Podcast
Questions and Answers
What is one of the overall goals of oxygen therapy?
What is one of the overall goals of oxygen therapy?
- To maintain adequate tissue oxygenation (correct)
- To increase blood pressure
- To reduce the heart rate
- To cure chronic respiratory diseases
Which condition is indicated for oxygen therapy due to suspected hypoxemia?
Which condition is indicated for oxygen therapy due to suspected hypoxemia?
- Routine check for lung capacity
- Stable asthma without any complications
- Severe headache with no breathing issues
- Documented hypoxemia with PaO2 less than 60 mm Hg (correct)
Which of the following is a potential hazard of oxygen therapy?
Which of the following is a potential hazard of oxygen therapy?
- Contamination (correct)
- Increased respiratory rate
- Decreased oxygen saturation levels
- Enhanced immune response
In which situation might oxygen therapy be necessary post-operatively?
In which situation might oxygen therapy be necessary post-operatively?
What complication can occur with an FIO2 greater than 50%?
What complication can occur with an FIO2 greater than 50%?
What should be monitored closely to assess a patient's response to oxygen therapy?
What should be monitored closely to assess a patient's response to oxygen therapy?
What should be avoided to prevent oxygen toxicity?
What should be avoided to prevent oxygen toxicity?
What is the primary purpose of a high flow system in oxygen therapy?
What is the primary purpose of a high flow system in oxygen therapy?
Which device listed is NOT considered a high flow oxygen device?
Which device listed is NOT considered a high flow oxygen device?
What factor is essential when using an air entrainment mask for oxygen delivery?
What factor is essential when using an air entrainment mask for oxygen delivery?
What may be a concern when using oxygen hoods for infants?
What may be a concern when using oxygen hoods for infants?
Which statement about the air entrainment mask is accurate?
Which statement about the air entrainment mask is accurate?
What is the input flow range for an adult simple mask?
What is the input flow range for an adult simple mask?
What is a primary concern associated with prolonged exposure to high FIO2?
What is a primary concern associated with prolonged exposure to high FIO2?
What is the primary purpose of the bag in a partial rebreathing mask?
What is the primary purpose of the bag in a partial rebreathing mask?
Which mask prevents rebreathing using one-way valves?
Which mask prevents rebreathing using one-way valves?
Which condition is particularly affected by depression of ventilation due to supplemental O2?
Which condition is particularly affected by depression of ventilation due to supplemental O2?
What is the FiO2 range for a partial rebreathing mask?
What is the FiO2 range for a partial rebreathing mask?
What complication arises from excessive blood O2 levels in neonates?
What complication arises from excessive blood O2 levels in neonates?
Absorption atelectasis is likely to occur when FIO2 is above:
Absorption atelectasis is likely to occur when FIO2 is above:
Which of the following describes the input flow requirement for a nonrebreathing mask?
Which of the following describes the input flow requirement for a nonrebreathing mask?
What common issue can occur with reservoir masks?
What common issue can occur with reservoir masks?
What is a significant hazard associated with supplemental O2 in surgical settings?
What is a significant hazard associated with supplemental O2 in surgical settings?
Which delivery system is characterized by variable performance due to patient needs?
Which delivery system is characterized by variable performance due to patient needs?
Which statement about the nonrebreathing mask is true?
Which statement about the nonrebreathing mask is true?
How does a pulse demand oxygen delivery system function?
How does a pulse demand oxygen delivery system function?
What factor does NOT influence FiO2 in low-flow systems?
What factor does NOT influence FiO2 in low-flow systems?
What is the primary function of reservoir systems in oxygen delivery?
What is the primary function of reservoir systems in oxygen delivery?
What is the FiO2 range for a nonrebreathing mask?
What is the FiO2 range for a nonrebreathing mask?
Which of the following statements about high-flow systems is true?
Which of the following statements about high-flow systems is true?
What is the typical FiO2 range when using a nasal cannula?
What is the typical FiO2 range when using a nasal cannula?
