Podcast
Questions and Answers
Which age group has the highest prevalence of fractures related to osteoporosis?
Which age group has the highest prevalence of fractures related to osteoporosis?
- Adults aged 30 and above
- Children under 18
- Women aged 50 and above (correct)
- Men aged 60 and below
What is the primary mechanism by which low Vitamin D levels lead to increased bone resorption?
What is the primary mechanism by which low Vitamin D levels lead to increased bone resorption?
- Increased availability of calcium in the blood
- Enhanced bone mineralization
- Elevated levels of parathyroid hormone (PTH) (correct)
- Inhibition of osteoclast activity
Which type of fracture is commonly associated with osteoporosis and is often the result of reduced bone density?
Which type of fracture is commonly associated with osteoporosis and is often the result of reduced bone density?
- Greenstick fracture
- Stress fracture
- Colles' fracture (correct)
- Compound fracture
What is the main diagnostic method used to measure bone mineral density in osteoporosis patients?
What is the main diagnostic method used to measure bone mineral density in osteoporosis patients?
Which region has the highest prevalence of knee osteoarthritis?
Which region has the highest prevalence of knee osteoarthritis?
What change occurs in the bone marrow related to increased plasma cells in osteoporosis?
What change occurs in the bone marrow related to increased plasma cells in osteoporosis?
What is the expected increase in the burden of osteoporosis-related fractures by 2050 worldwide?
What is the expected increase in the burden of osteoporosis-related fractures by 2050 worldwide?
What is the primary mechanism by which bisphosphonates help treat Paget's disease?
What is the primary mechanism by which bisphosphonates help treat Paget's disease?
What is the primary pathological change observed in osteoarthritis?
What is the primary pathological change observed in osteoarthritis?
Which treatment option is considered the first-line for rapid normalization of alkaline phosphatase in Paget's disease?
Which treatment option is considered the first-line for rapid normalization of alkaline phosphatase in Paget's disease?
What effect does estrogen have on bone mineralization in women?
What effect does estrogen have on bone mineralization in women?
Which component of the cartilage matrix is primarily degraded in osteoarthritis?
Which component of the cartilage matrix is primarily degraded in osteoarthritis?
What type of imaging is typically performed to assess the severity of osteoarthritis?
What type of imaging is typically performed to assess the severity of osteoarthritis?
Which of the following skeletal sites is least likely to be affected by osteoporosis-related fractures?
Which of the following skeletal sites is least likely to be affected by osteoporosis-related fractures?
In the context of Paget's disease, what is the significance of microfractures?
In the context of Paget's disease, what is the significance of microfractures?
What characteristic is NOT typically associated with osteoarthritic joint tissues?
What characteristic is NOT typically associated with osteoarthritic joint tissues?
What differentiates Paget's disease from rheumatoid arthritis?
What differentiates Paget's disease from rheumatoid arthritis?
Which characteristic is indicative of osteomalacia or rickets seen in radiographic images?
Which characteristic is indicative of osteomalacia or rickets seen in radiographic images?
What histological feature is observed in bone biopsies of patients with osteomalacia?
What histological feature is observed in bone biopsies of patients with osteomalacia?
What feature seen on X-ray is indicative of osteoarthritis?
What feature seen on X-ray is indicative of osteoarthritis?
What does the typical female-to-male ratio of rheumatoid arthritis suggest?
What does the typical female-to-male ratio of rheumatoid arthritis suggest?
Which of the following reflects a false statement about abnormal chondrocyte behavior in osteoarthritis?
Which of the following reflects a false statement about abnormal chondrocyte behavior in osteoarthritis?
What is the most common clinical presentation of Paget’s disease?
What is the most common clinical presentation of Paget’s disease?
Which of the following is NOT a common symptom of osteoarthritis?
Which of the following is NOT a common symptom of osteoarthritis?
Which skeletal sites are most commonly affected by Paget’s disease?
Which skeletal sites are most commonly affected by Paget’s disease?
What biochemical marker is typically increased in patients with Paget’s disease?
What biochemical marker is typically increased in patients with Paget’s disease?
