Podcast
Questions and Answers
Which part of the true pelvis is measured during an internal examination?
Which part of the true pelvis is measured during an internal examination?
- Interspinous diameter
- Pelvic brim
- Transverse diameter
- Obstetric conjugate (correct)
What is the primary role of the coccyx during labor?
What is the primary role of the coccyx during labor?
- To form the pelvic canal
- To allow the fetal head to descend (correct)
- To protect the lumbar vertebrae
- To support the uterus throughout pregnancy
What is cervical effacement?
What is cervical effacement?
- The rapid descent of the fetal head
- Formation of the physiological retraction ring
- Thinning of the cervical canal (correct)
- Widening of the cervical os
What indicates the smallest diameter of the pelvic canal?
What indicates the smallest diameter of the pelvic canal?
During labor, how does the curvature of the pelvic canal affect the fetal head's descent?
During labor, how does the curvature of the pelvic canal affect the fetal head's descent?
What is the most important diameter at the pelvic outlet?
What is the most important diameter at the pelvic outlet?
What is the primary power that effects physiological alterations during labor?
What is the primary power that effects physiological alterations during labor?
What happens to the cervical os during complete dilatation?
What happens to the cervical os during complete dilatation?
What is Bandl’s ring associated with?
What is Bandl’s ring associated with?
Which of the following factors is suggested to cause pain during labor?
Which of the following factors is suggested to cause pain during labor?
What does the 'increment' phase of a uterine contraction refer to?
What does the 'increment' phase of a uterine contraction refer to?
Which characteristic of uterine contraction measures the time from the end of one contraction to the start of the next?
Which characteristic of uterine contraction measures the time from the end of one contraction to the start of the next?
How does the intensity of a contraction change during labor?
How does the intensity of a contraction change during labor?
What is indicated by a frequency of contractions diminishing over time?
What is indicated by a frequency of contractions diminishing over time?
Which factor might contribute to the sensation of labor pain due to physical mechanisms?
Which factor might contribute to the sensation of labor pain due to physical mechanisms?
What describes the acme phase of a uterine contraction?
What describes the acme phase of a uterine contraction?
What is the process referred to as when the fetal head moves downward within the pelvic inlet?
What is the process referred to as when the fetal head moves downward within the pelvic inlet?
What aids the flexion of the fetal head during the descent?
What aids the flexion of the fetal head during the descent?
During which movement does the occiput rotate until it is positioned superior to the symphysis pubis?
During which movement does the occiput rotate until it is positioned superior to the symphysis pubis?
What is the function of Ritgen's Maneuver in the delivery process?
What is the function of Ritgen's Maneuver in the delivery process?
What describes the position of the fetal head at the beginning of internal rotation?
What describes the position of the fetal head at the beginning of internal rotation?
Which stage follows the birth of the infant and involves the delivery of the placenta?
Which stage follows the birth of the infant and involves the delivery of the placenta?
What happens during external rotation immediately after the birth of the infant's head?
What happens during external rotation immediately after the birth of the infant's head?
What occurs once the shoulders of the baby are delivered?
What occurs once the shoulders of the baby are delivered?
What is the purpose of a lumbar epidural during the first stage of labor?
What is the purpose of a lumbar epidural during the first stage of labor?
Which anesthetic is used in a pudendal block for perineal anesthesia?
Which anesthetic is used in a pudendal block for perineal anesthesia?
What is a key advantage of a mediolateral episiotomy over a midline episiotomy?
What is a key advantage of a mediolateral episiotomy over a midline episiotomy?
What is a common nursing responsibility in the 4th stage of labor?
What is a common nursing responsibility in the 4th stage of labor?
What effect can a high, firm fundus after placental delivery indicate?
What effect can a high, firm fundus after placental delivery indicate?
What is the primary purpose of local infiltration of the perineum with lidocaine?
What is the primary purpose of local infiltration of the perineum with lidocaine?
How soon does anesthesia from a lumbar epidural typically last after administration?
How soon does anesthesia from a lumbar epidural typically last after administration?
What nursing action benefits a patient experiencing swelling after an episiotomy?
What nursing action benefits a patient experiencing swelling after an episiotomy?
What does lochia alba consist of?
What does lochia alba consist of?
What may cause chills in a mother following delivery?
What may cause chills in a mother following delivery?
What is one characteristic of a full bladder after delivery?
What is one characteristic of a full bladder after delivery?
What is the best method for relieving chills in a postpartum mother?
What is the best method for relieving chills in a postpartum mother?
What can happen if a full bladder is not addressed after delivery?
What can happen if a full bladder is not addressed after delivery?
How frequently should vital signs be monitored after delivery when the patient is stable?
How frequently should vital signs be monitored after delivery when the patient is stable?
Which condition is NOT a predisposing factor for perineal edema?
Which condition is NOT a predisposing factor for perineal edema?
What does urinary retention after delivery suggest if urine output is less than 300cc on the initial void?
What does urinary retention after delivery suggest if urine output is less than 300cc on the initial void?
Flashcards are hidden until you start studying
Study Notes
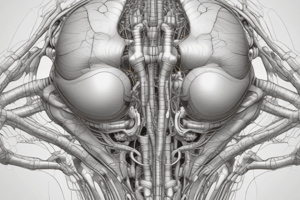
Coccyx
- The coccyx is the posterior portion of the pelvis, composed of five fused vertebrae.
- It joins the sacrum through the sacrococcygeal joint.