What is a common complication associated with transtracheal catheters?
What is a common complication associated with transtracheal catheters?
At what flow rate does the use of a humidifier become necessary with a nasal cannula?
At what flow rate does the use of a humidifier become necessary with a nasal cannula?
Which of the following statements about nasal catheters is true?
Which of the following statements about nasal catheters is true?
What is one feature of reservoir systems designed to conserve oxygen?
What is one feature of reservoir systems designed to conserve oxygen?
What flow rate should a transtracheal catheter typically be set at?
What flow rate should a transtracheal catheter typically be set at?
How does a low inspiratory flow affect FiO2 delivered by low-flow systems?
How does a low inspiratory flow affect FiO2 delivered by low-flow systems?
What is a common troubleshooting issue with low-flow oxygen delivery systems?
What is a common troubleshooting issue with low-flow oxygen delivery systems?
What factor can cause a decrease in FiO2 for low-flow systems?
What factor can cause a decrease in FiO2 for low-flow systems?
What is the range of FiO2 provided by low-flow systems at a flow rate of 8 L/min?
What is the range of FiO2 provided by low-flow systems at a flow rate of 8 L/min?
Flashcards
Oxygen Therapy Goal
Oxygen Therapy Goal
Maintain adequate tissue oxygenation and minimize cardiopulmonary work.
Oxygen Therapy Indications
Oxygen Therapy Indications
Documented or suspected hypoxemia (low blood oxygen), severe trauma, acute MI, and post-op situations.
Hypoxemia Definition
Hypoxemia Definition
Low blood oxygen levels, usually measured by PaO2 < 60 mm Hg or SaO2 < 90% on room air, or below desirable range for a condition.
Oxygen Toxicity
Oxygen Toxicity
Signup and view all the flashcards
Absorption Atelectasis
Absorption Atelectasis
Signup and view all the flashcards
Ventilatory Depression
Ventilatory Depression
Signup and view all the flashcards
Retinopathy of Prematurity (ROP)
Retinopathy of Prematurity (ROP)
Signup and view all the flashcards
What is a major concern with long-term high-concentration oxygen therapy?
What is a major concern with long-term high-concentration oxygen therapy?
Signup and view all the flashcards
How can high oxygen levels affect COPD patients?
How can high oxygen levels affect COPD patients?
Signup and view all the flashcards
What is Retinopathy of Prematurity (ROP)?
What is Retinopathy of Prematurity (ROP)?
Signup and view all the flashcards
What breathing condition can be caused by high FIO2?
What breathing condition can be caused by high FIO2?
Signup and view all the flashcards
What is the main concern regarding oxygen therapy and fire?
What is the main concern regarding oxygen therapy and fire?
Signup and view all the flashcards
What are the types of oxygen delivery systems?
What are the types of oxygen delivery systems?
Signup and view all the flashcards
How does FiO2 change in low-flow systems?
How does FiO2 change in low-flow systems?
Signup and view all the flashcards
What is the primary limitation of low-flow systems?
What is the primary limitation of low-flow systems?
Signup and view all the flashcards
In what situations is a low-flow oxygen delivery system MOST appropriate?
In what situations is a low-flow oxygen delivery system MOST appropriate?
