Podcast
Questions and Answers
Which of the following best describes the primary function of the periodontal ligament (PDL)?
Which of the following best describes the primary function of the periodontal ligament (PDL)?
- To act as a barrier, preventing bacterial invasion into the alveolar bone.
- To secrete enamel proteins for tooth remineralization.
- To facilitate the movement of the mandible during mastication.
- To provide a cushion between the tooth and bone, absorbing forces generated during chewing. (correct)
The periodontal ligament is continuous with the connective tissue of the gingiva, and also communicates with what other structure?
The periodontal ligament is continuous with the connective tissue of the gingiva, and also communicates with what other structure?
- The cementum of the root
- The marrow spaces through vascular channels in the bone (correct)
- The dentinal tubules of the root
- The enamel of the crown
Which of the following is NOT a known function of the periodontal ligament?
Which of the following is NOT a known function of the periodontal ligament?
- Sensory
- Nutritive
- Excretory (correct)
- Physical
The average width of the periodontal ligament (PDL) is approximately 0.2mm. Under which loading condition is the width of the PDL expected to be the smallest?
The average width of the periodontal ligament (PDL) is approximately 0.2mm. Under which loading condition is the width of the PDL expected to be the smallest?
Which statement best describes the appearance of the periodontal ligament on a radiograph?
Which statement best describes the appearance of the periodontal ligament on a radiograph?
After root development begins, from which structure does the periodontal ligament primarily originate?
After root development begins, from which structure does the periodontal ligament primarily originate?
What feature characterizes the initial arrangement of fibers during the development of the periodontal ligament?
What feature characterizes the initial arrangement of fibers during the development of the periodontal ligament?
Which type of fibers are the first to appear apical to the cementoenamel junction (CEJ) during periodontal ligament development?
Which type of fibers are the first to appear apical to the cementoenamel junction (CEJ) during periodontal ligament development?
Sharpey's fibres are embedded in bone and cementum. How does the arrangement of Sharpey's fibres in bone differ from their arrangement in cementum?
Sharpey's fibres are embedded in bone and cementum. How does the arrangement of Sharpey's fibres in bone differ from their arrangement in cementum?
What is the correct order (first to last) of the appearance of Sharpey's fibres during eruption?
What is the correct order (first to last) of the appearance of Sharpey's fibres during eruption?
What is the most abundant structural element within the periodontal ligament?
What is the most abundant structural element within the periodontal ligament?
The periodontal ligament receives its principal blood supply from:
The periodontal ligament receives its principal blood supply from:
Which of the following is a primary function of the oblique fiber group of the periodontal ligament?
Which of the following is a primary function of the oblique fiber group of the periodontal ligament?
Which principal fiber group of the periodontal ligament is only found in multirooted teeth?
Which principal fiber group of the periodontal ligament is only found in multirooted teeth?
What is the primary function of the interdental ligament (transseptal fibers)?
What is the primary function of the interdental ligament (transseptal fibers)?
Which component of the periodontal ligament ground substance is responsible for the exchange of metabolites?
Which component of the periodontal ligament ground substance is responsible for the exchange of metabolites?
The periodontal ligament is supplied by how many types of nerves?
The periodontal ligament is supplied by how many types of nerves?
Which of the following is a characteristic change observed in the periodontal ligament with age?
Which of the following is a characteristic change observed in the periodontal ligament with age?
With age-related changes in the periodontal ligament and calcified tissues, what specific structural alteration is often observed?
With age-related changes in the periodontal ligament and calcified tissues, what specific structural alteration is often observed?
Which of the following is the implication of periodontal disease on transseptal fibers?
Which of the following is the implication of periodontal disease on transseptal fibers?
Flashcards
Periodontal Ligament (PDL)
Periodontal Ligament (PDL)
Connective tissue surrounding the tooth root, connecting it to the bone. It is continuous with gingiva and communicates with marrow spaces.
Functions of Periodontal Ligament
Functions of Periodontal Ligament
The PDL performs sensory, nutritive, physical and formative (remodelling) / resorptive functions to maintain the tooth in its socket
PDL on a radiograph
PDL on a radiograph
The ligament showing up as the periodontal space on radiographs.
