Podcast
Questions and Answers
What is a key factor for successful delivery of peripheral nerve blocks?
What is a key factor for successful delivery of peripheral nerve blocks?
- Patient gender
- Patient age
- Anatomical landmarks (correct)
- Patient weight
What is a relative contraindication for peripheral nerve blocks?
What is a relative contraindication for peripheral nerve blocks?
- Obesity
- Old age
- Pregnancy (correct)
- Smoking
Which nerve is commonly targeted for peripheral nerve blocks for headache disorders?
Which nerve is commonly targeted for peripheral nerve blocks for headache disorders?
- Vagus nerve
- Sciatic nerve
- Facial nerve
- Greater occipital nerve (correct)
What is a possible complication of peripheral nerve blocks?
What is a possible complication of peripheral nerve blocks?
What is a potential benefit of peripheral nerve blocks for headache disorders?
What is a potential benefit of peripheral nerve blocks for headache disorders?
What is an adverse effect of peripheral nerve blocks?
What is an adverse effect of peripheral nerve blocks?
What is a pitfall to be aware of when administering peripheral nerve blocks?
What is a pitfall to be aware of when administering peripheral nerve blocks?
What is a potential preventative effect of peripheral nerve blocks for migraine headaches?
What is a potential preventative effect of peripheral nerve blocks for migraine headaches?
What is the purpose of peripheral nerve blocks in headache management?
What is the purpose of peripheral nerve blocks in headache management?
What is the significance of identifying anatomical landmarks for effective nerve blockade?
What is the significance of identifying anatomical landmarks for effective nerve blockade?
What is the recommended needle gauge size for injecting the solution during a greater occipital nerve block?
What is the recommended needle gauge size for injecting the solution during a greater occipital nerve block?
What is the effect of peripheral nerve blocks on the severity and frequency of migraine headaches?
What is the effect of peripheral nerve blocks on the severity and frequency of migraine headaches?
What are the adverse effects of peripheral nerve blocks?
What are the adverse effects of peripheral nerve blocks?
What is the difference between using corticosteroids for greater occipital nerve blocks and lesser occipital nerve blocks?
What is the difference between using corticosteroids for greater occipital nerve blocks and lesser occipital nerve blocks?
What is the recommended approach for patients with headache who have reproducible pain with palpation over the pericranial nerve area in the scalp?
What is the recommended approach for patients with headache who have reproducible pain with palpation over the pericranial nerve area in the scalp?
What is the recommended treatment for patients with pre-existing bleeding disorders or anticoagulation use who require peripheral nerve blocks?
What is the recommended treatment for patients with pre-existing bleeding disorders or anticoagulation use who require peripheral nerve blocks?
What is the main purpose of peripheral nerve blocks for headache disorders?
What is the main purpose of peripheral nerve blocks for headache disorders?
What is the most commonly targeted nerve for peripheral nerve blocks?
What is the most commonly targeted nerve for peripheral nerve blocks?
What type of patients are likely to respond to nerve blocks?
What type of patients are likely to respond to nerve blocks?
What is the recommended position for the patient during a greater occipital nerve block?
What is the recommended position for the patient during a greater occipital nerve block?
What type of needle should be used for injecting the solution during a greater occipital nerve block?
What type of needle should be used for injecting the solution during a greater occipital nerve block?
What type of nerve blocks involve a combination of lidocaine and/or bupivacaine?
What type of nerve blocks involve a combination of lidocaine and/or bupivacaine?
What are some possible adverse effects of peripheral nerve blocks?
What are some possible adverse effects of peripheral nerve blocks?
What is a relative contraindication for injecting patients with peripheral nerve blocks?
What is a relative contraindication for injecting patients with peripheral nerve blocks?
What type of nerve blocks are not recommended during pregnancy?
What type of nerve blocks are not recommended during pregnancy?
What is the purpose of multiple cranial nerve blocks for chronic migraines?
What is the purpose of multiple cranial nerve blocks for chronic migraines?
What type of nerve blocks have been effective in treating occipital neuralgia, supraorbital neuralgia, and auriculotemporal neuralgia?
What type of nerve blocks have been effective in treating occipital neuralgia, supraorbital neuralgia, and auriculotemporal neuralgia?
What is the main finding of a 2015 article in Cephalalgia about peripheral nerve blocks for headache medicine?
What is the main finding of a 2015 article in Cephalalgia about peripheral nerve blocks for headache medicine?
What is the most common pericranial nerve targeted in peripheral nerve blocks for headache disorders?
What is the most common pericranial nerve targeted in peripheral nerve blocks for headache disorders?