Signup and view all the flashcards
Nasal Cannula FiO2
Nasal Cannula FiO2
Signup and view all the flashcards
Nasal Cannula Flow Rates
Nasal Cannula Flow Rates
Signup and view all the flashcards
Nasal Cannula Humidifier
Nasal Cannula Humidifier
Signup and view all the flashcards
Nasal Catheter Use
Nasal Catheter Use
Signup and view all the flashcards
Transtracheal Catheter Placement
Transtracheal Catheter Placement
Signup and view all the flashcards
Transtracheal Catheter Advantages
Transtracheal Catheter Advantages
Signup and view all the flashcards
Low-Flow Oxygen Concentration
Low-Flow Oxygen Concentration
Signup and view all the flashcards
Low-Flow Concentration Factors
Low-Flow Concentration Factors
Signup and view all the flashcards
Low-Flow System Troubleshooting
Low-Flow System Troubleshooting
Signup and view all the flashcards
Reservoir Systems for Oxygen Conservation
Reservoir Systems for Oxygen Conservation
Signup and view all the flashcards
High Flow System
High Flow System
Signup and view all the flashcards
Air Entrainment Mask
Air Entrainment Mask
Signup and view all the flashcards
Oxygen Hoods
Oxygen Hoods
Signup and view all the flashcards
High Flow Devices
High Flow Devices
Signup and view all the flashcards
High Flow Oxygen and Humidity
High Flow Oxygen and Humidity
Signup and view all the flashcards
Simple Mask Flow Rate
Simple Mask Flow Rate
Signup and view all the flashcards
Simple Mask FiO2 Range
Simple Mask FiO2 Range
Signup and view all the flashcards
Partial Rebreathing Mask: What's Different?
Partial Rebreathing Mask: What's Different?
Signup and view all the flashcards
Partial Rebreathing Mask Flow Rate
Partial Rebreathing Mask Flow Rate
Signup and view all the flashcards
Partial Rebreathing Mask FiO2 Range
Partial Rebreathing Mask FiO2 Range
Signup and view all the flashcards
Nonrebreathing Mask: One-way Valves
Nonrebreathing Mask: One-way Valves
Signup and view all the flashcards
Nonrebreathing Mask Flow Rate
Nonrebreathing Mask Flow Rate
Signup and view all the flashcards
Nonrebreathing Mask FiO2 Range
Nonrebreathing Mask FiO2 Range
Signup and view all the flashcards
Troubleshooting Reservoir Systems
Troubleshooting Reservoir Systems
Signup and view all the flashcards
Pulse Demand Oxygen Delivery
Pulse Demand Oxygen Delivery
Signup and view all the flashcards
Study Notes
Chapter 42: Medical Gas Therapy - Low-Flow System
- Learning Objectives (1 of 3): Describe when oxygen therapy is needed, assess the need for oxygen therapy, describe precautions and complications associated with oxygen therapy, and select an appropriate oxygen delivery system.
Learning Objectives (2 of 3)
- Describe how to administer oxygen to adults, children, and infants.
- Describe how to identify and correct malfunctions of oxygen delivery systems.
- Assess and monitor a patient's response to oxygen therapy.
- Describe how and when to modify or recommend modifications to oxygen therapy.
Learning Objectives (3 of 3)
- Describe how to implement protocol-based oxygen therapy.
- Identify the indications, complications, and hazards of hyperbaric oxygen therapy.
- Identify when and how to administer specialty therapeutic gases.
Oxygen Therapy
- Overall goal: Maintain adequate tissue oxygenation. Minimize cardiopulmonary work.
- Clinical objectives: Correct documented or suspected acute hypoxemia, decrease symptoms of chronic hypoxemia, and decrease the workload imposed on the cardiopulmonary system by hypoxemia.
Assessing the Need for Oxygen Therapy - Indications
- Documented or suspected hypoxemia, as evidenced by:
- PaO2 less than 60 mm Hg
- SaO2 less than 90% in subjects breathing room air
- PaO2 or SaO2 below desirable ranges for a specific clinical situation.
- Severe trauma
- Acute myocardial infarction (MI)
- Post-operative conditions (e.g., post-anesthesia recovery)
Clinical Signs of Hypoxia
- Mild to moderate: Tachypnea, dyspnea, pale, tachycardia, mild hypertension, peripheral vasoconstriction, restlessness, disorientation, headaches, lassitude
- Severe: Tachypnea, dyspnea, cyanosis, tachycardia, eventual bradycardia or arrhythmia, hypertension and eventually hypotension, somnolence, confusion, distressed appearance, blurred/tunnel vision, loss of coordination, impaired judgment, slow reaction time, manic-depressive activity, coma
Hazards of Oxygen Therapy
- Absorption atelectasis: FiO2 > 50% may cause atelectasis due to oxygen replacing nitrogen.
