Podcast
Questions and Answers
What is the primary function of the postanesthesia care unit (PACU)?
What is the primary function of the postanesthesia care unit (PACU)?
- To provide extended care for patients requiring ongoing observation.
- To provide care for patients recovering from anesthesia or moderate sedation/analgesia. (correct)
- To manage long-term rehabilitation for patients after surgery.
- To prepare patients for self-care and discharge to home.
A patient is being discharged to a rehabilitation center after a hip replacement. Which phase of postoperative care is this patient entering?
A patient is being discharged to a rehabilitation center after a hip replacement. Which phase of postoperative care is this patient entering?
- Phase III
- PACU phase
- Phase I
- Phase II (correct)
In which postoperative phase is close monitoring of airway, ventilation, hemodynamic stability, and pain control most critical?
In which postoperative phase is close monitoring of airway, ventilation, hemodynamic stability, and pain control most critical?
- Phase II
- Phase III
- Phase I (correct)
- Extended Care
A patient undergoes same-day surgery. What nursing intervention is most important to implement?
A patient undergoes same-day surgery. What nursing intervention is most important to implement?
Which classification describes a surgery scheduled to remove a non-malignant skin lesion?
Which classification describes a surgery scheduled to remove a non-malignant skin lesion?
A patient requires immediate surgery to control internal bleeding from a traumatic injury. How is this surgery classified in terms of urgency?
A patient requires immediate surgery to control internal bleeding from a traumatic injury. How is this surgery classified in terms of urgency?
A patient is scheduled for a diagnostic laparoscopy to determine the cause of abdominal pain. What is the primary purpose of this surgical procedure?
A patient is scheduled for a diagnostic laparoscopy to determine the cause of abdominal pain. What is the primary purpose of this surgical procedure?
Which surgical classification aims to alleviate symptoms without curing the underlying disease, such as nerve root resection for chronic pain?
Which surgical classification aims to alleviate symptoms without curing the underlying disease, such as nerve root resection for chronic pain?
What type of surgery is a cleft palate repair considered, based on its purpose?
What type of surgery is a cleft palate repair considered, based on its purpose?
In preparing a patient psychologically for surgery, what strategy is most effective in addressing their anxiety?
In preparing a patient psychologically for surgery, what strategy is most effective in addressing their anxiety?
Which common patient question should a nurse be prepared to answer when a patient is scheduled for surgery?
Which common patient question should a nurse be prepared to answer when a patient is scheduled for surgery?
Why is preoperative teaching about postoperative activities important for surgical patients?
Why is preoperative teaching about postoperative activities important for surgical patients?
What is a key consideration when timing preoperative teaching for a patient undergoing surgery?
What is a key consideration when timing preoperative teaching for a patient undergoing surgery?
Which of the following is a typical activity included in the preoperative phase of in-hospital surgery?
Which of the following is a typical activity included in the preoperative phase of in-hospital surgery?
Why are leg exercises important to teach patients before surgery?
Why are leg exercises important to teach patients before surgery?
What is the purpose of teaching a patient to splint their incision when coughing after surgery?
What is the purpose of teaching a patient to splint their incision when coughing after surgery?
Which action is essential when providing preoperative care on the day of surgery?
Which action is essential when providing preoperative care on the day of surgery?
What is the primary goal of the intraoperative phase of the nursing process?
What is the primary goal of the intraoperative phase of the nursing process?
Why is it important for the nurse to assess the surgical site dressing for drainage in the postoperative period?
Why is it important for the nurse to assess the surgical site dressing for drainage in the postoperative period?
What immediate action should the nurse take if a postoperative patient shows a significant deviation from their preoperative vital signs?
What immediate action should the nurse take if a postoperative patient shows a significant deviation from their preoperative vital signs?
Which intervention is most appropriate to promote respiratory function and prevent complications after surgery?
Which intervention is most appropriate to promote respiratory function and prevent complications after surgery?
What is the rationale for using an incentive spirometer postoperatively?
What is the rationale for using an incentive spirometer postoperatively?
A nurse notices that the patient is repositioning and guarding. These are the potential signs and symptoms of which post operative health problem?
A nurse notices that the patient is repositioning and guarding. These are the potential signs and symptoms of which post operative health problem?
A patient is complaining of pain. A nurse assesses the patient and determines the prescribed pain medication should be administered. Which aspect of comfort is the nurse addressing?
A patient is complaining of pain. A nurse assesses the patient and determines the prescribed pain medication should be administered. Which aspect of comfort is the nurse addressing?
A nurse elevated the side rails and place the bed in the locked, low position. What aspect of post-operative care is the nurse addressing?
