Podcast
Questions and Answers
Which area is primarily anesthetized by the Greater Palatine Nerve Block?
Which area is primarily anesthetized by the Greater Palatine Nerve Block?
- Maxillary alveolar process
- Soft tissues covering the posterior portion of the hard palate (correct)
- Anterior portion of the hard palate
- Lingual surface of the mandible
What is the purpose of topical anesthesia in the Nasopalatine Nerve Block Technique?
What is the purpose of topical anesthesia in the Nasopalatine Nerve Block Technique?
- To provide adequate pain relief at the injection site. (correct)
- To numb the entire maxillary region.
- To speed up the administration of the anesthetic.
- To eliminate the need for pressure anesthesia.
What is the depth of penetration for the needle during a Greater Palatine Nerve Block?
What is the depth of penetration for the needle during a Greater Palatine Nerve Block?
- 3 mm
- 10 mm
- 7 mm
- 5 mm (correct)
Which palatal injection technique is specifically used for anesthesia of the anterior portion of the hard palate?
Which palatal injection technique is specifically used for anesthesia of the anterior portion of the hard palate?
Which landmark is critical for identifying the target area during the Greater Palatine Nerve Block?
Which landmark is critical for identifying the target area during the Greater Palatine Nerve Block?
What is the main advantage of using computer-controlled local anesthetic delivery systems in palatal injections?
What is the main advantage of using computer-controlled local anesthetic delivery systems in palatal injections?
What is the proper orientation of the needle bevel during the procedure?
What is the proper orientation of the needle bevel during the procedure?
What should be done if inadequate anesthesia occurs due to overlapping nerve supply?
What should be done if inadequate anesthesia occurs due to overlapping nerve supply?
Which of the following techniques provides only soft tissue anesthesia and does not affect pulpal anesthesia of the maxillary teeth?
Which of the following techniques provides only soft tissue anesthesia and does not affect pulpal anesthesia of the maxillary teeth?
How long should topical anesthetic remain in contact with palatal soft tissues before injection?
How long should topical anesthetic remain in contact with palatal soft tissues before injection?
How long should a clinician wait before commencing the procedure post-administration of anesthesia?
How long should a clinician wait before commencing the procedure post-administration of anesthesia?
What is the preferred method for aspirating during the Greater Palatine Nerve Block?
What is the preferred method for aspirating during the Greater Palatine Nerve Block?
Which nerves are anesthetized using the Palatal Infiltration Technique?
Which nerves are anesthetized using the Palatal Infiltration Technique?
What is a key component to ensure control over the needle during palatal injection?
What is a key component to ensure control over the needle during palatal injection?
What is the recommended volume for depositing local anesthetic during the Greater Palatine Nerve Block?
What is the recommended volume for depositing local anesthetic during the Greater Palatine Nerve Block?
Which technique offers pulpal anesthesia in addition to soft tissue anesthesia for maxillary teeth?
Which technique offers pulpal anesthesia in addition to soft tissue anesthesia for maxillary teeth?
Which area is NOT anesthetized by a maxillary nerve block?
Which area is NOT anesthetized by a maxillary nerve block?
What is a primary advantage of using the maxillary nerve block technique?
What is a primary advantage of using the maxillary nerve block technique?
Which alternative must be administered to achieve the same anesthesia as a maxillary nerve block?
Which alternative must be administered to achieve the same anesthesia as a maxillary nerve block?
What is a contraindication for performing a maxillary nerve block?
What is a contraindication for performing a maxillary nerve block?
What is the disadvantage associated with the High-Tuberosity Approach for nerve blocks?
What is the disadvantage associated with the High-Tuberosity Approach for nerve blocks?
Which of these components is NOT typically included in the armamentarium for the maxillary nerve block technique?
Which of these components is NOT typically included in the armamentarium for the maxillary nerve block technique?
Which group of structures does the maxillary nerve block influence during procedures?
Which group of structures does the maxillary nerve block influence during procedures?
What is a common misconception related to the maxillary nerve block technique?
What is a common misconception related to the maxillary nerve block technique?
What sensation is typically experienced on the side being injected during the procedure?
What sensation is typically experienced on the side being injected during the procedure?
Which test is used to determine the pulpal response during the procedure?
Which test is used to determine the pulpal response during the procedure?
Which complication is associated with the High-Tuberosity Approach?
Which complication is associated with the High-Tuberosity Approach?
What is a potential consequence of injecting local anesthetic into the orbit?
What is a potential consequence of injecting local anesthetic into the orbit?
What symptom indicates that the needle may have entered the nasal cavity during injection?
What symptom indicates that the needle may have entered the nasal cavity during injection?
Which of the following is NOT a sign of penetration of the Orbit?
Which of the following is NOT a sign of penetration of the Orbit?
Which outcome indicates correct administration of local anesthesia during treatment?
Which outcome indicates correct administration of local anesthesia during treatment?
What is a potential consequence of Abducens Nerve Block during the procedure?
What is a potential consequence of Abducens Nerve Block during the procedure?
What position should the patient be in for the Greater Palatine Approach?
What position should the patient be in for the Greater Palatine Approach?
How is the greater palatine foramen typically located?
How is the greater palatine foramen typically located?
