Podcast
Questions and Answers
What is an important aspect to assess when inspecting the auricles and surrounding tissue?
What is an important aspect to assess when inspecting the auricles and surrounding tissue?
- Asymmetry (correct)
- Deformities (correct)
- All of the above
- Skin Lesions (correct)
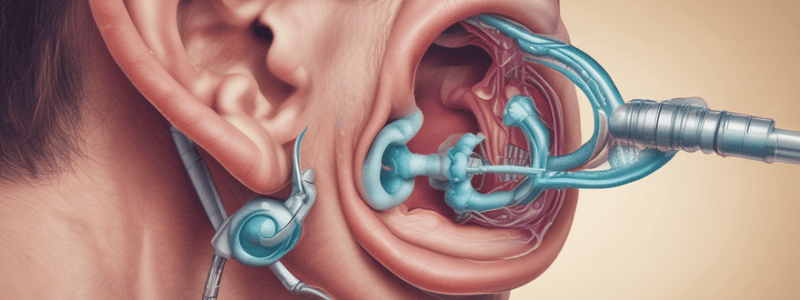
What should the healthcare provider do when using an otoscope?
What should the healthcare provider do when using an otoscope?
- Lift the auricle up and back (correct)
- Hold the otoscope with all fingers
- Insert the speculum sharply into the ear canal
- Position the patient's head so you can't see through the otoscope
What should the healthcare provider ask about during the subjective history?
What should the healthcare provider ask about during the subjective history?
- History of frequent ear infections (correct)
- History of frequent colds
- History of allergic reactions
- History of surgery to the nose
What should the healthcare provider assess for when palpating the auricle, tragus, and mastoid?
What should the healthcare provider assess for when palpating the auricle, tragus, and mastoid?
What should the healthcare provider ask the patient about during the review of systems?
What should the healthcare provider ask the patient about during the review of systems?
What is the correct direction to insert the speculum into the ear canal?
What is the correct direction to insert the speculum into the ear canal?
When should the healthcare provider lift the auricle up and back?
When should the healthcare provider lift the auricle up and back?
How should the healthcare provider hold the otoscope?
How should the healthcare provider hold the otoscope?
What is the normal color of the tympanic membrane?
What is the normal color of the tympanic membrane?
What is the purpose of the Weber test?
What is the purpose of the Weber test?
What is a common finding in serous otitis media?
What is a common finding in serous otitis media?
What is a characteristic of the eustachian tube in infants and children?
What is a characteristic of the eustachian tube in infants and children?
What is a common finding in otitis externa?
What is a common finding in otitis externa?
What is a characteristic of cerumen in older adults?
What is a characteristic of cerumen in older adults?
What is the purpose of the Rinne test?
What is the purpose of the Rinne test?
What is a characteristic of the tympanic membrane in older adults?
What is a characteristic of the tympanic membrane in older adults?
What is a common finding in bacterial otitis media?
What is a common finding in bacterial otitis media?
What is the purpose of inspecting the ear canal?
What is the purpose of inspecting the ear canal?
What is the main reason for the lens to lose elasticity and cannot change shape to accommodate for near vision in older adults?
What is the main reason for the lens to lose elasticity and cannot change shape to accommodate for near vision in older adults?
What is a characteristic of the lens in older adults that can lead to vision problems?
What is a characteristic of the lens in older adults that can lead to vision problems?
What is a type of deposit that can accumulate under the retina in older adults, but does not affect vision?
What is a type of deposit that can accumulate under the retina in older adults, but does not affect vision?
What is a common finding in sudden increases in intracranial pressure, severe hypertension, and diabetes?
What is a common finding in sudden increases in intracranial pressure, severe hypertension, and diabetes?
What is a characteristic of the optic disc in glaucoma?
What is a characteristic of the optic disc in glaucoma?
What can cause floaters to appear in the vitreous humor?
What can cause floaters to appear in the vitreous humor?
What is a characteristic of age-related macular degeneration?
What is a characteristic of age-related macular degeneration?
What can cause visual disturbances, headaches, and nausea in patients?
What can cause visual disturbances, headaches, and nausea in patients?
What is the leading cause of vision loss and blindness among older adults?
What is the leading cause of vision loss and blindness among older adults?
What is the most common type of Age-related Macular Degeneration?
What is the most common type of Age-related Macular Degeneration?
What is the characteristic symptom of Wet (Neovascular) Age-related Macular Degeneration?