A nurse elevated the side rails and place the bed in the locked, low position. What aspect of post-operative care is the nurse addressing?
Flashcards
PACU
PACU
Area adjacent to surgical suite for recovering patients from anesthesia/sedation.
Postoperative phase
Postoperative phase
Begins upon PACU admission; ends with full recovery after last follow-up visit. Has 3 phases
Postoperative Phase I
Postoperative Phase I
High monitoring for airway, breathing, circulation, fluids, lytes, and pain.
Postoperative Phase II
Postoperative Phase II
Signup and view all the flashcards
Postoperative Phase III
Postoperative Phase III
Signup and view all the flashcards
Elective Surgery
Elective Surgery
Signup and view all the flashcards
Urgent Surgery
Urgent Surgery
Signup and view all the flashcards
Emergency Surgery
Emergency Surgery
Signup and view all the flashcards
Diagnostic Surgery
Diagnostic Surgery
Signup and view all the flashcards
Ablative Surgery
Ablative Surgery
Signup and view all the flashcards
Palliative Surgery
Palliative Surgery
Signup and view all the flashcards
Reconstructive Surgery
Reconstructive Surgery
Signup and view all the flashcards
Transplantation Surgery
Transplantation Surgery
Signup and view all the flashcards
Constructive Surgery
Constructive Surgery
Signup and view all the flashcards
Intentional presence
Intentional presence
Signup and view all the flashcards
Deep-breathing exercises
Deep-breathing exercises
Signup and view all the flashcards
Deep-breathing Technique
Deep-breathing Technique
Signup and view all the flashcards
Coughing after surgery
Coughing after surgery
Signup and view all the flashcards
Splinting the Incision
Splinting the Incision
Signup and view all the flashcards
Incentive Spirometry
Incentive Spirometry
Signup and view all the flashcards
Leg exercises
Leg exercises
Signup and view all the flashcards
Turning in Bed
Turning in Bed
Signup and view all the flashcards
Preoperative checklist
Preoperative checklist
Signup and view all the flashcards
Intraoperative Phase
Intraoperative Phase
Signup and view all the flashcards
Causes of acute pain
Causes of acute pain
Signup and view all the flashcards
Study Notes
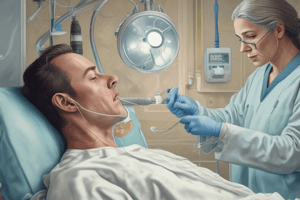
- Postanesthesia Care Unit (PACU): A special area near the surgical suite for patients recovering from anesthesia or sedation/analgesia.
- Postoperative Phase: Starts upon PACU admission and ends with full recovery and the final healthcare visit.
- Phase I: Intensive monitoring for airway, ventilation, hemodynamics, fluids/electrolytes, and pain.
- Phase II: Patient is ready for self-care or transfer to extended care, no longer needs acute measures.
- Phase III (Extended Care): Ongoing care for patients needing extended observation after Phase I/II.
- Surgical procedures are classified by urgency, risk, and purpose.
- All surgical procedures carry physical and psychological stress.
Classification of Surgical Procedures Based on Urgency
- Elective: Surgery can be delayed with no ill effects, scheduled in advance.
- Example: Tonsillectomy, hernia repair, cataract extraction, hip prosthesis, facelift, mammoplasty.
- Urgent: Needs to be done within 24-48 hours.
- Example: Gallbladder removal, coronary artery bypass graft (CABG), malignant tumor removal, colon resection, amputation.
- Emergency: Needs immediate action.
- Example: Hemorrhage control, trauma repair, perforated ulcer, intestinal obstruction, tracheostomy.
Classification of Surgical Procedures Based on Degree of Risk
- Major: May be elective, urgent, or emergency
- Example: Carotid endarterectomy, cholecystectomy, nephrectomy, colostomy, hysterectomy, radical mastectomy, amputation, trauma repair, CABG.
- Minor: Primarily elective
- Example: Tooth extraction, removal of warts, skin biopsy, dilation and curettage, laparoscopy, cataract extraction, arthroscopy.
Classification of Surgical Procedures Based on Purpose
- Diagnostic: To make or confirm a diagnosis
- Example: Breast biopsy, laparoscopy, exploratory laparotomy.
- Ablative: To remove a diseased body part
- Example: Appendectomy, subtotal thyroidectomy, partial gastrectomy, colon resection, amputation.
- Palliative: To relieve/reduce illness intensity, not curative.
- Example: Colostomy, nerve root resection, necrotic tissue debridement, tumor debulking, arthroscopy.
- Reconstructive: To restore function to traumatized or malfunctioning tissue, improves self-concept.