Which of the following features is less commonly associated with Paget’s disease?
Which of the following features is less commonly associated with Paget’s disease?
Which population is most commonly affected by Paget's disease?
Which population is most commonly affected by Paget's disease?
Which symptom is not typically associated with Paget’s disease?
Which symptom is not typically associated with Paget’s disease?
What primarily causes the accelerated phase of bone loss in women after menopause?
What primarily causes the accelerated phase of bone loss in women after menopause?
What is the fundamental defect in both osteomalacia and rickets?
What is the fundamental defect in both osteomalacia and rickets?
Which vitamins or supplements are recommended for those with osteoporosis who have deficiencies?
Which vitamins or supplements are recommended for those with osteoporosis who have deficiencies?
Which bone disorder occurs in children with open growth plates?
Which bone disorder occurs in children with open growth plates?
What might cause ineffective vitamin D activation in the body?
What might cause ineffective vitamin D activation in the body?
What is a characteristic feature of osteomalacia pathology?
What is a characteristic feature of osteomalacia pathology?
What could be a potential consequence of excessive treatment in osteomalacia and rickets?
What could be a potential consequence of excessive treatment in osteomalacia and rickets?
Which of the following describes a hallmark physical feature of rickets?
Which of the following describes a hallmark physical feature of rickets?
What type of joint fluid is typically found in a joint affected by osteoarthritis?
What type of joint fluid is typically found in a joint affected by osteoarthritis?
Which feature is characteristic of advanced osteoarthritis seen on X-ray?
Which feature is characteristic of advanced osteoarthritis seen on X-ray?
Which condition is NOT considered a part of spondyloarthropathies?
Which condition is NOT considered a part of spondyloarthropathies?
What is a hallmark lesion of spondyloarthritis?
What is a hallmark lesion of spondyloarthritis?
Which of the following describes the radiographic features of reactive arthritis?
Which of the following describes the radiographic features of reactive arthritis?
Which symptom is most likely associated with dactylitis?
Which symptom is most likely associated with dactylitis?
What genetic marker is commonly associated with spondyloarthropathies?
What genetic marker is commonly associated with spondyloarthropathies?
Which condition is characterized by inflammation of a whole finger or toe?
Which condition is characterized by inflammation of a whole finger or toe?
Flashcards
Osteoporosis
Osteoporosis
A common bone disease where bone density decreases, leading to an increased risk of fractures. It's estimated that over 8.9 million fractures occur globally each year due to osteoporosis.
Colles' Fracture
Colles' Fracture
A fracture that occurs in the wrist, specifically the distal radius bone. Often caused by a fall on an outstretched hand.
Vertebral Fractures
Vertebral Fractures
Fractures that occur in the vertebrae of the spine. These can be caused by trauma or due to osteoporosis.
Neck of Femur Fracture
Neck of Femur Fracture
Signup and view all the flashcards
Dual-Energy X-ray Absorptiometry (DXA)
Dual-Energy X-ray Absorptiometry (DXA)
Signup and view all the flashcards
T Score
T Score
Signup and view all the flashcards
Hyperparathyroidism
Hyperparathyroidism
Signup and view all the flashcards
Bone Resorption
Bone Resorption
Signup and view all the flashcards
Age-Related Bone Loss
Age-Related Bone Loss
Signup and view all the flashcards
Bone Remodeling Cycle
Bone Remodeling Cycle
Signup and view all the flashcards
Osteoclasts
Osteoclasts
Signup and view all the flashcards
Osteoblasts
Osteoblasts
Signup and view all the flashcards
Osteomalacia and Rickets
Osteomalacia and Rickets
Signup and view all the flashcards
Mineralization Disorder
Mineralization Disorder
Signup and view all the flashcards
Vitamin D Deficiency
Vitamin D Deficiency
Signup and view all the flashcards
Paget's Disease
Paget's Disease
Signup and view all the flashcards
Microfractures
Microfractures
Signup and view all the flashcards
Bisphosphonate
Bisphosphonate
Signup and view all the flashcards
Rheumatoid Arthritis
Rheumatoid Arthritis
Signup and view all the flashcards
What is Rheumatoid Arthritis?