What is the role of corticosteroids in peripheral nerve blocks for headache disorders?
What is the role of corticosteroids in peripheral nerve blocks for headache disorders?
What is a relative contraindication for peripheral nerve blocks for headache disorders?
What is a relative contraindication for peripheral nerve blocks for headache disorders?
What is the purpose of using topical anaesthetic cream before peripheral nerve blocks for headache disorders?
What is the purpose of using topical anaesthetic cream before peripheral nerve blocks for headache disorders?
What is the recommended needle gauge for injecting the solution in peripheral nerve blocks for headache disorders?
What is the recommended needle gauge for injecting the solution in peripheral nerve blocks for headache disorders?
What is the patient position recommended for peripheral nerve blocks for headache disorders?
What is the patient position recommended for peripheral nerve blocks for headache disorders?
What are some common adverse effects of peripheral nerve blocks for headache disorders?
What are some common adverse effects of peripheral nerve blocks for headache disorders?
What is the recommended solution distribution for injecting the solution in peripheral nerve blocks for headache disorders?
What is the recommended solution distribution for injecting the solution in peripheral nerve blocks for headache disorders?
What is the purpose of peripheral nerve blocks for headache disorders?
What is the purpose of peripheral nerve blocks for headache disorders?
What is the recommended approach for those with troublesome and refractory headache in peripheral nerve blocks?
What is the recommended approach for those with troublesome and refractory headache in peripheral nerve blocks?
What is the most extensively studied pericranial nerve targeted in peripheral nerve blocks for headache disorders?
What is the most extensively studied pericranial nerve targeted in peripheral nerve blocks for headache disorders?
What is the role of multiple cranial nerve blocks in the treatment of headache disorders?
What is the role of multiple cranial nerve blocks in the treatment of headache disorders?
What is the prevalence of headache disorders in neurological practice?
What is the prevalence of headache disorders in neurological practice?
What is the purpose of peripheral nerve blocks in headache management?
What is the purpose of peripheral nerve blocks in headache management?
What is the evidence base for the effectiveness of peripheral nerve blocks in managing headache disorders?
What is the evidence base for the effectiveness of peripheral nerve blocks in managing headache disorders?
Which nerve is commonly targeted in peripheral nerve blocks for headache management?
Which nerve is commonly targeted in peripheral nerve blocks for headache management?
Which patients are likely to respond to nerve blocks for headache management?
Which patients are likely to respond to nerve blocks for headache management?
What are the anatomical landmarks for effective nerve blockade of the greater occipital nerve?
What are the anatomical landmarks for effective nerve blockade of the greater occipital nerve?
What is the recommended syringe size for injecting the solution in a fanlike distribution during nerve blockade of the greater occipital nerve?
What is the recommended syringe size for injecting the solution in a fanlike distribution during nerve blockade of the greater occipital nerve?
What are some adverse effects of peripheral nerve blocks?
What are some adverse effects of peripheral nerve blocks?
What is a relative contraindication for injecting patients with peripheral nerve blocks for headache management?
What is a relative contraindication for injecting patients with peripheral nerve blocks for headache management?
What is the recommended approach for those with troublesome and refractory headache?
What is the recommended approach for those with troublesome and refractory headache?
What is the effect of peripheral nerve blocks on the severity and frequency of migraine headaches?
What is the effect of peripheral nerve blocks on the severity and frequency of migraine headaches?
What is a pitfall to be aware of when administering peripheral nerve blocks?
What is a pitfall to be aware of when administering peripheral nerve blocks?
Flashcards are hidden until you start studying
Study Notes
Peripheral Nerve Blocks for Headache Disorders: A Practical Guide
-
Headache is a prevalent and disabling condition in neurological practice, and peripheral nerve blocks are commonly used to treat headache disorders.
-
There is no national consensus on the technical aspects of delivering peripheral nerve blocks, but recent studies have shown positive results in clinical practice.
-
Peripheral nerve blocks have been effective in managing acute or prolonged migrainous episodes that commonly present to the emergency department, reducing the need for opiate-based therapies.
-
The evidence base for the effectiveness of peripheral nerve blocks for managing different headache disorders varies depending on the pericranial nerve targeted and the outcome measure used.
-
The greater occipital nerve (GON) is commonly targeted, but other cervical and cranial nerves may also be treated.
-
Patients with headache who have reproducible pain with palpation over the pericranial nerve area in the scalp and those with localised cutaneous allodynia are likely to respond to nerve blocks.
-
Peripheral nerve blocks are also effective in the older population with headache disorders, whose comorbidities might preclude the use of first-line preventative medications.