- Ventilatory depression: PaO2 > 60 mmHg may depress ventilation with chronic hypercapnia.
- Retinopathy of Prematurity (ROP): Excessive blood oxygen levels cause retinal vasoconstriction and necrosis.
- Oxygen toxicity
- Fire hazard
- Contamination
Precautions & Hazards of Supplemental Oxygen (cont.)
- Oxygen toxicity: Primarily affects lungs and central nervous system. Determining factors include PO2 and exposure time. Prolonged high FiO2 may cause lung parenchyma infiltration.
- Avoiding oxygen toxicity: Limit 100% O2 exposure to less than 24 hours whenever possible.
- Depression of ventilation: Occurs commonly in COPD patients with chronic hypercapnia.
Precautions & Hazards of Supplemental Oxygen (cont.)
- Absorption atelectasis: Can occur with FiO2 > 0.50. Patients breathing small tidal volumes are at greatest risk.
Oxygen Therapy (cont.)
- Fire hazard: Fires in oxygen-enriched environments still occur. Practitioners in surgery suites and with hyperbaric oxygen therapy require heightened caution.
Oxygen Delivery Systems
- Types: Low-flow, reservoir, high-flow
- Clinical performance: Ultimately determines how the device is used. How much O2 can the device deliver, and if the delivered FiO2 remains consistent or varies with patient demands?
Low-Flow Systems
- Variable performance: FiO2 can vary depending on the patient's respiratory rate/pattern, the flow of gas from equipment, and the equipment reservoir.
- Doesn't meet full demand: Needs additional mixing with room air.
- Includes: Nasal cannula, nasal catheter (less common), and transtracheal catheters.
Nasal Cannula
- Delivers FiO2 of 0.24 to 0.40
- Used with flow rates of 1 to 8 L/min
- FiO2 depends on how much room air the patient inhales
- Typically well tolerated
Nasal Catheter
- Generally limited to short-term oxygen administration during procedures like bronchoscopy
- Delivers FiO2 of 0.22 to 0.45
- Should be replaced with a new one at least every 8 hours and is less common than the nasal cannula
Transtracheal Catheter
- Surgically placed in the trachea
- Uses less oxygen to achieve the same PaO2 as a nasal cannula
- Used with flow rates of 1 to 4 L/min
- Requires careful maintenance and cleaning
- Complications such as infection are possible
Performance Characteristics of Low-Flow Systems
- Provide oxygen concentrations ranging from 22% at 1 L/min to 60% at 15 L/min
- Ranges from 22% to 45% at 8L/min; this is the upper limit of flow comfort.
- Concentration delivered varies with air dilution
- Each L/min of nasal O2 increases FiO2 approximately 4%
Performance Characteristics of Low-Flow Systems (cont.)
- Increases FiO2: Higher oxygen input, mouth-closed breathing, low inspiratory flow, low tidal volume, slow breathing rate, small minute ventilation, long inspiratory time, and high I:E ratio
- Decreases FiO2: Lower oxygen input, mouth-open breathing, high inspiratory flow, high tidal volume, fast breathing rate, large minute ventilation, short inspiratory time, and low I:E ratio
Troubleshooting Low-Flow Systems
- Common problems include inaccurate flow, system leaks and obstructions, device displacement, and skin irritation. The problem of inaccurate flow is greater with low-flow flowmeters (≤3 L/min).
Reservoir Systems: Cannulas
- Designed to conserve oxygen (decreases oxygen use by 50-75%).
- Includes: Nasal reservoir, pendant reservoir.
- Humidification usually not needed
Reservoir Systems: Masks
- Most commonly used reservoir systems
- Three types: Simple mask, partial rebreathing mask, nonrebreathing mask
Simple Mask
- Input flow range for adult: 5 to 10 L/min
- At flow rates less than 5 L/min, mask volume acts as dead space causing carbon dioxide rebreathing.
