Podcast
Questions and Answers
What is the primary hormone responsible for the formation of the corpus luteum?
What is the primary hormone responsible for the formation of the corpus luteum?
- Progesterone
- Follicle Stimulating Hormone (FSH)
- Estrogen
- Luteinizing Hormone (LH) (correct)
Which of the following is NOT a sign of ovulation?
Which of the following is NOT a sign of ovulation?
- Decreased sexual desire (correct)
- Breast tenderness
- Lower abdominal pain
- Increased body temperature
What occurs to the corpus luteum if fertilization does not happen?
What occurs to the corpus luteum if fertilization does not happen?
- It remains active for the entire menstrual cycle.
- It degenerates and forms the corpus albicans. (correct)
- It transforms back into a primordial follicle.
- It increases in size and secretes more progesterone.
During which phase does the endometrium reach a thickness of 6 mm?
During which phase does the endometrium reach a thickness of 6 mm?
What initiates menstruation?
What initiates menstruation?
What is the duration of the luteal (post-ovulation) phase?
What is the duration of the luteal (post-ovulation) phase?
During the proliferative phase, which hormone predominantly controls the thickening of the endometrium?
During the proliferative phase, which hormone predominantly controls the thickening of the endometrium?
What is the function of prostaglandins in the reproductive cycle?
What is the function of prostaglandins in the reproductive cycle?
What primarily stimulates the growth of ovarian follicles during the ovarian cycle?
What primarily stimulates the growth of ovarian follicles during the ovarian cycle?
During which phase does the follicle grow and undergo significant changes under FSH control?
During which phase does the follicle grow and undergo significant changes under FSH control?
What is the primary function of progesterone in the menstrual cycle?
What is the primary function of progesterone in the menstrual cycle?
Which structure forms after ovulation to secrete hormones during the luteal phase?
Which structure forms after ovulation to secrete hormones during the luteal phase?
What change occurs in the endometrium during the menstrual cycle?
What change occurs in the endometrium during the menstrual cycle?
What is the outcome of the mature Graffian follicle during ovulation?
What is the outcome of the mature Graffian follicle during ovulation?
What hormone is primarily responsible for stimulating ovulation?
What hormone is primarily responsible for stimulating ovulation?
What occurs at the end of the ovarian cycle if fertilization does not happen?
What occurs at the end of the ovarian cycle if fertilization does not happen?
What is the primary outcome for an oocyte if it is not fertilized within 24 hours?
What is the primary outcome for an oocyte if it is not fertilized within 24 hours?
What triggers menstruation after the secretory phase?
What triggers menstruation after the secretory phase?
Which physiological change occurs during the luteal phase?
Which physiological change occurs during the luteal phase?
What is a characteristic feature of the proliferative phase?
What is a characteristic feature of the proliferative phase?
What physiological process is primarily stimulated by LH after ovulation?
What physiological process is primarily stimulated by LH after ovulation?
Which feature characterizes the secretory phase?
Which feature characterizes the secretory phase?
What is the fate of the corpus luteum if fertilization occurs?
What is the fate of the corpus luteum if fertilization occurs?
Which of the following signs does NOT typically indicate ovulation?
Which of the following signs does NOT typically indicate ovulation?
What primarily governs the changes in the ovarian cycle leading up to ovulation?
What primarily governs the changes in the ovarian cycle leading up to ovulation?
Which structure is formed by the proliferation of follicular cells during the follicular phase?
Which structure is formed by the proliferation of follicular cells during the follicular phase?
The primary role of progesterone in the menstrual cycle is to:
The primary role of progesterone in the menstrual cycle is to:
What marks the end of the follicular phase in the ovarian cycle?
What marks the end of the follicular phase in the ovarian cycle?
Which hormone is primarily responsible for stimulating the growth of the uterine lining during the menstrual cycle?
Which hormone is primarily responsible for stimulating the growth of the uterine lining during the menstrual cycle?