-
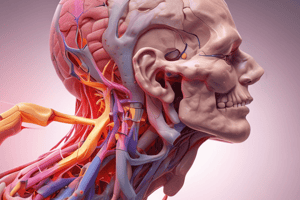
The anatomical landmarks of the occipital and superficial branches of the trigeminal nerve are important for effective nerve blockade.
-
The GON can be localised superficially by identifying a point one-third (medially) of the way between the occipital protuberance (inion) and the mastoid process, approximately 2 cm lateral and 1.5–2.0 cm below the inion.
-
The patient should be comfortably seated on a chair with the head slightly flexed, and the clinician standing behind. Use a 5 mL syringe with a 25-gauge needle to inject the solution in a fanlike distribution.
-
Corticosteroids are commonly used only for GON blocks, but some headache centres use them to infiltrate the lesser occipital nerve as well.
-
Topical anaesthetic cream a few minutes before the procedure can be used to numb the skin around the injection site, especially for the supraorbital, supratrochlear and auriculotemporal nerve injection sites.Peripheral Nerve Blocks for Headache Management: Techniques, Pitfalls, and Solutions
-
Peripheral nerve blocks are effective in the acute and preventative management of several headache disorders.
-
Neurologists can administer these blocks as a day procedure, in clinic or the emergency department.
-
Patient position and anatomical landmarks are key for successful delivery of peripheral nerve blocks.
-
Corticosteroids are frequently used for greater occipital nerve blocks but may also be used for lesser occipital nerve blocks.
-
Supraorbital, supratrochlear and auriculotemporal nerve blocks involve a combination of lidocaine and/or bupivacaine.
-
Uncommon but important adverse effects include transient dizziness, light-headedness, transient headache exacerbation, and rarely localised lipoatrophy and alopecia with corticosteroids.
-
Allergy to local anaesthetic or corticosteroid is a pitfall to be aware of; patients can receive corticosteroid-only blocks, but this limits the procedure to greater/lesser occipital nerve blocks only.
-
Bleeding during the procedure is usually minimal and applying pressure with a swab after the injection will suffice.
-
Pre-existing bleeding disorders and anticoagulation use are relative contraindications and decisions about injecting these patients should be individualised depending on the benefits and risks.
-
Pain during injection, bleeding from injection site, and dizziness are possible complications to take into account.
-
Corticosteroid nerve blocks are not recommended during pregnancy, but anaesthetic-only blocks are considered safe and recommended throughout pregnancy.
-
Peripheral nerve blocks allow an interventional approach for those with troublesome and refractory headache.Peripheral Nerve Blocks for Headache Treatment: Key Findings from Multiple Studies
-
Peripheral nerve blocks, including occipital nerve blocks, have been used as a treatment for various headache disorders.
-
A 2015 article in Cephalalgia highlights the potential benefits of peripheral nerve blocks and steroid injections for headache medicine.
-
An audit of BASH members’ practice in the UK in 2019 found that peripheral nerve blocks were commonly used for headache disorders.
-
Occipital nerve blocks have been studied extensively for their effectiveness in treating headache disorders, including migraines and cluster headaches.
-
Multiple cranial nerve blocks have also been studied as a transitional treatment for chronic headaches.
-
Studies have shown that greater occipital nerve blocks can be effective in treating prolonged or persistent migraine aura, as well as acute migraine headaches.
-
A 2011 study found that suboccipital steroid injections were effective in treating patients with more than two cluster headache attacks per day.
-
Peripheral nerve blocks have also been used to treat occipital neuralgia, supraorbital neuralgia, and auriculotemporal neuralgia.
-
Multiple cranial nerve blocks have been suggested as an alternative preventative therapy for chronic migraines.
-
Peripheral nerve blocks may have a preventive effect on the severity and frequency of migraine headaches.
-
Adverse effects of peripheral nerve blocks include Cushing syndrome, alopecia, cutaneous atrophy, and lidocaine injection-related adverse effects.
-
Expert consensus recommendations exist for the performance of peripheral nerve blocks for headaches, including anaesthetic peripheral nerve block.
Peripheral Nerve Blocks for Headache Disorders: A Practical Guide
-
Headache is a prevalent and disabling condition in neurological practice, and peripheral nerve blocks are commonly used to treat headache disorders.
-
There is no national consensus on the technical aspects of delivering peripheral nerve blocks, but recent studies have shown positive results in clinical practice.
-
Peripheral nerve blocks have been effective in managing acute or prolonged migrainous episodes that commonly present to the emergency department, reducing the need for opiate-based therapies.