What is the characteristic symptom of Wet (Neovascular) Age-related Macular Degeneration?
What is the cause of Glaucoma?
What is the cause of Glaucoma?
What is the characteristic symptom of Chronic-open Angle Glaucoma?
What is the characteristic symptom of Chronic-open Angle Glaucoma?
What is the characteristic symptom of Cataracts?
What is the characteristic symptom of Cataracts?
What is a risk factor for Chronic-open Angle Glaucoma?
What is a risk factor for Chronic-open Angle Glaucoma?
What is the characteristic effect of Age-related Macular Degeneration on central vision?
What is the characteristic effect of Age-related Macular Degeneration on central vision?
What is the purpose of using oblique lighting when inspecting the cornea and lens?
What is the purpose of using oblique lighting when inspecting the cornea and lens?
What is the normal size of the pupils?
What is the normal size of the pupils?
What is anisocoria?
What is anisocoria?
What is the purpose of the corneal light reflex test?
What is the purpose of the corneal light reflex test?
What is the normal result of the corneal light reflex test?
What is the normal result of the corneal light reflex test?
What is the purpose of the direct and consensual pupillary light reflex test?
What is the purpose of the direct and consensual pupillary light reflex test?
What is the difference between miosis and mydriasis?
What is the difference between miosis and mydriasis?
What is the purpose of the accommodation test?
What is the purpose of the accommodation test?
What is the normal appearance of retinal vessels?
What is the normal appearance of retinal vessels?
What is the A:V Ratio in normal retinal vessels?
What is the A:V Ratio in normal retinal vessels?
What happens to the retinal vessels as they move away from the optic disc?
What happens to the retinal vessels as they move away from the optic disc?
What is the phenomenon where a small artery (arteriole) is seen crossing a small vein (venule), which results in the compression of the vein with bulging on either side of the crossing?
What is the phenomenon where a small artery (arteriole) is seen crossing a small vein (venule), which results in the compression of the vein with bulging on either side of the crossing?
What is the medical condition where the optic nerve at the back of the eye becomes swollen due to a buildup of pressure in or around the brain?
What is the medical condition where the optic nerve at the back of the eye becomes swollen due to a buildup of pressure in or around the brain?
How many sets of retinal vessels are normally present in each quadrant?
How many sets of retinal vessels are normally present in each quadrant?
What is the location of the superior nasal vessels?
What is the location of the superior nasal vessels?
What is the characteristic of retinal vessels that allows them to be identified?
What is the characteristic of retinal vessels that allows them to be identified?
What type of refractive error is characterized by impaired close vision?
What type of refractive error is characterized by impaired close vision?
What is the term for the cloudy or opaque natural lens in the eye that affects vision?
What is the term for the cloudy or opaque natural lens in the eye that affects vision?
What is the term for the yellowish deposits that can accumulate in the macula of the eye, leading to age-related macular degeneration?
What is the term for the yellowish deposits that can accumulate in the macula of the eye, leading to age-related macular degeneration?
What is the term for the progressive damage to the optic nerve that can lead to vision loss?
What is the term for the progressive damage to the optic nerve that can lead to vision loss?
What is the term for the examination of the eye using a Snellen chart to assess visual acuity?
What is the term for the examination of the eye using a Snellen chart to assess visual acuity?
What is the term for the measurement of the pressure inside the eye?
What is the term for the measurement of the pressure inside the eye?
What is the term for the condition characterized by a cloudy or opaque natural lens in the eye that affects vision?
What is the term for the condition characterized by a cloudy or opaque natural lens in the eye that affects vision?
What is the term for the age-related condition characterized by damage to the macula of the eye, leading to central vision loss?
What is the term for the age-related condition characterized by damage to the macula of the eye, leading to central vision loss?
What is the purpose of inspecting the iris during an eye exam?
What is the purpose of inspecting the iris during an eye exam?
What is the abnormal condition where the pupils are unequal in size?
What is the abnormal condition where the pupils are unequal in size?
What is the purpose of the Corneal Light Reflex test?
What is the purpose of the Corneal Light Reflex test?
What is the normal result of the Corneal Light Reflex test?
What is the normal result of the Corneal Light Reflex test?
What is the term for the abnormal constriction of the pupils?
What is the term for the abnormal constriction of the pupils?
What is the purpose of the Direct and Consensual Pupillary Light Reflex test?
What is the purpose of the Direct and Consensual Pupillary Light Reflex test?