The fate of the follicle after ovulation is typically to:
The fate of the follicle after ovulation is typically to:
What happens to the endometrium during the luteal phase of the menstrual cycle?
What happens to the endometrium during the luteal phase of the menstrual cycle?
During what phase is the follicular cavity filled with fluid containing estrogen?
During what phase is the follicular cavity filled with fluid containing estrogen?
What physical changes occur in the body as indicators of ovulation?
What physical changes occur in the body as indicators of ovulation?
Describe the fate of the corpus luteum if fertilization does not occur.
Describe the fate of the corpus luteum if fertilization does not occur.
What triggers the onset of the secretory phase of the menstrual cycle?
What triggers the onset of the secretory phase of the menstrual cycle?
What hormonal changes occur during the menstrual phase, and what are their effects?
What hormonal changes occur during the menstrual phase, and what are their effects?
How does estrogen affect the endometrium during the proliferative phase?
How does estrogen affect the endometrium during the proliferative phase?
What is the role of LH during the luteal phase of the menstrual cycle?
What is the role of LH during the luteal phase of the menstrual cycle?
Explain the process that occurs if fertilization happens during the menstrual cycle.
Explain the process that occurs if fertilization happens during the menstrual cycle.
What changes in the follicular cavity are associated with ovulation?
What changes in the follicular cavity are associated with ovulation?
Describe the primary function of follicle stimulating hormone (FSH) in the ovarian cycle.
Describe the primary function of follicle stimulating hormone (FSH) in the ovarian cycle.
What is the significance of the mature Graffian follicle during the ovulation phase?
What is the significance of the mature Graffian follicle during the ovulation phase?
Explain the hormonal changes that occur during the secretory phase of the menstrual cycle.
Explain the hormonal changes that occur during the secretory phase of the menstrual cycle.
What initiates the process of ovulation around the 14th day of the ovarian cycle?
What initiates the process of ovulation around the 14th day of the ovarian cycle?
What marks the transition from the follicular phase to ovulation in the ovarian cycle?
What marks the transition from the follicular phase to ovulation in the ovarian cycle?
Summarize the role of estrogen during the menstrual cycle.
Summarize the role of estrogen during the menstrual cycle.
What happens to ovarian follicles that do not undergo ovulation?
What happens to ovarian follicles that do not undergo ovulation?
Identify the primary roles of thetheca interna and theca externa in the mature Graffian follicle.
Identify the primary roles of thetheca interna and theca externa in the mature Graffian follicle.
What is the main hormonal trigger for the growth of ovarian follicles during the follicular phase?
What is the main hormonal trigger for the growth of ovarian follicles during the follicular phase?
Which hormone is dominant during the secretory phase of the menstrual cycle?
Which hormone is dominant during the secretory phase of the menstrual cycle?
Describe the role of the corpus luteum if fertilization occurs.
Describe the role of the corpus luteum if fertilization occurs.
What characterizes the onset of ovulation in the ovarian cycle?
What characterizes the onset of ovulation in the ovarian cycle?
What changes does estrogen induce in the endometrium during the proliferative phase?
What changes does estrogen induce in the endometrium during the proliferative phase?
How does the absence of fertilization affect the fate of the corpus luteum?
How does the absence of fertilization affect the fate of the corpus luteum?
What is the fate of the follicle that successfully undergoes ovulation?
What is the fate of the follicle that successfully undergoes ovulation?
Explain the changes in the follicle that occur during the follicular phase leading up to ovulation.
Explain the changes in the follicle that occur during the follicular phase leading up to ovulation.
What hormonal changes occur in the luteal phase and how do they affect the endometrium?
What hormonal changes occur in the luteal phase and how do they affect the endometrium?
Explain the role of prostaglandins in the contraction of theca externa during ovulation.
Explain the role of prostaglandins in the contraction of theca externa during ovulation.
How does the fate of the corpus luteum differ based on fertilization status?
How does the fate of the corpus luteum differ based on fertilization status?
