Podcast
Questions and Answers
What is the primary microorganism responsible for osteomyelitis?
What is the primary microorganism responsible for osteomyelitis?
- Staphylococcus aureus (correct)
- Klebsiella
- Escherichia coli
- Pseudomonas
Which risk factor is NOT associated with an increased incidence of osteomyelitis?
Which risk factor is NOT associated with an increased incidence of osteomyelitis?
- Young athletes (correct)
- Poor nutrition
- Impaired immune system
- Elderly individuals
What characterizes chronic osteomyelitis?
What characterizes chronic osteomyelitis?
- Lasts less than 1 month
- Only affects children
- Persists for longer than 4 weeks (correct)
- Absence of recurrent pain
Which of the following is a common clinical manifestation of osteomyelitis?
Which of the following is a common clinical manifestation of osteomyelitis?
What type of imaging is most likely to show a soft tissue mass associated with osteomyelitis?
What type of imaging is most likely to show a soft tissue mass associated with osteomyelitis?
What is the purpose of immobilizing the affected area in osteomyelitis management?
What is the purpose of immobilizing the affected area in osteomyelitis management?
Which complication may arise from untreated acute osteomyelitis?
Which complication may arise from untreated acute osteomyelitis?
Which of the following laboratory studies can indicate an inflammatory process in osteomyelitis?
Which of the following laboratory studies can indicate an inflammatory process in osteomyelitis?
Which antibiotic is typically initiated for staphylococcal infections in osteomyelitis management?
Which antibiotic is typically initiated for staphylococcal infections in osteomyelitis management?
What is the primary route of infection for osteomyelitis that results from other primary infections?
What is the primary route of infection for osteomyelitis that results from other primary infections?
Flashcards
Osteomyelitis
Osteomyelitis
A pyogenic infection of bone and surrounding tissues, potentially acute or chronic, requiring immediate intervention.
Acute Osteomyelitis
Acute Osteomyelitis
Bone infection lasting less than one month; responds to initial antibiotics.
Chronic Osteomyelitis
Chronic Osteomyelitis
Persistent bone infection lasting more than four weeks, resistant to initial antibiotic treatment.
Staphylococcus aureus
Staphylococcus aureus
Signup and view all the flashcards
Hematogenous route
Hematogenous route
Signup and view all the flashcards
Direct route
Direct route
Signup and view all the flashcards
Risk factors for osteomyelitis
Risk factors for osteomyelitis
Signup and view all the flashcards
Sequestrum
Sequestrum
Signup and view all the flashcards
Septic arthritis
Septic arthritis
Signup and view all the flashcards
Septicemia
Septicemia
Signup and view all the flashcards
Erythrocyte Sedimentation Rate (ESR)
Erythrocyte Sedimentation Rate (ESR)
Signup and view all the flashcards
Study Notes
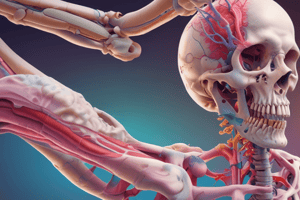
Osteomyelitis Definition and Incidence
- Osteomyelitis is a pyogenic bone infection of surrounding tissues, either acute or chronic, needing immediate intervention.
- It occurs at any age but is more common under 12.
- Males are affected more often than females due to higher rates of blunt trauma.
Etiology and Risk Factors
- Common causes are bacterial infections, primarily Staphylococcus aureus. Other bacteria like Escherichia coli, Pseudomonas, Klebsiella, and Proteus can also be involved.
- Viral and fungal organisms can also initiate osteomyelitis.
- Infection routes include:
- Direct: Open fractures, surgeries, open wounds.
- Hematogenous: Spread from other sites (e.g., upper respiratory infection, tonsillitis, genitourinary tract infections, infected teeth)
- Risk factors include:
- Malnutrition
- Old age
- Obesity
- Weakened immune system
- Chronic diseases (rheumatoid arthritis, diabetes)
- Long-term corticosteroid use
Types of Osteomyelitis
- Acute osteomyelitis: Infection lasting less than one month.
- Chronic osteomyelitis: Infection lasting more than four weeks that doesn't respond to initial antibiotic treatment.
Pathophysiology
- Initial response: Inflammation, increased blood flow, and swelling.
- 2-3 days: Ischemia (reduced blood flow) and bone tissue necrosis (death)
- Infection spreads to the medullary cavity, periosteum, and surrounding soft tissues and joints.
- Chronic osteomyelitis development: If infection isn't effectively treated.
- Abscess formation: Containing dead bone (sequestrum), which is slow to liquefy and drain.
- New bone growth: Develops around the sequestrum, but the infected area persists, leading to recurring abscesses.
Clinical Manifestations
- General symptoms: High fever (38.5-40°C), chills, tachycardia, malaise, headache, nausea.
- Local symptoms (acute): Localized pain (worsening with movement), tenderness, redness, warmth, swelling.
- Local symptoms (chronic): Recurrent pain, redness, warmth, swelling, draining sinus tracts, low-grade fever (up to 38°C).
Complications
- Acute osteomyelitis can progress to chronic form with ineffective treatment.
- Growth retardation in children.
- Septic arthritis and osteoarthritis (infection spreading to adjacent joints).
- Septicemia (infection spreading to the bloodstream).
- Squamous cell carcinoma development (in cases of chronic, draining sinuses).
Diagnostic Studies
- Laboratory tests: Complete blood count (elevated white blood cells), elevated erythrocyte sedimentation rate (ESR). Blood and wound cultures (to identify the causative organism).
- Radiological studies: Bone X-rays (initial soft tissue swelling, bone necrosis), bone scans (detect inflammation), MRI (soft tissue mass, sinus tracts, bone marrow changes).
Management
- General management: Immobilization of the affected area (e.g., casts, slings), pain management, fever control, aseptic wound care.
- Pharmacological management:
- IV antibiotics (e.g., semisynthetic penicillins, cephalosporins, tetracyclines, aminoglycosides) until controlled, then oral for up to 3 months.
- Analgesics (pain relievers) and antipyretics (fever reducers).
- Hyperbaric oxygen therapy (100% O2 at 2 ATM for 2 hours, 6 times/week).
- Surgical management (acute): Needle aspiration, percutaneous biopsy.
- Surgical management (chronic): Surgical debridement to remove dead bone and infected tissue.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.