Development of the PDL
Development of the PDL
Signup and view all the flashcards
Fibers of Periodontal Ligament
Fibers of Periodontal Ligament
Signup and view all the flashcards
Alveolar Crest Fibres
Alveolar Crest Fibres
Signup and view all the flashcards
Horizontal Group Fibres
Horizontal Group Fibres
Signup and view all the flashcards
Oblique Group Fibres
Oblique Group Fibres
Signup and view all the flashcards
Apical Group Fibres
Apical Group Fibres
Signup and view all the flashcards
Inter-radicular Group Fibres
Inter-radicular Group Fibres
Signup and view all the flashcards
Study Notes
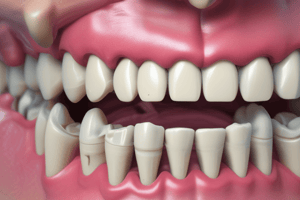
- The periodontal ligament (PDL) is a connective tissue that surrounds the root of the tooth, connecting it to the bone
- The PDL is continuous with the gingival connective tissue and communicates with bone marrow spaces through vascular channels
- At the root apex, the PDL merges with the dental pulp
Functions of the Periodontal Ligament
- Sensory
- Physical
- Nutritive
- Formative & (remodelling)resorptive
PDL Width
- The average width of PDL is 0.2mm
- PDL width range spans from 0.15mm to 0.38mm
- Near the crest of the alveolus, the width of PDL is 0.35mm when heavily loaded, 0.14mm when normally loaded, and 0.10mm when functionless
- In the middle of the alveolus, the width of PDL measures 0.28mm when heavily loaded, 0.10mm when normally loaded, and 0.06mm when functionless
- Approaching the fundus of the alveolus, the PDL width is 0.30mm in heavy loading, 0.12mm under normal loading, and 0.06mm when functionless
PDL on Radiographs
- It appears as periodontal space on radiographs
- It is a radiolucent area between the lamina dura of alveolar bone proper and radiopaque cementum
- It is narrower in permanent teeth compared to deciduous teeth
Development of PDL
- Originates from the dental follicle shortly after root development begins
- As crown approaches the oral mucosa, fibroblasts in the follicle become active
- Fibres initially lack organization, becoming oblique to the tooth
- First fibres are apical to the cementoenamel junction (CEJ), giving rise to gingivodental fibres
- With eruption, more fibres develop, attaching to new cementum and bone
- During eruption, cemental Sharpey’s fibres appear first, followed by Sharpey’s fibres in bone
- Sharpey's fibres in bone are fewer
- Alveolar fibres extend into the middle zone, joining the lengthening cemental fibres, gaining thickness and strength during occlusal function
Structural Elements of PDL
- Cells
- Fibres
- Ground substance
- Extracellular substance
- Epithelial rests of malassez
- Defence
- Progenitor
- Resorptive
- Synthetic
Blood Supply
- The principal blood supply comes from the superior and inferior alveolar arteries
- Apical vessels
- Penetrating vessels from the alveolar bone
- Anastomosing vessels from the gingiva
- Vessels anastomose freely within the ligament, occupying interstitial spaces
Nerve supply
- Sensory nerves
- Autonomic nerves
- Branches of the second & third division of the 5th cranial nerve (trigeminal nerve)
Fibres of Periodontal Ligament
- All fibres are made from collagen
- PDL is wider near the apex and cervical margin of the tooth
- Most fibres are principal fibres, organized into groups, resembling spliced ropes
- Fibres distribute forces of mastication & speech
- Principal fibres are embedded into cementum & bone, known as Sharpey's fibres
Principal Fibre Groups
- Main principal fibres consists of 5 groups
- Alveolar crest group
- Horizontal group
- Oblique group
- Apical group
- Interradicular group
- The overall function of the five groups is to resist rotational forces
Alveolar Crest Group Fibres
- Located just beneath the junctional epithelium
- Originates from cementum, below the CEJ
- Runs downwards and outwards, inserting into the alveolar crest
- Prevents tooth extrusion from the socket and resists lateral, tilting, and intrusive tooth displacement
Horizontal Group Fibres
- Located limited to the coronal one-fourth of PDL
- Originates from cementum, apical to the alveolar crest group
- Runs at right angles to the long axis of the tooth, inserting into the bone apical to the alveolar crest
- Resists horizontal and tipping forces
Oblique Group Fibres
- Located in the two thirds of length of the PDL
- Originates from cementum
- Runs obliquely in the coronal direction and inserts into the alveolar bone
- Largest group of fibres
- It resists vertical masticatory forces, preventing tooth intrusion
Apical Group Fibres
- Located at the root tip
- Originates from cementum, around the apex of the tooth
- Fans out in an irregular fashion and inserts into the apex of the socket
- Not found in incompletely formed roots
- They resist vertical, luxative & twisting forces, protecting delicate nerves and vessels at the apex
Inter-radicular Group Fibres
- Located roots of multi rooted teeth
- Originates from cementum
- Insertion located to interradicular septum
- Resists vertical & lateral movement
- Assist with Tipping, torquing & luxation
- Periodontal disease results in total loss of fibres
Interdental Ligament (Transseptal Fibres)
- Important fibres which run through gingival mucosa to connect neighboring teeth
- Inserts interdentally into cervical cementum of neighboring teeth over alveolar crest
- Fibres travel from cementum to cementum without any bony attachment
- Resists rotational forces & keeps teeth in alignment
Gingival Fibre Group
- A name given to separated but adjacent fibre groups found within the lamina propria of marginal gingiva
Ground Substance
- Collagen fibres
- Water 70%
- Tissue fluid pressure high, 10mm Hg above atmospheric pressure
- Functions include the exchange of metabolites, ion & water binding, fibre orientation, and tooth support & binding mechanisms
Age Changes
- Number of cells decrease
- Increase in fibrous tissue
- Decrease in vascularity and mitotic activity
- Narrowing of PDL width
- Scalloping is seen on calcified tissues with PDL attached to the peaks of scallops
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.