Describe the physiological changes that signal ovulation beyond hormonal factors.
Describe the physiological changes that signal ovulation beyond hormonal factors.
What events lead to the initiation of menstruation following the secretory phase?
What events lead to the initiation of menstruation following the secretory phase?
How does estrogen influence the endometrium during the proliferative phase of the menstrual cycle?
How does estrogen influence the endometrium during the proliferative phase of the menstrual cycle?
What is the significance of the corpus hemorrhagicum following ovulation?
What is the significance of the corpus hemorrhagicum following ovulation?
Explain how LH contributes to the formation of the corpus luteum after ovulation.
Explain how LH contributes to the formation of the corpus luteum after ovulation.
What marks the beginning of the ovarian cycle and what is its duration?
What marks the beginning of the ovarian cycle and what is its duration?
How does luteinizing hormone (LH) contribute to the reproductive cycle?
How does luteinizing hormone (LH) contribute to the reproductive cycle?
Describe the fate of the oocyte after ovulation if fertilization does not occur.
Describe the fate of the oocyte after ovulation if fertilization does not occur.
What physiological changes are primarily stimulated by estrogen during the proliferative phase?
What physiological changes are primarily stimulated by estrogen during the proliferative phase?
What event signifies the transition from the follicular phase to ovulation in the ovarian cycle?
What event signifies the transition from the follicular phase to ovulation in the ovarian cycle?
What happens to the corpus luteum if fertilization occurs?
What happens to the corpus luteum if fertilization occurs?
Which hormones control the secretory phase of the menstrual cycle and what do they promote?
Which hormones control the secretory phase of the menstrual cycle and what do they promote?
Describe the primary role of follicle stimulating hormone (FSH) in the ovarian cycle.
Describe the primary role of follicle stimulating hormone (FSH) in the ovarian cycle.
What hormonal changes occur in the corpus luteum if fertilization does not occur?
What hormonal changes occur in the corpus luteum if fertilization does not occur?
Explain how the endometrium is affected during the menstrual phase.
Explain how the endometrium is affected during the menstrual phase.
Describe the physiological role of progesterone during the secretory phase.
Describe the physiological role of progesterone during the secretory phase.
What signs indicate the onset of ovulation based on hormonal changes?
What signs indicate the onset of ovulation based on hormonal changes?
What consequences arise from the degeneration of the corpus luteum?
What consequences arise from the degeneration of the corpus luteum?
How does the formation of corpus hemorrhagicum relate to the post-ovulation phase?
How does the formation of corpus hemorrhagicum relate to the post-ovulation phase?
Discuss the fate of the oocyte if it is not fertilized within 24 hours.
Discuss the fate of the oocyte if it is not fertilized within 24 hours.
What role does estrogen play during the proliferative phase of the menstrual cycle?
What role does estrogen play during the proliferative phase of the menstrual cycle?
Flashcards are hidden until you start studying
Study Notes
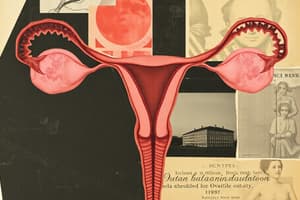
Ovarian Cycle
- Cyclic changes in the ovary that occur each month, starting at puberty and ending at menopause.
- Hormonal Control:
- Follicle Stimulating Hormone (FSH): Stimulates growth of ovarian follicles and the production of Estrogen by the follicles.
- Luteinizing Hormone (LH): Stimulates ovulation and the formation of the Corpus Luteum.
Phases of the Ovarian Cycle
- Follicular ("Pre-Ovulation") Phase: This lasts for 14 days, under the influence of FSH.
- Primordial Follicle: Contains a primary oocyte surrounded by a layer of follicular cells.
- Growing Follicle: The oocyte is surrounded by a Zona Pellucida, and the follicular cells proliferate.