- Example: Scar revision, plastic surgery, skin graft, internal fracture fixation, breast reconstruction.
- Transplantation: To replace diseased/malfunctioning organs/structures.
- Example: Kidney, liver, cornea, heart, joints.
- Constructive: To restore function in congenital anomalies.
- Example: Cleft palate repair, closure of atrial-septal defect.
Nursing Interventions for Psychological Needs
- Use intentional presence, focus on being in the moment with the patient.
- Build/maintain a therapeutic relationship, allowing verbalization of fears/concerns.
- Use active listening to catch and understand anxiety/fear.
- Use touch, when appropriate, to show empathy and caring.
- Be ready to answer common surgery questions.
Common Patient Questions About Surgery
- Includes questions about loss of bodily control, OR and PACU time, family location, pain after waking up, anesthetic side effects, blood transfusions, time before eating, scar appearance, sexual activity, and return to work.
Preparing the Patient Psychologically Through Teaching
- Teaching about postoperative activities is a nursing responsibility implemented preoperatively.
- Information includes what to expect, pain management, and the physical activities necessary to reduce risk for complications.
- Success depends on timing, patient/support system, surgery type, individual/group sessions, universal and individual patient needs.
- Patients with detailed preoperative instructions manage surgery better and take part in self-care.
- Teaching too early or when the patient is anxious is not as effective.
- Preoperative teaching checklists give guidelines for instruction.
Teaching About Surgical Events and Sensations
- When surgery is scheduled, explain how long it and postanesthesia care will last, including pre-, during, and post-operative events.
Sample Preoperative Teaching: Activities and Events for In-Hospital Surgery
- Preoperative Phase:
- Exercises (deep breathing, coughing, incentive spirometry, turning, leg).
- Pain management (PRN orders, multimodal options, timing, splinting incision, nonpharmacologic methods).
- Anesthesiologist/CRNA visit.
- Physical prep (NPO, medications).
- Preoperative checklist review.
- Transportation to OR, visitors, waiting room.
- Intraoperative Phase:
- Holding area.
- Skin preparation.
- IV lines/fluids.
- Medications.
- OR environment (bed, lights, equipment).
- Safety measures.
- Sensations.
- Healthcare team roles.
- Postoperative Phase:
- PACU.
- Frequent vital signs, assessments.
- Dressings, drains, tubes, catheters.
- IV lines.
- Pain/comfort measures.
- Family notification.
- Sensations.
- Airway/oxygen therapy/pulse oximetry.
- Healthcare team roles.
- Unit transfer.
- Frequent vital signs.
- Sensations.
- Pain medications/nonpharmacologic strategies.
- NPO, diet progression.
- Exercises.
- Early ambulation.
- Visitation policies.
Teaching Deep-Breathing Techniques
- Patient position: semi-Fowler's with neck/shoulders supported.
- Place hands over the rib cage so the patient feels chest expansion.
- Steps:
- Exhale gently and completely.
- Inhale gently and completely through the nose.
- Hold the breath for 3-5 seconds, counting mentally.
- Exhale completely through pursed lips.
- Repeat three times.
- Do every 1-2 hours while awake the first 24 hours, and as needed afterward.
Rationale for Deep-Breathing Techniques
- Deep-breathing exercises help prevent atelectasis and respiratory infection.
- Deep-breathing hyperventilate alveoli, improving lung expansion/volume, expelling anesthetic gases/mucus, and enhancing tissue oxygenation.
Coughing Techniques
- Helps remove retained mucus.
- Teach in conjunction with with deep breathing
- Important for patients at risk of respiratory complications.
- Splint the incision with a pillow to reduce pain.
Incentive Spirometry
- Often prescribed for patients after surgery.
- Technique should be taught properly.
- Increases lung volume, promotes alveoli inflation, and aids venous return.
- Gauge allows measurement of progress and is positive reinforcement.
Leg Exercises
- During surgery, venous blood return slows from the legs which can increase the risk for DVT, thrombophlebitis, and emboli.
- Leg exercises increase venous return through flexion and contraction of the quadriceps and gastrocnemius muscles.
- Individualized to patient’s needs, condition, and physician preference.
Turning in Bed
- Improves venous return, respiratory function, and intestinal peristalsis, while preventing the effects of immobility.
Effective Coughing Guidelines
- Position: Semi-Fowler's, leaning forward.
- Provide a pillow/bath blanket to splint incision.
- Steps:
- Inhale/exhale deeply/slowly through the nose three times.
- Take a deep breath, hold for 3 seconds.
- "Hack" out three short breaths.
- Take a quick breath with mouth open.
- Cough deeply once/twice.