What is Rheumatoid Arthritis?
Signup and view all the flashcards
Looser's Zones
Looser's Zones
Signup and view all the flashcards
Osteomalacia
Osteomalacia
Signup and view all the flashcards
Thick Osteoid Seams
Thick Osteoid Seams
Signup and view all the flashcards
Increased Bone Turnover
Increased Bone Turnover
Signup and view all the flashcards
Sclerotic Lesions
Sclerotic Lesions
Signup and view all the flashcards
Alkaline Phosphatase
Alkaline Phosphatase
Signup and view all the flashcards
Bone Pain
Bone Pain
Signup and view all the flashcards
What is Enthesitis?
What is Enthesitis?
Signup and view all the flashcards
What are Spondyloarthropathies?
What are Spondyloarthropathies?
Signup and view all the flashcards
What is Dactylitis?
What is Dactylitis?
Signup and view all the flashcards
What causes a Varus Knee Deformity?
What causes a Varus Knee Deformity?
Signup and view all the flashcards
What is Axial Spondyloarthritis?
What is Axial Spondyloarthritis?
Signup and view all the flashcards
What is Ankylosing Spondylitis?
What is Ankylosing Spondylitis?
Signup and view all the flashcards
What is the characteristic of Synovial Fluid in Osteoarthritis?
What is the characteristic of Synovial Fluid in Osteoarthritis?
Signup and view all the flashcards
How does Osteoarthritis present in Biochemistry?
How does Osteoarthritis present in Biochemistry?
Signup and view all the flashcards
What is osteoarthritis?
What is osteoarthritis?
Signup and view all the flashcards
What is a key factor in the development of osteoarthritis?
What is a key factor in the development of osteoarthritis?
Signup and view all the flashcards
How does OA affect cartilage cells?
How does OA affect cartilage cells?
Signup and view all the flashcards
Why are X-rays important for diagnosing OA?
Why are X-rays important for diagnosing OA?
Signup and view all the flashcards
What are osteophytes?
What are osteophytes?
Signup and view all the flashcards
What is subchondral sclerosis?
What is subchondral sclerosis?
Signup and view all the flashcards
What are subchondral cysts?
What are subchondral cysts?
Signup and view all the flashcards
How does the prevalence of OA differ across ethnicities?
How does the prevalence of OA differ across ethnicities?
Signup and view all the flashcards
Study Notes
Approach to the Patient with Metabolic Bone Disease & Rheumatic Disease
- This presentation outlines an approach to patients with metabolic bone disease and rheumatic disease.
- A roadmap is presented, highlighting key areas like general approach, osteomalacia/rickets, osteoporosis, rheumatoid arthritis, and spondyloarthropathies.
Clinical Examination of the Musculoskeletal System
- Hands: Swelling, deformity, nail changes, tophi, Raynaud's, rheumatoid nodules, nail dystrophy in psoriatic arthritis.
- Face: Rash, alopecia, mouth ulcers, butterfly rash, scleritis.
- Trunk: Kyphosis, scoliosis, tender spots (fibromyalgia, enthesitis).
- Legs: Deformity, swelling, restricted movement, synovitis, Heberden and Bouchard nodes.
- Feet: Deformity, swelling (gout, dactylitis), redness, acute gout.
- General observation: includes gait, deformity, swelling, redness, and rash are all examined.
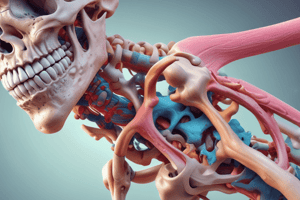
Structure of Major Musculoskeletal Tissues
- Bone: Calcified zone, hypertrophic zone, proliferative zone, trabecular bone, cortical bone, osteoblasts, osteocytes, osteoclasts, epiphyseal plate.
- Muscle: Myofilament, myofibril, fascicle.
- Articular cartilage: Chondrocytes, calcified cartilage, subchondral bone, synovium, synovial lining cells, joint capsule, haversian system, blood vessels, collagen lamellae, osteocytes.