- Mature Graffian Follicle: This develops from the growing follicle and contains the oocyte surrounded by a Zona Pellucida, Corona Radiate, and Cumulus Oophorus. The follicle capsule consists of three layers: Theca Externa (outer fibrous layer), Theca Interna (inner vascular layer) and Granulosa cells. The follicular cavity is filled with fluid containing Estrogen. The mature follicle undergoes ovulation at the 14th day, liberating the oocyte.
Ovulation
- The mature Graffian follicle ruptures releasing the oocyte.
- Occurs around the 14th day of the cycle.
- Caused by: Prostaglandins, LH, and increased tension within the follicular cavity.
- The oocyte is either fertilized by sperm or degenerates within 24 hours.
- Signs of Ovulation: Increased body temperature, heightened senses, breast tenderness, lower abdominal pain, and increased sexual desire.
Luteal ("Post-Ovulation") Phase:
- Lasts for 14 days under the influence of LH.
- Formation of Corpus Luteum: The ruptured follicle fills with blood forming the Corpus Hemorrhagicum, then the follicular cells are stimulated by LH to fill with yellow pigment forming the Corpus Luteum.
- Function of Corpus Luteum: Secretes Progesterone.
- Fate of the Corpus Luteum:
- If fertilization occurs, the Corpus Luteum increases in size and remains active until the 4th month.
- If fertilization does not occur, the Corpus Luteum shrinks and forms a Corpus Albicans.
Menstrual Cycle:
- Cyclic changes in the endometrium (lining of the uterus) that occur every month, starting at puberty and ending at menopause.
Phases of the Menstrual Cycle:
-
Menstrual Phase:
- Duration: 3-5 days.
- Cause: Degeneration of the Corpus Luteum leads to a decrease in Progesterone, causing spasm of the arteries, ischemia (restriction of blood flow) and degeneration of the endometrium.
- Features: This phase involves the shedding of 50 ml of unclotted blood containing an unfertilized ovum, compact and spongy layers of the endometrium.
-
Proliferative Phase: Corresponds to the Follicular phase of the Ovarian Cycle.
- Duration: 6th to 14th day.
- Hormonal control: Estrogen secreted by the ovarian follicles.
- Features: Proliferation of the endometrium and its thickness increasing to 3 mm.
-
Secretory Phase: Corresponds to the Luteal phase of the Ovarian Cycle.
- Duration: 14th to 28th day.
- Hormonal Control: Progesterone from the Corpus Luteum.
- Features:
- Increased thickness of the endometrium to 6 mm.
- Glands are filled with secretions and there is increased vascularity in the endometrium.
-
Fate of the Secretory Phase:
- If fertilization occurs: The Corpus Luteum grows, leading to increased Progesterone. This causes dilation of arteries, increased thickness of the endometrium, and increased secretions.
- If fertilization does not occur: The Corpus Luteum degenerates, resulting in decreased Progesterone, causing spasm of the arteries, degeneration of the endometrium, and finally menstruation.
