Podcast
Questions and Answers
A post-menopausal woman's DEXA scan reveals a T-score of -2.0. How should this result be interpreted?
A post-menopausal woman's DEXA scan reveals a T-score of -2.0. How should this result be interpreted?
- Paget's disease is indicated.
- Osteopenia is indicated. (correct)
- Osteoporosis is indicated.
- Normal bone density.
Which medication is most commonly used to treat osteoporosis by increasing bone density through calcium deposition?
Which medication is most commonly used to treat osteoporosis by increasing bone density through calcium deposition?
- Methotrexate
- Bisphosphates (correct)
- Colchicine
- Allopurinol
What is the primary difference between rickets and osteomalacia?
What is the primary difference between rickets and osteomalacia?
- Rickets affects children, while osteomalacia affects adults. (correct)
- Rickets is caused by calcium deficiency, while osteomalacia is caused by vitamin D deficiency.
- Rickets affects adults, while osteomalacia affects children.
- Rickets is treated with bisphosphates, while osteomalacia is treated with antibiotics.
A 65-year-old male presents with bone pain, frequent headaches, and tingling sensations in his arms and legs. An X-ray reveals bone deformities. Which condition is most likely?
A 65-year-old male presents with bone pain, frequent headaches, and tingling sensations in his arms and legs. An X-ray reveals bone deformities. Which condition is most likely?
Which of the following is the most common cause of osteomyelitis?
Which of the following is the most common cause of osteomyelitis?
A patient complains of joint pain that worsens throughout the day, primarily in the knees and hips. X-rays show thinning cartilage and osteophytes. Which condition is most likely?
A patient complains of joint pain that worsens throughout the day, primarily in the knees and hips. X-rays show thinning cartilage and osteophytes. Which condition is most likely?
Which of the following characteristics is more commonly associated with rheumatoid arthritis (RA) compared to osteoarthritis (OA)?
Which of the following characteristics is more commonly associated with rheumatoid arthritis (RA) compared to osteoarthritis (OA)?
A patient with rheumatoid arthritis is prescribed Methotrexate. What is the purpose of this medication?
A patient with rheumatoid arthritis is prescribed Methotrexate. What is the purpose of this medication?
Which joint is primarily affected in early stages of rheumatoid arthritis, often leading to ulnar deviation?
Which joint is primarily affected in early stages of rheumatoid arthritis, often leading to ulnar deviation?
A patient with osteoarthritis experiences stiffness in the morning that improves as the day progresses. Is this statement True or False?
A patient with osteoarthritis experiences stiffness in the morning that improves as the day progresses. Is this statement True or False?
What is the underlying cause of inflammation in gout?
What is the underlying cause of inflammation in gout?
Which dietary change is typically recommended for patients to manage and prevent gout attacks?
Which dietary change is typically recommended for patients to manage and prevent gout attacks?
What is a common subjective sign of gout?
What is a common subjective sign of gout?
Which of the following conditions is characterized by widespread muscle pain and tenderness, along with fatigue and sleep problems, and is more common in women?
Which of the following conditions is characterized by widespread muscle pain and tenderness, along with fatigue and sleep problems, and is more common in women?
When diagnosing fibromyalgia, what would be expected from blood tests measuring inflammatory markers?
When diagnosing fibromyalgia, what would be expected from blood tests measuring inflammatory markers?
A patient is diagnosed with osteomyelitis following a surgical procedure. Which of the following is the most likely course of treatment?
A patient is diagnosed with osteomyelitis following a surgical procedure. Which of the following is the most likely course of treatment?
A patient with gout is experiencing an acute flare-up. Which medication is most appropriate for immediate relief of pain and inflammation?
A patient with gout is experiencing an acute flare-up. Which medication is most appropriate for immediate relief of pain and inflammation?
What is the primary goal of treatment for osteoarthritis?
What is the primary goal of treatment for osteoarthritis?
Which pathological condition is indicated by the presence of osteophytes on X-rays?
Which pathological condition is indicated by the presence of osteophytes on X-rays?
Which of the following complications is associated with Paget's disease?
Which of the following complications is associated with Paget's disease?
Flashcards
Osteopenia
Osteopenia
Lower bone density than normal for age, showing decreased bone mass and increased porosity.