-
The evidence base for the effectiveness of peripheral nerve blocks for managing different headache disorders varies depending on the pericranial nerve targeted and the outcome measure used.
-
The greater occipital nerve (GON) is commonly targeted, but other cervical and cranial nerves may also be treated.
-
Patients with headache who have reproducible pain with palpation over the pericranial nerve area in the scalp and those with localised cutaneous allodynia are likely to respond to nerve blocks.
-
Peripheral nerve blocks are also effective in the older population with headache disorders, whose comorbidities might preclude the use of first-line preventative medications.
-
The anatomical landmarks of the occipital and superficial branches of the trigeminal nerve are important for effective nerve blockade.
-
The GON can be localised superficially by identifying a point one-third (medially) of the way between the occipital protuberance (inion) and the mastoid process, approximately 2 cm lateral and 1.5–2.0 cm below the inion.
-
The patient should be comfortably seated on a chair with the head slightly flexed, and the clinician standing behind. Use a 5 mL syringe with a 25-gauge needle to inject the solution in a fanlike distribution.
-
Corticosteroids are commonly used only for GON blocks, but some headache centres use them to infiltrate the lesser occipital nerve as well.
-
Topical anaesthetic cream a few minutes before the procedure can be used to numb the skin around the injection site, especially for the supraorbital, supratrochlear and auriculotemporal nerve injection sites.Peripheral Nerve Blocks for Headache Management: Techniques, Pitfalls, and Solutions
-
Peripheral nerve blocks are effective in the acute and preventative management of several headache disorders.
-
Neurologists can administer these blocks as a day procedure, in clinic or the emergency department.
-
Patient position and anatomical landmarks are key for successful delivery of peripheral nerve blocks.
-
Corticosteroids are frequently used for greater occipital nerve blocks but may also be used for lesser occipital nerve blocks.
-
Supraorbital, supratrochlear and auriculotemporal nerve blocks involve a combination of lidocaine and/or bupivacaine.
-
Uncommon but important adverse effects include transient dizziness, light-headedness, transient headache exacerbation, and rarely localised lipoatrophy and alopecia with corticosteroids.
-
Allergy to local anaesthetic or corticosteroid is a pitfall to be aware of; patients can receive corticosteroid-only blocks, but this limits the procedure to greater/lesser occipital nerve blocks only.
-
Bleeding during the procedure is usually minimal and applying pressure with a swab after the injection will suffice.
-
Pre-existing bleeding disorders and anticoagulation use are relative contraindications and decisions about injecting these patients should be individualised depending on the benefits and risks.
-
Pain during injection, bleeding from injection site, and dizziness are possible complications to take into account.
-
Corticosteroid nerve blocks are not recommended during pregnancy, but anaesthetic-only blocks are considered safe and recommended throughout pregnancy.
-
Peripheral nerve blocks allow an interventional approach for those with troublesome and refractory headache.Peripheral Nerve Blocks for Headache Treatment: Key Findings from Multiple Studies
-
Peripheral nerve blocks, including occipital nerve blocks, have been used as a treatment for various headache disorders.
-
A 2015 article in Cephalalgia highlights the potential benefits of peripheral nerve blocks and steroid injections for headache medicine.
-
An audit of BASH members’ practice in the UK in 2019 found that peripheral nerve blocks were commonly used for headache disorders.
-
Occipital nerve blocks have been studied extensively for their effectiveness in treating headache disorders, including migraines and cluster headaches.
-
Multiple cranial nerve blocks have also been studied as a transitional treatment for chronic headaches.
-
Studies have shown that greater occipital nerve blocks can be effective in treating prolonged or persistent migraine aura, as well as acute migraine headaches.
-
A 2011 study found that suboccipital steroid injections were effective in treating patients with more than two cluster headache attacks per day.
-
Peripheral nerve blocks have also been used to treat occipital neuralgia, supraorbital neuralgia, and auriculotemporal neuralgia.
-
Multiple cranial nerve blocks have been suggested as an alternative preventative therapy for chronic migraines.
-
Peripheral nerve blocks may have a preventive effect on the severity and frequency of migraine headaches.
-
Adverse effects of peripheral nerve blocks include Cushing syndrome, alopecia, cutaneous atrophy, and lidocaine injection-related adverse effects.
-
Expert consensus recommendations exist for the performance of peripheral nerve blocks for headaches, including anaesthetic peripheral nerve block.
Peripheral Nerve Blocks for Headache Disorders: A Practical Guide
-
Headache is a prevalent and disabling condition in neurological practice, and peripheral nerve blocks are commonly used to treat headache disorders.
-
There is no national consensus on the technical aspects of delivering peripheral nerve blocks, but recent studies have shown positive results in clinical practice.