Ovarian Cycle
- Cyclic changes in the ovary every lunar month
- Begins at puberty and continues until menopause
- Controlled by hormones: Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH)
- FSH: stimulates growth of ovarian follicles and estrogen production
- LH: stimulates ovulation and formation of corpus luteum
Phases of Ovarian Cycle
Follicular Phase ("pre-ovulation" phase)
- Lasts for 14 days under the control of FSH
- Primordial Follicles: primary oocyte surrounded by a layer of follicular cells
- Growing Follicle: zona pellucida surrounds the oocyte and follicular cells proliferate
- Mature Graffian Follicle:
- Oocyte surrounded by zona pellucida, corona radiate, and cumulus oophorus
- Capsule is formed from theca externa (outer fibrous layer), theca interna (inner vascular layer), and granulosa cells
- Follicular cavity is filled with fluid containing estrogen
- Fate of Follicle: undergoes ovulation on the 14th day, liberating the oocyte
Ovulation
- Rupture of the mature Graffian follicle
- Occurs around the 14th day
- Causes: prostaglandins, LH, and increased tension in the follicular cavity
- Fate of Oocyte: fertilized by sperm or degenerates within 24 hours if not fertilized
- Signs of Ovulation: increased body temperature, heightened senses, breast tenderness, lower abdominal pain, and increased sexual desire
Luteal Phase ("post-ovulation" phase)
- Lasts for 14 days under the effect of LH
- Formation of Corpus Luteum:
- After ovulation, the ruptured follicle fills with blood, forming corpus hemorrhagicum
- LH causes follicular cells to be filled with yellow pigment, forming the corpus luteum
- Function of Corpus Luteum: secretes progesterone
- Fate of Corpus Luteum:
- If fertilization occurs, the corpus luteum increases in size and remains active until the 4th month
- If fertilization doesn't occur, the corpus luteum decreases in size and forms corpus albicans
Menstrual Cycle
- Cyclic changes in the endometrium every lunar month
- Begins at puberty and continues until menopause
- Controlled by hormones: estrogen and progesterone
- Estrogen: stimulates proliferation of the endometrium
- Progesterone: stimulates secretory changes in the endometrium
Phases of Menstrual Cycle
Menstrual Phase
- Duration: 3-5 days
- Causes: degeneration of corpus luteum, decrease in progesterone, spasm of arteries, ischemia, and degeneration of the endometrium
- Features: 50 ml of unclotted blood containing an unfertilized ovum and compact and spongy layers of the endometrium
Proliferative Phase (corresponds to the Follicular phase of the ovarian cycle)
- Duration: 6th to 14th day
- Hormonal Control: estrogen secreted by ovarian follicles
- Features: proliferation of the endometrium, increasing its thickness to 3 mm
Secretory Phase (corresponds to the Luteal phase of the ovarian cycle)
- Duration: 14th to 28th day
- Hormonal Control: progesterone from the corpus luteum
- Features: increased thickness of the endometrium (6 mm), glands filled with secretions, and marked increase in vascularity of the endometrium
- Fate of Secretory Phase:
- If fertilization occurs, the corpus luteum grows, increasing progesterone, dilating arteries, increasing the thickness of the endometrium and secretions
- If fertilization doesn't occur, the corpus luteum degenerates, decreasing progesterone, causing spasm of arteries, degeneration of the endometrium, and ultimately, menstruation
Ovarian Cycle
- Cyclic changes in the ovary every lunar month
- Begins at puberty and ends at menopause
- Controlled by Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH)
- FSH stimulates the growth of ovarian follicles and estrogen production
- LH stimulates ovulation and the formation of the corpus luteum
Menstrual Cycle
- Cyclic changes in the endometrium every lunar month
- Begins at puberty and ends at menopause
- Controlled by estrogen and progesterone
- Estrogen stimulates the proliferation of the endometrium
- Progesterone stimulates secretory changes in the endometrium
Phases of the Ovarian Cycle
Follicular Phase (Pre-ovulation)
- Lasts for approximately 14 days
- Controlled by FSH
- Stages of follicle development:
- Primordial Follicles: Contains a primary oocyte surrounded by a layer of follicular cells
- Growing Follicles: Zona pellucida surrounds the oocyte, follicular cells proliferate
- Mature Graffian Follicle: Contains the oocyte surrounded by the zona pellucida, corona radiate, and cumulus oophorus; capsule is formed by the theca externa, theca interna, and granulosa cells; follicular cavity is filled with fluid containing estrogen
- The mature follicle undergoes ovulation on day 14 to release the oocyte
Ovulation
- The rupture of the mature Graffian follicle
- Occurs around day 14
- Triggered by:
- Prostaglandins: stimulate contraction of the theca externa
- LH: hormonal drive
- Increased tension of the follicular cavity
- Oocyte is fertilized by sperm or degenerates within 24 hours if not fertilized
Signs of Ovulation
- Increase in body temperature
- Heightened senses
- Breast tenderness
- Lower abdominal pain
- Increased sexual desire
Luteal Phase (Post-ovulation)
- Lasts for 14 days (under effect of LH)
- Formation of the corpus luteum:
- The ruptured follicle fills with blood after ovulation, forming the corpus hemorrhagicum.