- Calcium phosphate travels through blood and goes into kidney.
Bone Remodelling Cycle
- Bone-lining cells, microdamage, osteoclasts (eat old bone), osteocytes (new bone), osteoblasts (formation of new bone), apoptotic osteoclast, resorption, reparation of the bone, osteoclasts dead in 12 days, reversal.
Example of Double Tetracycline Labelling
- Evaluates the creation of new bone.
- Using a double tetracycline marker, the progress of new growth is measured by the disparity between the markers
Cellular and Molecular Regulators of Bone Remodelling
- Renal phosphate excretion, bone marrow stromal cells, FGF23, SOST, Wnt, osteoblast, osteocyte, OPG, M-CSF, RANKL, osteoclast precursor, osteoclast.
Key Regulators of Bone Remodelling
- Mediator: RANKL, Osteoprotegerin, Wnt, Sclerostin, Parathyroid hormone, Thyroid hormone, Oestrogen, Glucocorticoid.
- Source: Osteocytes, stromal cells, activated T cells, lymphocytes, stromal cells, osteocytes, parathyroid glands, thyroid gland, ovaries, adrenal glands, exogenous.
- Effects: Stimulates bone resorption, inhibits bone resorption, stimulates bone formation, activates LRP receptors, blocks effect of Wnt, increases bone resorption and formation, increases bone resorption and formation, inhibits bone resorption, inhibits bone formation.
Investigations of Musculoskeletal Disease
- Imaging: Plain X-rays, bone scintigraphy, MRI, ultrasonography, computed tomography, dual x-ray absorptiometry
- Blood tests: Haematology, biochemistry, immunology
- Other: Tissue biopsy, electromyography, joint aspiration
MRI & Ultrasound Image Showing Synovitis
- Images showing inflammation of the synovial membrane.
Typical Biochemical Abnormalities in Various Skeletal Diseases
- Charts showing the presence and absence of abnormalities in a variety of bone disorders.
Patterns of Joint Involvement in Different Forms of Polyarthritis
- Diagrams showing the areas of the skeleton affected in various forms of arthritis.
Osteoporosis
- Most common bone disease, more than 8.9 million fractures annually.
- One-third of women and one-fifth of men age 50 and above.
- Fracture risks increase over time.
- Common fracture sites include the forearm, spine, humerus, and hip.
Dual-Energy X-ray Absorptiometry (DXA)
- Measures bone density.
- Scores show bone density as T and Z scores.
Risk Factors for Osteoporosis
- Genetic factors: single-gene disorders, receptor mutations, endocrine disease.
- Inflammatory disease: inflammatory bowel disease, ankylosing spondylitis.
- Drugs: glucocorticoids, gonadotrophin releasing hormone agonists, levothyroxine.
- Gastrointestinal disease: malabsorption.
- Lung disease: chronic obstructive pulmonary disease.
- Myeloma, homocystinuria, anorexia nervosa, highly trained athletes, HIV, Gaucher's disease, polygenic inheritance, hyperparathyroidism, Cushing's syndrome.
- Rheumatoid arthritis, aromatise inhibitors, thiazolidinediones, anticonvulsants, alcohol intake, heparin, chronic liver disease, cystic fibrosis, systemic mastocytosis, immobilisation, body mass index <18, smoking.
- Data on Vit D intake and calcium ingestion affect bone reabsorption.
- Osteoporosis occurs due to an imbalance between bone reabsorption osteoblast, and creation of new bone osteoclast.
Fractures
- Tables and diagrams showing fracture rates across different age groups and areas of the body.
Vertebral Fractures
- Data on cumulative survival with and without vertebral fractures.
Pathophysiology of Osteoporosis
- Reduced bone density leads to micro-architectural deterioration and fracture risk, increased risk of falling with age, bone mass increase during growth, fall afterward, bone loss accelerates post-menopause due to estrogen deficiency ,and imbalance in bone remodelling cycle.
Investigations in Osteoporosis
- Lists of investigations to perform to diagnose osteoporosis.