-
Peripheral nerve blocks have been effective in managing acute or prolonged migrainous episodes that commonly present to the emergency department, reducing the need for opiate-based therapies.
-
The evidence base for the effectiveness of peripheral nerve blocks for managing different headache disorders varies depending on the pericranial nerve targeted and the outcome measure used.
-
The greater occipital nerve (GON) is commonly targeted, but other cervical and cranial nerves may also be treated.
-
Patients with headache who have reproducible pain with palpation over the pericranial nerve area in the scalp and those with localised cutaneous allodynia are likely to respond to nerve blocks.
-
Peripheral nerve blocks are also effective in the older population with headache disorders, whose comorbidities might preclude the use of first-line preventative medications.
-
The anatomical landmarks of the occipital and superficial branches of the trigeminal nerve are important for effective nerve blockade.
-
The GON can be localised superficially by identifying a point one-third (medially) of the way between the occipital protuberance (inion) and the mastoid process, approximately 2 cm lateral and 1.5–2.0 cm below the inion.
-
The patient should be comfortably seated on a chair with the head slightly flexed, and the clinician standing behind. Use a 5 mL syringe with a 25-gauge needle to inject the solution in a fanlike distribution.
-
Corticosteroids are commonly used only for GON blocks, but some headache centres use them to infiltrate the lesser occipital nerve as well.
-
Topical anaesthetic cream a few minutes before the procedure can be used to numb the skin around the injection site, especially for the supraorbital, supratrochlear and auriculotemporal nerve injection sites.Peripheral Nerve Blocks for Headache Management: Techniques, Pitfalls, and Solutions
-
Peripheral nerve blocks are effective in the acute and preventative management of several headache disorders.
-
Neurologists can administer these blocks as a day procedure, in clinic or the emergency department.
-
Patient position and anatomical landmarks are key for successful delivery of peripheral nerve blocks.
-
Corticosteroids are frequently used for greater occipital nerve blocks but may also be used for lesser occipital nerve blocks.
-
Supraorbital, supratrochlear and auriculotemporal nerve blocks involve a combination of lidocaine and/or bupivacaine.
-
Uncommon but important adverse effects include transient dizziness, light-headedness, transient headache exacerbation, and rarely localised lipoatrophy and alopecia with corticosteroids.
-
Allergy to local anaesthetic or corticosteroid is a pitfall to be aware of; patients can receive corticosteroid-only blocks, but this limits the procedure to greater/lesser occipital nerve blocks only.
-
Bleeding during the procedure is usually minimal and applying pressure with a swab after the injection will suffice.
-
Pre-existing bleeding disorders and anticoagulation use are relative contraindications and decisions about injecting these patients should be individualised depending on the benefits and risks.
-
Pain during injection, bleeding from injection site, and dizziness are possible complications to take into account.
-
Corticosteroid nerve blocks are not recommended during pregnancy, but anaesthetic-only blocks are considered safe and recommended throughout pregnancy.
-
Peripheral nerve blocks allow an interventional approach for those with troublesome and refractory headache.Peripheral Nerve Blocks for Headache Treatment: Key Findings from Multiple Studies
-
Peripheral nerve blocks, including occipital nerve blocks, have been used as a treatment for various headache disorders.
-
A 2015 article in Cephalalgia highlights the potential benefits of peripheral nerve blocks and steroid injections for headache medicine.
-
An audit of BASH members’ practice in the UK in 2019 found that peripheral nerve blocks were commonly used for headache disorders.
-
Occipital nerve blocks have been studied extensively for their effectiveness in treating headache disorders, including migraines and cluster headaches.
-
Multiple cranial nerve blocks have also been studied as a transitional treatment for chronic headaches.
-
Studies have shown that greater occipital nerve blocks can be effective in treating prolonged or persistent migraine aura, as well as acute migraine headaches.
-
A 2011 study found that suboccipital steroid injections were effective in treating patients with more than two cluster headache attacks per day.
-
Peripheral nerve blocks have also been used to treat occipital neuralgia, supraorbital neuralgia, and auriculotemporal neuralgia.
-
Multiple cranial nerve blocks have been suggested as an alternative preventative therapy for chronic migraines.
-
Peripheral nerve blocks may have a preventive effect on the severity and frequency of migraine headaches.
-
Adverse effects of peripheral nerve blocks include Cushing syndrome, alopecia, cutaneous atrophy, and lidocaine injection-related adverse effects.
-
Expert consensus recommendations exist for the performance of peripheral nerve blocks for headaches, including anaesthetic peripheral nerve block.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.