- LH causes the follicular cells to fill with yellow pigment, forming the corpus luteum.
- Function of the Corpus Luteum: Secretes progesterone
- Fate of the Corpus Luteum:
- If fertilization occurs: Corpus luteum increases in size and remains active until the 4th month of pregnancy.
- If fertilization doesn't occur: Corpus luteum decreases in size and forms the corpus albicans.
Phases of the Menstrual Cycle
Menstrual Phase
- Duration: 3-5 days
- Causes: Degeneration of corpus luteum leads to a decrease in progesterone, causing spasm of arteries, ischemia, and degeneration of the endometrium.
- Features: Discharge of 50 ml of unclotted blood containing an unfertilized ovum and the compact and spongy layers of the endometrium.
Proliferative Phase
- Duration: 6th day to the 14th day
- Hormonal Control: Estrogen secreted by the ovarian follicles
- Features: Proliferation of the endometrium, which becomes 3 mm thick.
Secretory Phase
- Duration: 14th day to the 28th day
- Hormonal Control: Progesterone from the corpus luteum
- Features: Increase in the thickness of the endometrium (6 mm), glands are filled with secretions, and marked increase in vascularity of the endometrium.
- Fate of the Secretory Phase:
- If fertilization occurs; corpus luteum grows, increasing progesterone levels, leading to dilatation of arteries, increased thickening of the endometrium, and increased secretions.
- If fertilization doesn't occur: Degeneration of the corpus luteum leads to a decrease in progesterone, causing spasm of arteries, and degeneration of the endometrium causing menstruation.
Ovarian Cycle
- Cyclic changes in the ovary that occur every lunar month
- Begins at puberty and ends at menopause
- Controlled by FSH (follicle-stimulating hormone) and LH (luteinizing hormone)
Follicular Phase
- Lasts for 14 days and is controlled by FSH
- Primordial Follicles: primary oocyte surrounded by follicular cells
- Growing Follicle: zona pellucida surrounds the oocyte; follicular cells proliferate
- Mature Graffian Follicle: oocyte surrounded by zona pellucida, corona radiata, and cumulus oophorus; capsule formed of theca externa, theca interna, and granulosa cells; follicular cavity filled with estrogen-containing fluid
Ovulation
- Rupture of mature Graffian follicle
- Occurs around the 14th day of the cycle
- Caused by prostaglandins, LH, and increased tension of the follicular cavity
- Oocyte is either fertilized by sperm or degenerates within 24 hours
Luteal Phase
- Lasts for 14 days and is controlled by LH
- Corpus Luteum Formation: ruptured follicle filled with blood, forming corpus hemorrhagicum; LH causes follicular cells to fill with yellow pigment, forming the corpus luteum
- Corpus Luteum Function: secretes progesterone
- Corpus Luteum Fate: if fertilization occurs, it increases in size and remains active until the 4th month; if not, it decreases in size and forms a corpus albicans
Menstrual Cycle
- Cyclic changes of the endometrium that occur every lunar month
- Begins at puberty and ends at menopause
- Controlled by estrogen and progesterone
Menstrual Phase
- Duration: 3-5 days
- Causes: degeneration of corpus luteum, decreased progesterone, and arterial spasm, leading to ischemia and degeneration of the endometrium
- Features: discharge of 50 ml of unclotted blood containing an unfertilized ovum and compact and spongy layers of endometrium
Proliferative Phase
- Corresponds to the Follicular Phase of the ovarian cycle
- Duration: 6th day to 14th day
- Hormonal Control: estrogen secreted by ovarian follicles
- Features: proliferation of the endometrium, increasing its thickness to 3 mm
Secretory Phase
- Corresponds to the Luteal Phase of the ovarian cycle
- Duration: 14th day to 28th day
- Hormonal Control: progesterone from the corpus luteum
- Features: increased thickness of the endometrium (6 mm), glands filled with secretions, and increased vascularity of the endometrium
- Fate: if fertilization occurs, corpus luteum growth, increased progesterone, arterial dilation, increased thickness of endometrium, and increased secretions; if fertilization doesn't occur, degeneration of the corpus luteum, decreased progesterone, arterial spasm, and degeneration of the endometrium, leading to menstruation.