What is the depth of penetration for the needle during the greater palatine nerve block?
What is the depth of penetration for the needle during the greater palatine nerve block?
What volume of local anesthetic is typically deposited during the greater palatine nerve block?
What volume of local anesthetic is typically deposited during the greater palatine nerve block?
What should be done if resistance is felt during the advancement of the needle into the greater palatine canal?
What should be done if resistance is felt during the advancement of the needle into the greater palatine canal?
How long should one wait after administering the maxillary nerve block before commencing the dental procedure?
How long should one wait after administering the maxillary nerve block before commencing the dental procedure?
What is the purpose of aspiration in two perpendicular planes during the maxillary nerve block?
What is the purpose of aspiration in two perpendicular planes during the maxillary nerve block?
What type of symptoms are typically associated with the V2-NB technique?
What type of symptoms are typically associated with the V2-NB technique?
Flashcards are hidden until you start studying
Study Notes
Palatal Anesthesia Techniques
- Nasopalatine Nerve Block Technique: Provides anesthesia to the anterior portion of the hard palate.
- Technique: Involves applying topical anesthesia, pressure anesthesia, and slow injection of anesthetic solution.
- Landmark: Incisive papilla.
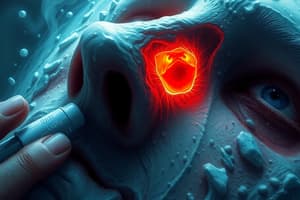
Greater Palatine Nerve Block (GPNB) Technique
- Areas Anesthetized: Soft tissues covering the posterior portion of the hard palate.
- Target Area: Greater palatine nerve as it passes through the greater palatine foramen.
- Landmark: Greater palatine foramen, located between the maxillary second and third molars, distal to the second molar.
- Procedure:
- Insert the needle at a right angle to the target area from the opposite side of the mouth.
- Orient the bevel towards the palatal soft tissues.
- Advance the needle until it contacts the palatine bone (approximately 5 mm deep).
- Aspirate in two planes and deposit 0.6 mL of anesthetic solution slowly.
- Wait 2-3 minutes before proceeding with dental procedures.
- Complications:
- Inadequate anesthesia of the maxillary first premolar: May be due to overlapping nerve supply from the nasopalatine nerve. Administer additional nasopalatine nerve block.
- Soft palate anesthesia: May be due to inadvertent anesthesia of the lesser palatine nerve. Reassure the patient and avoid swallowing until anesthesia subsides.
- Approach options:
- Intra-oral (high tuberosity approach)
- Intra-oral (greater palatine approach)
- Extra-oral approach
Maxillary Nerve Block (V2-NB)
- Alternatives: To achieve the same anesthetic distribution as a maxillary nerve block, posterior superior alveolar, anterior superior alveolar (infraorbital), nasopalatine, and greater palatine nerve blocks must be administered.
- Areas Anesthetized: Ipsilateral buccal and palatal mucoperiosteum, alveolar bone plates, periodontal tissues, pulps of all maxillary teeth, buccal skin of the lower eyelid, side of the nose, upper lip, and skin over cheek zygomaticofacial.
- Advantages:
- Provides a large field of anesthesia with long duration of action.
- Minimizes needle penetrations and volume of anesthetic solution.
- Disadvantages:
- Lack of hemostasis, may require additional infiltration with vasoconstrictor for surgical procedures.
- Indications:
- Comprehensive dental procedures requiring anesthesia of the entire maxillary division.
- When tissue inflammation or infection prevents other regional nerve blocks.
- Diagnostic and therapeutic procedures for trigeminal neuralgias involving the maxillary division.
- Contraindications:
- Inexperienced administrator.
- Uncooperative patient.
- Infection at the injection site.
- Increased risk of hemorrhage.
- Bony obstructions in the greater palatine canal, which may prevent access in 5-15% of cases.
- Technique:
- High-Tuberosity Approach: Less painful than the greater palatine approach but with a higher risk of hematoma.
- Greater Palatine Approach:
- Procedure:
- Patient opens their mouth widely, extends their neck and turns their head towards the operator.
- Locate the greater palatine foramen distal to the maxillary second molar (swab will fall into the depression).
- Apply pressure to the tissue over the foramen to induce ischemia.
- Inject anesthetic solution slowly into the greater palatine canal (30 mm depth) after aspirating in two planes.
- Wait 3-5 minutes before proceeding.
- Complications:
- Penetration of the orbit:
- Can occur if the needle penetrates too far into a smaller skull size.
- Risk of retrobulbar hemorrhage, proptosis, amaurosis, retrobulbar block, diplopia.
- Penetration of the nasal cavity:
- Can occur if the needle deviates medially during insertion.
- Signs: Air aspiration, anesthetic solution running down the throat.
- Penetration of the orbit:
- Procedure:
Signs and Symptoms of V2-NB Technique
- Subjective: Pressure behind the upper jaw, tingling and numbness of lower eyelid, side of the nose, and upper lip, numbness in teeth and buccal and palatal soft tissues.
- Objective: Absence of response to electrical pulp testing, probing, thermal testing, and pain during treatment
Complications of V2-NB Technique
- Hematoma: Related to puncture of the maxillary artery (high-tuberosity approach)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.