- FiO2 range is 0.35 to 0.50.
- Air dilution is a factor during inspiration. The degree of air dilution impacts FiO2 variability depending on the oxygen flow input, mask volume/leakage, and the patient's breathing pattern.
Partial Rebreathing Masks
- Higher FiO2 capabilities than a simple mask due to reservoir bag
- No valves; O2 flows into the mask/directly to the patient during inhalation.
- During exhalation, O2 flows into the reservoir bag.
- Minimum input flow of 10 L/min to prevent bag collapse on inspiration
- FiO2 range is 0.40 to 0.70
Nonrebreathing Mask (1 of 2)
- More commonly used than the partial rebreathing mask.
- Minimum input flow requirement of 10L/min to prevent bag collapse on inhalation
- FiO2 range is 0.60 to 0.80
Nonrebreathing Mask (2 of 2)
- Prevents rebreathing with one-way valves
- Inspiratory valve on top of bag; expiratory valves cover the ports on the mask body.
- During inhalation, slight negative mask pressure closes the expiratory valves. This prevents air dilution. During expiration, valve action reverses the flow direction.
Troubleshooting Reservoir Systems
- Common problems include: Device displacement, system leaks and obstructions, improper flow adjustment, and skin irritation.
Oxygen Conservation Device
- Pulse demand oxygen delivery system delivers oxygen only during inspiration.
- Can be used with nasal cannulas and transtracheal oxygen catheters.
- Delivers flows equivalent to 1 to 5 L/min
High-Flow Systems
- Fixed performance: Provides flow rate adequate to meet patients' inspiratory needs.
- Provides relatively constant FiO2 by not diluting the patient's gas supply with room air. The flow should be at least 60 L/min.
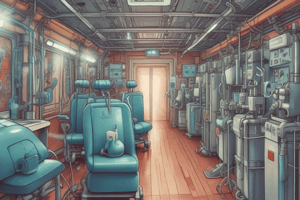
- Includes: Air entrainment mask, oxygen hoods, incubators, oxygen tents, high-volume aerosol and humidifiers via face masks/tracheostomy collars
High-Flow Systems (cont.)
- Delivers FiO2 from 0.24 to 1.0, regardless of patient's breathing patterns.
Air Entrainment Mask (Venturi Mask)
- Oxygen delivered through an orifice increases gas flow rate.
- Decrease in pressure on opposite side of the orifice causes air entrainment from the atmosphere.
- Oxygen mixes with air to obtain precise O2 concentrations
- Primary use: oxygen therapy for patients with COPD.
Air Entrainment Mask (cont.)
- Total flow from the mask is calculated by multiplying oxygen flow rate by the number of parts. Cannot be used with humidifiers (due to back pressure). Humidity may be added by attaching collars to air entrainment ports.
Oxygen Hoods
- Encloses the patient's head; generally best for infants.
- FiO2 should be monitored at the same level as the infant's nose.
- Noise levels inside the hood are a potential issue.
- Must analyze the O₂ level near the infant's head.
Incubators
- Regulate temperature, humidity, and FiO2 for infants.
- Include ports to regulate FiO2; open ports result in lower FiO2. FiO2 is significantly affected by opening chambers for nursing care.
Incubators (cont.)
- Hood inside the incubator may be necessary to maintain a consistent FiO2.
Oxygen Tents
- Encloses the patient with a frame and soft plastic material. Common for use in pediatrics, especially for croup.
- Oxygen is delivered from a high-flow aerosol system
- FiO2 is difficult to control due to the tent's large volume.
Oxygen Blenders and Mixers
- Mixes 50 psig oxygen and air to generate precise FiO2
- Alarms are used to signal failure in the compressed gas source.
- Pressure changes (10 psig) will trigger alarms.
Other Oxygen Delivery Devices
- Various devices exist for oxygen delivery
- Charts/tables are available to help with guidance in selecting appropriate equipment based on desired FiO2 level and stability.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.