Ovarian Cycle
- The ovarian cycle is a monthly series of changes in the ovary, occurring from puberty to menopause.
- Follicle-stimulating hormone (FSH) stimulates the growth of ovarian follicles and the production of estrogen.
- Luteinizing hormone (LH) triggers ovulation and the formation of the corpus luteum.
Menstrual Cycle
- The menstrual cycle is a monthly series of changes in the endometrium, the lining of the uterus, occurring from puberty to menopause.
- Estrogen promotes the proliferation of the endometrium.
- Progesterone stimulates secretory changes in the endometrium, preparing it for a potential pregnancy.
Phases of the Ovarian Cycle
Follicular Phase
- The follicular phase lasts for 14 days and is controlled by FSH.
- Primordial follicles contain a primary oocyte surrounded by follicular cells.
- As a follicle grows, a zona pellucida forms around the oocyte, and follicular cells proliferate.
- The mature Graffian follicle contains the oocyte surrounded by the zona pellucida, corona radiate, and cumulus oophorus.
- The capsule of the Graffian follicle consists of the theca externa (outer fibrous layer), theca interna (inner vascular layer), and granulosa cells.
- The follicular cavity is filled with fluid containing estrogen.
- The Graffian follicle undergoes ovulation on day 14, releasing the oocyte.
Ovulation
- Ovulation is the rupture of the mature Graffian follicle, releasing the oocyte.
- Ovulation occurs around day 14.
- Factors contributing to ovulation include prostaglandins, LH, and increased follicular fluid tension.
- If the oocyte is not fertilized, it degenerates within 24 hours.
Signs of Ovulation
- Elevated body temperature
- Heightened senses
- Breast tenderness
- Lower abdominal pain
- Increased sexual desire
Luteal Phase
- The luteal phase lasts for 14 days and is influenced by LH.
- After ovulation, the ruptured follicle fills with blood, becoming the corpus hemorrhagicum.
- LH stimulates the follicular cells, leading to their filling with yellow pigment and forming the corpus luteum.
- The corpus luteum secretes progesterone.
- If fertilization occurs, the corpus luteum grows and remains active until the fourth month of pregnancy.
- If fertilization does not occur, the corpus luteum degenerates and becomes the corpus albicans.
Phases of the Menstrual Cycle
Menstrual Phase
- The menstrual phase lasts for 3 to 5 days.
- Degeneration of the corpus luteum reduces progesterone levels, causing a spasm of arteries.
- Reduced blood flow to the endometrium leads to its ischemia and degeneration.
- The menstrual flow consists of approximately 50 ml of unclotted blood containing an unfertilized ovum and the compact and spongy layers of the endometrium.
Proliferative Phase
- The proliferative phase corresponds to the follicular phase of the ovarian cycle and lasts from day 6 to 14.
- Estrogen secreted by the ovarian follicles stimulates proliferation of the endometrium, increasing its thickness to 3 mm.
Secretory Phase
- The secretory phase corresponds to the luteal phase of the ovarian cycle and lasts from day 14 to 28.
- Progesterone secreted by the corpus luteum causes further thickening of the endometrium (up to 6 mm), stimulates glandular secretion, and increases vascularity.
- If fertilization occurs, the corpus luteum continues to secrete progesterone, supporting the development of the endometrium.
- If fertilization does not occur, the corpus luteum regresses, leading to a decrease in progesterone, resulting in a spasm of arteries and degeneration of the endometrium, ultimately causing menstruation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.