Osteoporosis
Osteoporosis
Severe weakening of bones, more susceptible to fractures; often linked to hormones or deficiencies.
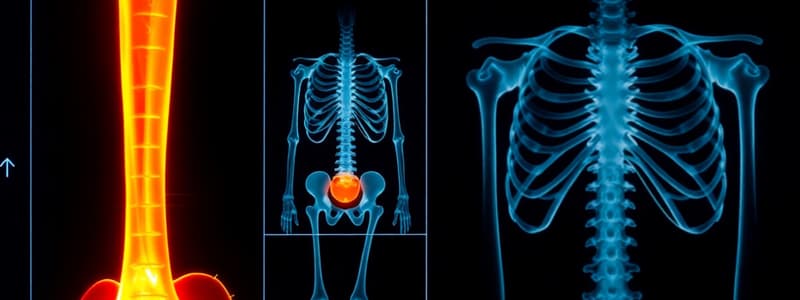
DEXA Scan
DEXA Scan
X-ray to measure bone density; T-score indicates bone condition.
Bisphosphonates
Bisphosphonates
Signup and view all the flashcards
Rickets
Rickets
Signup and view all the flashcards
Osteomalacia
Osteomalacia
Signup and view all the flashcards
Paget's Disease
Paget's Disease
Signup and view all the flashcards
Osteomyelitis
Osteomyelitis
Signup and view all the flashcards
Osteoarthritis (OA)
Osteoarthritis (OA)
Signup and view all the flashcards
Rheumatoid Arthritis (RA)
Rheumatoid Arthritis (RA)
Signup and view all the flashcards
DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
Signup and view all the flashcards
Osteophytes
Osteophytes
Signup and view all the flashcards
Gout
Gout
Signup and view all the flashcards
Fibromyalgia
Fibromyalgia
Signup and view all the flashcards
Study Notes
Osteoporosis vs. Osteopenia
- Osteopenia is a condition characterized by lower bone density than normal for a person's age, indicating a decrease in bone mass and increased porosity.
- Osteoporosis is a more severe condition than osteopenia, leading to weakened bones that are more susceptible to fractures.
- Osteoporosis is often associated with hormonal changes, especially in post-menopausal women, as well as calcium or vitamin D deficiencies.
- Bone mineral density is measured using a DEXA scan, which is an X-ray that quantifies bone density.
- A T-score from a DEXA scan indicates bone density, where scores greater than -1 are considered normal.
- T-scores between -1 and -2.5 indicate osteopenia
- T- scores of -2.5 or lower indicate osteoporosis
Clinical Manifestations and Treatment of Osteoporosis
- Clinical signs of osteoporosis include decreased height, fractures (especially compression fractures), and kyphosis.
- Bisphosphates are a class of medications used to treat osteoporosis by drawing calcium from the blood and depositing it back into the bones, increasing bone density.
Rickets and Osteomalacia
- Rickets is the softening and weakening of bones in children, while osteomalacia is the same condition occurring in adults.
- These conditions are typically caused by deficiencies in vitamin D, calcium, or phosphate.
- While rare in the U.S., rickets remains a significant health issue in underdeveloped countries.
- Rickets can be prevented through vitamin D supplementation and a diet rich in vitamin D.
- Softened bones from rickets or osteomalacia are prone to bowing and fractures.
- Diagnosis involves blood tests to check calcium and phosphorus levels, X-rays, and bone biopsies.
- Treatment primarily involves supplementation to address the underlying deficiency.
Paget's Disease
- Paget's disease is a progressive condition characterized by abnormal bone destruction and remodeling, leading to bone deformities.
- The cause of Paget's disease is unknown, and while there is no cure, treatment can help manage the condition.
- Paget's disease is more common in individuals over 40, with incidence rates doubling each decade.
- It is also more prevalent in men than in women.
- Clinical signs can include bone pain, headaches, tingling, numbness in the arms and legs, and bent bones.
- Complications can include fractures, deformities, osteoarthritis, and bone cancer.
- Diagnosis involves blood tests, X-rays, and bone scans.
- Treatment includes bisphosphates, similar to osteoporosis treatment.