What is the term for the abnormal dilation of the pupils?
What is the term for the abnormal dilation of the pupils?
What is the purpose of inspecting the pupils during an eye exam?
What is the purpose of inspecting the pupils during an eye exam?
What should the conjunctiva appear as during inspection?
What should the conjunctiva appear as during inspection?
What is the purpose of the direct and consensual pupillary light reflex test?
What is the purpose of the direct and consensual pupillary light reflex test?
What is being assessed during the extraocular muscle assessment?
What is being assessed during the extraocular muscle assessment?
What is being evaluated during the lacrimal apparatus evaluation?
What is being evaluated during the lacrimal apparatus evaluation?
What is the purpose of the corneal light reflex test?
What is the purpose of the corneal light reflex test?
What should the healthcare provider do when inspecting the conjunctiva and sclera?
What should the healthcare provider do when inspecting the conjunctiva and sclera?
What is the normal result of the corneal light reflex test?
What is the normal result of the corneal light reflex test?
What is being assessed during the pupillary light reflex test?
What is being assessed during the pupillary light reflex test?
What is the purpose of shining a pen light onto the eye from the side during the pupillary light reflex test?
What is the purpose of shining a pen light onto the eye from the side during the pupillary light reflex test?
What is the normal response of the pupils when a patient focuses on a finger moving closer to their face?
What is the normal response of the pupils when a patient focuses on a finger moving closer to their face?
Which cranial nerve innervates the superior oblique muscles?
Which cranial nerve innervates the superior oblique muscles?
What is the purpose of the corneal light reflex test?
What is the purpose of the corneal light reflex test?
What is the normal response of the eyes when following a finger through the six cardinal positions of gaze?
What is the normal response of the eyes when following a finger through the six cardinal positions of gaze?
What is the term for the fine oscillating movement of the eyes?
What is the term for the fine oscillating movement of the eyes?
What is the purpose of testing the near reaction?
What is the purpose of testing the near reaction?
What happens to the pupils when a patient is focusing on a distant object?
What happens to the pupils when a patient is focusing on a distant object?
What is the result of a right optic tract cut?
What is the result of a right optic tract cut?
What is the characteristic of the optic disc in a normal eye?
What is the characteristic of the optic disc in a normal eye?
What is the location of the macula in relation to the optic disc?
What is the location of the macula in relation to the optic disc?
What is the normal color of the retinal background?
What is the normal color of the retinal background?
What is the part of the ophthalmoscope that is used to view the retinal vessels?
What is the part of the ophthalmoscope that is used to view the retinal vessels?
What is the result of an optic chiasm cut?
What is the result of an optic chiasm cut?
What is the purpose of the ophthalmoscope?
What is the purpose of the ophthalmoscope?
What is the characteristic of the retinal vessels in a normal eye?
What is the characteristic of the retinal vessels in a normal eye?
What is the leading cause of vision loss and blindness among older adults?
What is the leading cause of vision loss and blindness among older adults?
What is the characteristic symptom of Chronic-open Angle Glaucoma?
What is the characteristic symptom of Chronic-open Angle Glaucoma?
What is the characteristic symptom of Wet (Neovascular) Age-related Macular Degeneration?
What is the characteristic symptom of Wet (Neovascular) Age-related Macular Degeneration?
What is the cause of Glaucoma?
What is the cause of Glaucoma?
What is the characteristic symptom of Cataracts?
What is the characteristic symptom of Cataracts?
What is a risk factor for Chronic-open Angle Glaucoma?
What is a risk factor for Chronic-open Angle Glaucoma?
What is the characteristic effect of Age-related Macular Degeneration on central vision?
What is the characteristic effect of Age-related Macular Degeneration on central vision?
What is the most common type of Age-related Macular Degeneration?
What is the most common type of Age-related Macular Degeneration?
Flashcards are hidden until you start studying
Study Notes
Inspecting the Ear
- Inspect the ear canal, noting any discharge, foreign bodies, redness of the skin, swelling, or cerumen.
- Inspect the tympanic membrane, noting its color, contour, and the presence of a cone of light.
- Look for perforations in the tympanic membrane.
Normal Tympanic Membrane
- The normal tympanic membrane is pale, gray, ovoid, and semi-transparent.
- It is flat, slightly pulled at the center, and flutters if the patient performs the Valsalva maneuver.
- A light reflex (cone of light) is present at 5:00 in the right ear and 7:00 in the left ear.