- Take another deep breath.
- Repeat every 2 hours while awake.
Preoperative Patient Care: Hospitalized Patient (Day of Surgery)
- Check consent forms are signed, correct, dated, and witnessed, and advance directives are in place.
- Gather equipment and supplies.
- Perform hand hygiene.
- Check vital signs and report any changes.
- Provide oral care/assess loose teeth, verify food/fluid restrictions were followed.
- Facilitate/verify bathing and prep skin with antiseptic per the protocol.
- Clothing and jewelry removal, including body piercings and nail polish.
- Secure valuables with a family member or in the hospital safe.
- Have the patient empty their bladder.
- Attend to any special orders (IV lines).
- Complete the preoperative checklist.
- Administer preoperative medications.
- Raise side rails/lower the bed, instruct the patient to stay on the bed/stretcher, using a safety belt if necessary.
- Help move the patient to the transport stretcher, reconfirm/document information.
- Inform the family of the patient's post-surgery location and where the surgeon will provide an update.
- After the patient leaves for OR, prepare the room and make a postoperative bed for the patient.
Intraoperative Nursing Care
- Begins with admission to the surgical area and ends when the patient is transferred to the PACU.
- Collaborative effort to meet patient needs intraoperatively.
- Surgical scrub attire. Assess emotional/physical status and verify preoperative checklist information, including assessment data, lab reports, and consents. Perform skin preparation, start IV fluids, place IPCDs, determine pain level, give preop medications, and provide comfort.
- Anesthetize, position, prep, and drape the patient, reviews preoperative data, and continually maintain safety (positioning and monitoring).
Diagnosing Actual or Potential Health Problems and Needs (Intraoperative)
- May occur due to patient positioning, anesthesia effects, equipment use, tissue disruption during the procedure, and incision.
Outcome Identification and Planning (Intraoperative)
- Identify interventions to prevent complications/ensure safety.
- Expected outcomes: free of neuromuscular injury; free from wrong-site, wrong-side, wrong-patient surgical procedure.
Postoperative Assessments and Interventions
- Vital signs and oxygen saturation:
- Obtain temperature, blood pressure, pulse, respiratory rate, and oxygen saturation.
- Note, report, and document deviations from preoperative and PACU data as well as symptoms of complications.
- Color and temperature of skin:
- Inspect skin for color (pallor, cyanosis), temperature, and moisture (diaphoresis).
- Level of consciousness:
- Verify type of anesthesia and any reversal agents administered.
- Assess and reorient (as needed) to person, place, and time.
- Assess reaction to stimuli and ability to move all four extremities.
- Intravenous fluids:
- Verify estimated blood loss in the OR.
- Check infusion site(s).
- Verify type and amount of solution, flow rate, security, and patency of tubing.
- Surgical site:
- Verify surgical procedure, location, approach, and any positioning requirements.
- Assess dressing and dependent areas for drainage (color, amount, consistency).
- Other tubes:
- Secure drains and tubes, ensure that they are intact/patent and properly connected to drainage systems.
- Assess indwelling urinary catheter, gastrointestinal suction, and other tubes for drainage, patency, and amount of output.
- Ensure that dependent drainage bags are hanging properly and suction drainage is attached and functioning.
- If oxygen is prescribed, ensure placement of prescribed application and flow rate.
- Comfort:
- Verify orders for pain medications including medication(s), dose, route, and frequency.
- Assess pain (location, duration, intensity) and determine whether analgesics were given in the PACU.
- Assess for nausea and vomiting.
- Cover the patient with a blanket.
- Reorient to the room as necessary.
- Allow visitors to remain with the patient after the initial assessment is completed.
- Position and Safety:
- Place the patient in an ordered position or, if the patient is not fully conscious, place in the side-lying position.
- Elevate the side rails and place the bed in locked and low position.
- Perform a focused or brief head-to-toe assessment to establish a baseline.
Postoperative Patient Actual or Potential Health Problems and Needs
- Acute Pain:
- Etiologic factors may include surgical incision, required surgical positioning, and required movement to prevent postoperative complications.
- Potential signs and symptoms include change in physiologic parameters (pulse, respirations, blood pressure), self-report or evidence of pain characteristics using a standardized pain instrument, instinctive and/or frequent repositioning or guarding, joint and/or tissue with neurologic discomfort, and hesitation or refusal to ambulate or engage in coughing and deep breathing exercises.
- Surgical Site Infection Risk
- Etiologic factors may include patient-specific factor (comorbidities, nutritional state, compensatory mechanisms, immune response), environmental personnel/equipment failure, and contamination of the sterile field.
- No potential signs and symptoms given.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.