Osteomyelitis
- Osteomyelitis is an infectious bone disease characterized by inflammation or swelling in the bone.
- Bacteria entering from outside the body, such as through a wound, open fracture, or surgical procedure, typically causes it.
- Osteomyelitis is more common in young children (under 5) and older adults.
- Clinical signs include bone pain and inflammation.
- Treatment commonly involves surgical debridement, culture, and antibiotics.
- MRSA (methicillin-resistant Staphylococcus aureus) is a common causative bacterium.
Osteoarthritis (OA) vs. Rheumatoid Arthritis (RA)
- Osteoarthritis is a degenerative and progressive joint disorder resulting from the destruction of normal collagen due to wear and tear.
- Rheumatoid arthritis is a chronic autoimmune inflammatory disorder affecting many joints, including those in the hands and feet.
- OA affects 30 million people in the U.S., with incidence increasing with age and obesity, and is common in individuals 40 and older.
- RA affects about 6 million people in the U.S., with 75% of cases occurring in women.
- The cause of RA is multifactorial and often autoimmune.
- OA affects joints asymmetrically, particularly large weight-bearing joints like the knees and hips, with pain increasing throughout the day.
- RA affects joints symmetrically, with pain often improving as the day goes on.
- Diagnosis of OA involves plain X-rays and joint fluid analysis, with no specific lab work.
- Diagnosis of RA involves physical exams, blood work (inflammatory markers and rheumatoid factor), and imaging. Lifestyle modifications are key to its management, as well as anti-inflammatory medicines, physical therapy and supportive devices
Clinical Features: OA vs. RA
- OA treatment focuses on symptom relief, maintaining function, limiting disability, and avoiding drug toxicity, including lifestyle changes such as weight loss and exercise.
- RA management involves NSAIDs for pain and inflammation, as well as disease-modifying anti-rheumatic drugs (DMARDs) like Methotrexate and TNF inhibitors like Enbrel and Humira.
- In OA, there is thinning cartilage and osteophytes (bone spurs), which are not common in RA.
- RA involves bone erosion and swollen, inflamed synovial membranes, with swelling, redness, and heat in the synovial membrane.
- On X-rays, osteophytes indicate degeneration associated with osteoarthritis.
More Clinical Feature Details
- Rheumatoid arthritis primarily affects metacarpophalangeal and proximal interphalangeal joints, often leading to ulnar deviation.
- Osteoarthritis primarily affects distal interphalangeal and carpometacarpal joints.
- Heberden's nodes and Bouchard's nodes (nodes on the finger joints) are absent in RA but frequently present in OA
- RA joints are soft, warm, and tender to the touch due to inflammation, while OA joints are hard and bony.
- Stiffness worsens after rest in RA, improving as the day progresses, while stiffness in OA worsens after effort, often described as evening stiffness.
Gout
- Gout is an inflammatory disorder caused by elevated levels of uric acid in the blood and body fluids, including synovial fluid.
- Uric acid crystals form in the joints, causing inflammation.
- A defect in purine metabolism can cause gout.
- Subjective signs as pain, swelling, redness, heat, stiff joints, and night pain
- Gout attacks abruptly happen in a peripheral joint, 50% occuring in the great toe joints.
- Kidney stones are much more common in patients with gout compared to the general population.
- Diagnosis involves history, blood work, and joint fluid samples.
- Management includes medications like colchicine, corticosteroids, NSAIDs, and allopurinol.
- Patients should avoid foods high in purines, such as shellfish, alcohol (especially beer), and organ meats, to prevent gout attacks.
Fibromyalgia
- Fibromyalgia is a chronic musculoskeletal syndrome characterized by widespread muscle pain and tenderness, as well as joint tenderness.
- It is extremely common, with 90% of those affected being women, and is typically diagnosed between the ages of 30 and 50.
- The pathophysiology is unclear, but it is common in people, particularly women, who may also have irritable bowel syndrome or chronic fatigue.
- Clinical signs include chronic muscle pain, fatigue, sleep problems, and painful tender points.
- Diagnosing Fibromyalgia involves a history and physical, as there are no positive inflammatory markers (normal CRP and sed rate).
- Treatment includes medications for comfort, physical therapy, water therapy, and rest.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.