Drug Treatments for Osteoporosis
- Tables comparing various drug treatments' regimens, daily doses, and other factors.
Osteomalacia and Rickets
- OM and rickets are similar; the difference is that rickets occurs in children, OM in adults.
- Disturbed mineralization of osteoid, causing thick osteoid, stress fractures, bow-leggedness, and other skeletal issues.
Causes of Osteomalacia and Rickets
- Deficiency in vitamin D, lack of sunlight exposure, poor diet, malabsorption, familial hyperphosphatemia, kidney damage, and loss-of-function mutations.
- Defects in phosphate and pyrophosphate metabolism, mutations, tumour-induced hypophosphataemic osteomalacia, hypophosphatasia, and high fluoride in water.
Osteomalacia and Rickets (radiographs)
- Radiographic examples illustrating the conditions, particularly pseudofractures and bowing.
Paget's Disease
- Focal areas of increased and disorganized bone remodeling involving one or more skeletal sites.
- Increased bone resorption by abnormal osteoclasts, followed by rapid formation of poorly organized, structurally weak bone.
- Plain radiographs show increased uptake of radionuclide, increased serum levels of alkaline phosphatase, a hallmark sign of the disease.
Clinical Features of Paget's disease
- Axial skeleton is predominantly affected.
- Bone pain and pathological fracture.
- Many patients are asymptomatic.
- Bone deformity and expansion, increased warmth over affected bone.
- Neurological problems: deafness, cranial nerve defects, nerve root pain, spinal cord compression, and spinal stenosis.
- Osteosarcoma, a rare and serious complication.
Paget's disease (radiographs)
- Radiographic image highlighting the intense tracer uptake and deformity of the affected femur, and areas of osteosclerosis and radiolucency with pseudofractures.
Treatment for Paget's disease
- Combination of nonpharmacological (physical therapy) and pharmacological therapy (antiresorptive agents, analgesics).
- Bisphosphonates inhibit osteoclast activity.
- IV zoledronic acid leads to rapid, sustained normalization of alkaline phosphatase.
- Surgery may be needed for impending or complete fractures, joint realignment, and total arthroplasty in severe cases.
Rheumatoid Arthritis
- Common inflammatory arthritis affecting all ethnic groups worldwide.
- Prevalence: 0.8-1.0% in Europe and the Indian subcontinent (lower in Asia).
- Chronic disease with exacerbations and remissions.
Pathophysiology of Rheumatoid Arthritis
- Environmental triggers, genetic predisposition, and immune response lead to inflammation, immune complexes, activation and proliferation of T cells, macrophages and B cells.
- Leading to synovial inflammation, bone erosion, and cartilage destruction.
Criteria for Diagnosis of Rheumatoid Arthritis
- Scoring system based on joint involvement, presence of rheumatoid factors/anti-CCP antibodies, symptoms duration and acute phase reactants.
Clinical Presentation of Rheumatoid Arthritis
- Morning stiffness, symmetrical joint swelling affecting hands, wrists (proximal interphalangeal and metacarpophalangeal joints, and metatarsophalangeal joints), bony erosion and cartilage damage.
- Extra-articular features: rheumatoid nodules, interstitial lung disease, vasculitis, pleuropericarditis, scleritis, episcleritis, leg ulcers, Felty syndrome.
Investigations and Monitoring for Rheumatoid Arthritis
- Clinical criteria, erythrocyte sedimentation rate, C-Reactive protein, ultrasound or MRI, and tests for rheumatoid factor and anti-citrullinated peptide antibodies.
- Monitor disease activity, monitor damage with x-rays, and monitor drug safety.
Calculation of the Disease Activity Score and Algorithm for Management (rheumatoid arthritis)
- Measurement to assess the severity of disease activity and adapt treatment strategies accordingly.
- Factors such as number of swollen and tender joints, erythrocyte sedimentation rate, patient self assessment (on a scale of 0 -100), and are used to categorise patients into a specific category of disease activity.
Osteoarthritis
- Most common type of arthritis, characterised by pain and disability in older adults.
