystals (Washington monument): Blunt, fingerlike projections; found in hemoglobin SC disease.
- Heinz Bodies: Small, denatured hemoglobin inclusions; insoluble hemoglobin fragments; seen in G6PD deficiency, beta-thalassemia major, and drug-induced anemia.
Malarial Parasites
- Microscopically visualizable erythrocytic inclusions and changes in cytoplasm due to different species of malaria.
Abnormal RBC Distribution and Related Diseases
- Rouleaux: Stacked or "coin-like" arrangement of erythrocytes due to abnormal or increased plasma proteins.
- Agglutination: A non-specific clumping of red blood cells; associated with cold autoimmunity hemolytic anemia.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.