- During labor, the coccyx moves slightly backward to give more room for the fetal head to pass.
Pelvic Division
- The false pelvis is the upper portion of the iliac, supporting the uterus during pregnancy and directing the fetus to the true pelvis.
- The true pelvis forms the passageway for the fetus during labor.
Inlet
- Diagonal Conjugate: 12.5 cm diameter, measured internally from the midpoint of the sacral promontory to the lower margin of the symphysis pubis.
- Obstetric Conjugate: 11 cm, estimated by subtracting 1-1.5 cm from the diagonal conjugate.
- Conjugata Vera:
Pelvic Canal
- The canal curves at its half, below the ischial spine which helps control the speed of the fetal head descent.
- Rapid descent can lead to rupture of cerebral arteries.
- The pelvic cavity's snugness compresses the chest, aiding in expelling lung fluid and mucus.
- Interspinous diameter (smallest): 10 cm
- AP diameter at ischial spines: 11.5 cm
- Posterior sagittal diameter: 4.5 cm
Outlet
- The most important diameter of the outlet is the transverse diameter (bi-ischial) which is about 11.5 cm.
- Posterior sagittal diameter: 7.5 cm
Uterine Contractions
- Uterine contractions are the primary power in labor.
- They lead to physiological alterations including:
- Cervical dilatation: opening of the cervix from pinpoint to 10 cm.
- Cervical effacement: shortening and thinning of the cervical canal.
- Physiologic retraction ring: separation of the upper uterine segment from the lower, longer but thinner, passive segment.
- Bandl's ring: pathologic retraction ring formed in obstructed labor due to extreme thinning of the lower segment.
- Contractions are:
- Involuntary
- Rhythmical
- Intermittent
- Regular
- Painful
Pain in Labor
- The exact cause of pain during labor is unknown, but possible contributing factors include:
- Hypoxia due to circulatory stasis.
- Cervical stretching.
- Traction on the peritoneum and uterocervical supports.
- Compression of nerve ganglia.
- Emotional tension.
- Pressure on the bladder, bowel, or other pelvic structures.
Phases of Contractions
- Increment: period of increasing contraction, the longest phase.
- Acme: the peak of the contraction.
- Decrement: period of decreasing contraction.
Characteristics of Contractions
- Duration: length of a single contraction, from the increment to the decrement.
- Frequency: time interval between the beginning of one contraction to the beginning of the next.
- Interval of Rest: time from the end of one contraction to the start of the next, used for:
- Auscultating fetal heart rate.
- Checking maternal blood pressure.
- Delivering the head in extension.
Stages of Labor
- First Stage:*
- Begins with onset of regular contractions and ends with full cervical dilation (10 cm).
- Second Stage:*
- Begins with full cervical dilation and ends with the birth of the baby.
- The pressure of the fetus on the sacral nerves causes the mother to experience a pushing sensation.
- It consists of several phases:
- Descent: downward movement of the biparietal diameter of the fetal head into the pelvic inlet.
- Flexion: bending of the fetal head forward onto the chest.
- Internal Rotation: rotation of the occiput to a superior position, aligning the shoulders for entry into the inlet.
- Extension: birth of the head through extension.
- External Rotation: rotation of the head back to its original diagonal position, aligning the shoulders for delivery.
- Expulsion: delivery of the rest of the baby.
- Ritgen's Maneuver: an obstetrical procedure to control delivery of the fetal head and prevent lacerations.
- Third Stage:*
- Begins with the birth of the infant and ends with the delivery of the placenta.
- It comprises two phases:
- Placental separation
- Placental expulsion
- Fourth Stage:*
- First 2-3 hours after birth.
- Nursing responsibilities include:
- Transferring the patient to the bed.
- Providing perineal care, including applying ice packs.
- Transferring the patient to the recovery room.
- Monitoring vital signs and general condition.
- Observing for uterine atony or hemorrhage.
- Observing for any untoward effects from anesthesia.
- Orienting the patient to the surroundings.
- Allowing the patient time to rest.
- Encouraging the patient to drink fluids.
- Observing the bladder for distention.
- Evaluating the perineal area for edema and hematoma.
Anesthesia Options
- Lumbar Epidural: local anesthetic, provides continuous pain relief during labor and birth.
- Pudendal Block: local anesthetic, used for perineal anesthesia just before birth.
- Local Infiltration: local anesthetic, injected into the perineum for anesthesia during episiotomy.
- General Intravenous Anesthesia: administered IV, provides rapid anesthesia and recovery.
Episiotomy
- Surgical incision of the perineum to minimize tearing.
- Types:
- Midline
- Mediolateral
Lochia
- Lochia Rubra: dark red vaginal discharge, present for the first 2-3 days.
- Lochia Serosa: pinkish vaginal discharge, present from 3 to 10 days.
- Lochia Alba: whitish or yellowish-white vaginal discharge, present from day 10 to 21 or up to 6 weeks.
Postpartum Care
- Observe for chills, likely due to circulatory changes.
- Monitor vital signs, including temperature, every 15 minutes for the first hour.
- Assess for uterine atony or hemorrhage.
- Check for complications related to anesthesia.
- Provide patient education and comfort measures.
- Promote hydration.
- Monitor bladder distention.
Nursing Considerations
- Full bladder can displace the uterus and lead to postpartum hemorrhage.
- Be able to differentiate between a full bladder and a fundus.
- Provide perineal care to minimize edema and the development of hematomas.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.