- Focal loss of articular cartilage, subchondral osteosclerosis, osteophyte formation, joint margin remodeling, and affected joint enlargement.
- Increased prevalence with age (45% knee OA, 25% hip OA).
Pathophysiology of Osteoarthritis
- Cartilage degeneration is the defining feature.
- Chondrocytes start dividing and producing nests of metabolically active cells.
- Increased degradation of cartilage matrix components (aggrecan and type II collagen).
- Reduced concentration of aggrecan, making cartilage vulnerable to injury.
Pathologic Features of Osteoarthritic Joint Tissues
- Diagrams illustrating normal vs. osteoarthritic joints, including synovial membrane, cartilage, and subchondral bone.
Risk Factors and Pathological Changes in Osteoarthritis
- Genetic factors, adverse biomechanics, meniscectomy, ligament ruptures, Paget's disease, obesity, trauma, hormonal factors (estrogen deficiency) and aromatase inhibitors, can all lead to osteoarthritis.
- Abnormal nests of proliferating chondrocytes, cartilage fibrillation, osteophytes formation, subchondral sclerosis, and subchondral cysts are all hallmarks of osteoarthritis.
Symptoms and Signs of Osteoarthritis
- Insidious onset, variable, intermittent pain related to movement and weight-bearing, relieved by rest, brief morning stiffness.
- Restricted movement, palpable/audible crepitus, bony swelling, deformation, joint line/periarticular tenderness, muscle weakness, and minimal synovitis.
Investigations for Osteoarthritis
- Plain X-ray of the affected joint, which shows osteophytes and joint space narrowing.
- MRI can be performed to look for nerve compression.
- Biochemical, haematological, and rheumatological tests.
- Synovial fluid analysis is usually normal.
X-Ray Appearances in Knee Osteoarthritis
- Radiographic findings showing almost complete loss of joint space, sclerosis of subchondral bone, and lateral displacement of the patella.
Typical Varus Knee Deformity
- Radiographic image illustrating varus deformity of the knee related to osteoarthritis.
Spondyloarthropathies
- Group of related inflammatory musculoskeletal diseases with shared immunogenetic association with HLA-B27.
- Includes axial spondyloarthritis, ankylosing spondylitis, reactive arthritis, psoriatic arthritis, and arthritis associated with inflammatory bowel disease.
Spondyloarthropathies (Clinical Features)
- Axial skeleton is predominantly affected.
- Non-synovial musculoskeletal lesions (inflammatory in nature).
- Hallmarks is enthesitis (inflammation of a ligament or tendon being inserted into a bone).
- Dactylitis is also possible.
Spondyloarthropathies (Pathophysiology)
- Environmental triggers, genetic predisposition, and immune responses lead to an inflammatory process along ligaments, tendons, and periosteum.
- Key components to look at are the gut flora, microbial products, dendritic cell, antigen, T-cell activation and cytokine production (IL-22, TNF-α, IL-17).
Comparison of Spondyloarthropathies
- Table comparing the characteristics of different types of spondyloarthritis, including sacroiliitis involvement, peripheral arthritis, presence of HLA-B27, extra-articular features, and other names for the condition.
Radiographic Changes in Spondyloarthritis
- X-ray images illustrating typical radiographic changes in ankylosing spondylitis (symmetrical marginal syndesmophytes) and psoriatic spondylitis (coarse, asymmetrical, non-marginal syndesmophytes).
- Sacroiliac joint fusion, and generalised osteopenia.
Reactive Arthritis
- Clinical description of reactive arthritis, including skin changes (keratoderma blennorrhagicum), penile lesions (balanitis circinata), and ocular involvement.
Psoriatic Arthropathy
- Clinical description and appearance of dactylitis and distal interphalangeal pattern, along with accompanying nail dystrophy (pitting and onycholysis).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on osteoporosis and osteoarthritis with this comprehensive quiz. Explore key concepts such as fracture prevalence, diagnostic methods, and treatment options. Discover the mechanisms behind bone health and the impact of vitamin D and estrogen.