- Sections of the malleus may be visible.
Testing Auditory Acuity (Gross Hearing)
- Conversational voice test
- Finger Rub Test
- Whisper Test
- If abnormal, perform Weber and Rinne tests.
Weber Test
- Testing for lateralization: briskly stroke the prongs or strike the fork to start vibrations and place it on top of the patient's head.
- Ask the patient if the sound is louder in one ear.
- Normally, the sound is heard midline (equally).
Rinne Test
- Testing air conduction: compare air conduction (AC) to bone conduction (BC).
- Normal result: AC > BC (positive Rinne).
Normal Hearing
- Weber test: no lateralization
- Rinne test: AC > BC (positive Rinne)
Conductive Loss
- Weber test: lateralization to the bad ear
- Rinne test: AC = BC or AC < BC (negative Rinne)
Sensorineural Loss
- Weber test: lateralization to the good ear
- Rinne test: AC > BC (positive Rinne), but overall reduced.
Abnormal - Cerumen
- Impacted cerumen causes partial deafness (conductive hearing loss), tinnitus, or dizziness.
Abnormal - Exostosis
- Discreet, hard, round or oval outcropping formation of new bone on the surface of a bone.
- Seen in swimmers and surfers, develops over many years, and can result in infections, pain, or plugging.
Abnormal - Otitis Externa
- Scaling or crusting, inflammation, and discharge in the canal.
- Pain on movement of the tragus.
- May have palpable lymph nodes.
Abnormal - Foreign Body
- Presence of a foreign body in the ear canal.
Abnormal - Serous Otitis Media
- TM is retracted and has decreased mobility.
- Thin serous effusion gives a yellowish appearance.
- Bubbles apparent if the Eustachian tube is blocked.
Abnormal - Bacterial Otitis Media
- Infection of the middle ear.
Abnormal - Perforated TM
- Presence of a hole in the tympanic membrane.
Abnormal - Scarred TM
- Presence of scarring on the tympanic membrane.
Tympanostomy Tube
- A small tube inserted into the tympanic membrane to drain fluid.
Developmental Considerations
- Infants and children: inner ear starts to develop early in the 4th week of gestation, Eustachian tube is shorter and wider, and the slope of the auditory canal is shorter.
- Older adults: cilia lining the ear canal become coarse and stiff, leading to decreased hearing and cerumen accumulation.
Subjective - History
- Ask about past medical history, including hearing loss, tube placement, and surgery to the ear.
- Ask about family history of hearing loss.
Review of Systems
- Ask the patient about new hearing loss, pain in the ear, discharge, tinnitus, dizziness, nausea, vomiting, exposure to noise, trauma, and self-care behaviors.
Objective - Physical Assessment
- Inspect and palpate the external ear, looking for symmetry, deformities, lumps, pits, and skin lesions.
- Move and palpate the auricle, tragus, and mastoid, assessing for tenderness or pain.
Age-Related Macular Degeneration
- Central vision loss due to degeneration of the macula
- Leading cause of vision loss and blindness among older adults
- Two types: Dry (Atrophic) and Wet (Neovascular)
- Dry type:
- Develops gradually over time
- Early symptom: blurred vision
- Blind spot in central vision, starts small and grows larger over time
- Wet type:
- Develops more rapidly
- Early symptom: straight lines appear wavy
- Blind spot may be visible in central vision
Glaucoma
- Abnormal increase in intraocular pressure (IOP) caused by blockage preventing outflow of vitreous humor
- Two types: Chronic-open angle and Acute Closed Angle
- Chronic-open angle:
- Slow increase in IOP
- Genetic risk factors: family history, diabetes, hypertension, severe myopia, older adults
- Symptoms: halo effect, reduced night vision, report of eye "aching"
- Acute Closed Angle:
- Rapid increase in IOP due to sudden blockage
- Medical emergency - immediate treatment is needed
- Risk factors: eye trauma, eye surgery
- Symptoms: halo effect, photophobia, eye pain, lack of pupil constriction, decreased visual acuity
Cataracts
- Gradual clouding of the lens
- Can be age-related, genetic, or result of trauma from UV exposure
- Can occur in newborns with maternal rubella infection
- Symptoms:
- Cloudy/blurred vision
- Colors appear faded or yellowed
- Patient may report glares and difficulty with night time driving
- May also report halo effect
Documenting Your Findings
- ROS (Review of Systems): ask about recent changes in vision, use of contacts/glasses, eye pain, etc.
- Physical Exam: assess visual acuity, inspect lids and lashes, conjunctiva, sclera, iris, cornea, etc.
- PMH (Past Medical History): ask about history of ocular problems, glaucoma, cataracts, eye trauma, etc.
Developmental Considerations - Older Adults
- Skin loses elasticity, causing drooping, fat tissues, and muscles atrophy
- Cornea may show arcus senilis (degenerative lipid material around the limbus)
- Pupils decrease in size, lens loses elasticity, and cannot change shape to accommodate near vision (presbyopia)
- Lens discolors and thickens (cataract)
- Floaters may appear from debris in vitreous humor
Normal Age-Related Changes - Drusen
- Yellow deposits (made up of lipids and proteins) under the retina
- Normal in aging adults, does not affect vision
- Seen in normal aging or age-related macular degeneration
Identifying Retinal Vessels
- 4 sets of retinal vessels: paired vein and artery in each quadrant
- Arteries appear bright red, may also note a thin strip of white down the center of the arteries
- A:V Ratio = 2:3
- Vessels get smaller the further away they are from the optic disc
Abnormal Findings
- Arteriovenous Nicking (AV nicking): small artery crossing a small vein, resulting in compression of the vein with bulging on either side
- Papilledema: a serious medical condition where the optic nerve at the back of the eye becomes swollen due to a buildup of pressure in or around the brain
- Strabismus: a weakness or paralysis of one or more of the extraocular muscles, due to a congenital defect, an orbital fracture, trauma, or CVA-related palsy
- Retinal Hemorrhages: bleeding in the retina, can be superficial, preretinal, or deep, seen in sudden increases in intracranial pressure, severe hypertension, and diabetes
Eye Exam
- Inspect the eyes for opacities and abrasions using oblique lighting
- Check the size, shape, and symmetry of both pupils, which should be 3-5mm in size
- Miosis refers to abnormal constriction of the pupils, while mydriasis refers to abnormal dilation
- Anisocoria refers to unequal pupils
Corneal Light Reflex
- Shine a light towards the eyes to check for corneal light reflex
- The light should hit both eyes in the same spot, slightly nasal to the center of the pupils
- If the reflex is abnormal, it may indicate a problem with the extraocular muscles (EOMs)
Pupillary Light Reflex
- Test for direct and consensual pupillary light reflex
- Shine a pen light onto the eye from the side while the patient gazes into the distance
- Direct reaction: the pupil exposed to bright light should constrict
- Consensual reaction: the opposite pupil should also constrict
Accommodation
- Test for near reaction: convergence and accommodation
- Hold a finger in front of the patient's nose and have them focus on it
- Pupils should normally dilate when focusing on a far object and constrict when focusing on a near object
Extraocular Muscles
- Test the extraocular muscles by having the patient follow a finger through the six cardinal positions of gaze
- Check for parallel tracking of the eyes and look for nystagmus (fine oscillating movement) or lid lag
Visual Fields
- Assess the range of peripheral visual fields
- Check for any defects or abnormalities in the visual fields
Visual Pathways
- Review the visual pathways, including the optic nerve, optic chiasm, and optic tract
- Visual fields are projected upside down and reversed right to left
- Nerve impulses are conducted through the retina, optic nerve, optic chiasm, and optic tract on each side
Subjective History
- Ask about the patient's medical history, including any ocular problems, strabismus, glaucoma, cataracts, or eye trauma
- Ask about medications, including eye drops, and any prior surgeries involving the eyes
- Ask about family history of genetic eye conditions
Physical Exam
- Assess visual acuity using the Snellen test
- Inspect the lids, lashes, conjunctiva, sclera, iris, and cornea
- Check the shape and size of the pupils
- Test the corneal light reflex, pupillary light reflex, and accommodation
- Assess the extraocular muscles and visual fields
- Perform a funduscopic examination
Abnormalities
- Myopia (nearsightedness) and hyperopia (farsightedness) can cause impaired vision
- Glaucoma can cause abnormal increase in intraocular pressure (IOP) and lead to vision loss
- Cataracts can cause gradual clouding of the lens and lead to vision loss
- Age-related macular degeneration (ARMD) can cause central vision loss due to degeneration of the macula
- Optic nerve or optic tract cuts can cause visual field defects
Documentation
- Document the findings of the eye exam, including any abnormalities or defects
- Use a clear and concise format to record the results of the exam
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.