Podcast
Questions and Answers
Where do melanocytes originate from in relation to oral pigmentation?
Where do melanocytes originate from in relation to oral pigmentation?
- Epidermal cells
- Dermis
- Basal layer of the oral mucosa (correct)
- Connective tissue
What happens to epithelial cells as oral tissue ages?
What happens to epithelial cells as oral tissue ages?
- They divide uncontrollably and become tumors
- They migrate to the surface and form localized pigmented areas (correct)
- They migrate to the surface and retain their color
- They shrink and lose pigmentation
Which medication is known to induce changes in oral pigmentation?
Which medication is known to induce changes in oral pigmentation?
- Ibuprofen
- Paracetamol
- Aspirin
- Tetracycline (correct)
What is an amalgam tattoo in the context of oral pigmentation?
What is an amalgam tattoo in the context of oral pigmentation?
What can be an effect of HIV infection in relation to oral pigmentation?
What can be an effect of HIV infection in relation to oral pigmentation?
Which description best characterizes the clinical appearance of the lining mucosa in a healthy individual?
Which description best characterizes the clinical appearance of the lining mucosa in a healthy individual?
What is a key feature of the lining mucosa that distinguishes it from other types of oral mucosa?
What is a key feature of the lining mucosa that distinguishes it from other types of oral mucosa?
Which areas of the mouth are typically covered by the lining mucosa?
Which areas of the mouth are typically covered by the lining mucosa?
Fordyce spots are characterized by which of the following descriptions?
Fordyce spots are characterized by which of the following descriptions?
What role do sebaceous glands play in the formation of fordyce spots?
What role do sebaceous glands play in the formation of fordyce spots?
Which type of epithelium is most commonly associated with the lining mucosa?
Which type of epithelium is most commonly associated with the lining mucosa?
In terms of histological classification, how many main types of oral mucosa are identified?
In terms of histological classification, how many main types of oral mucosa are identified?
What characteristic does the lining mucosa not possess?
What characteristic does the lining mucosa not possess?
What type of epithelium is primarily found in the area described?
What type of epithelium is primarily found in the area described?
Which feature is characteristic of the submucosa in the described area?
Which feature is characteristic of the submucosa in the described area?
What is one benefit of the connective tissue in this area?
What is one benefit of the connective tissue in this area?
What is the clinical appearance of healthy masticatory mucosa generally?
What is the clinical appearance of healthy masticatory mucosa generally?
Which surgical consideration is noted for areas with the mentioned mucosa?
Which surgical consideration is noted for areas with the mentioned mucosa?
What is a significant characteristic of the masticatory mucosa?
What is a significant characteristic of the masticatory mucosa?
How does infection spread in the masticatory mucosa?
How does infection spread in the masticatory mucosa?
What is a key structural feature of the masticatory mucosa?
What is a key structural feature of the masticatory mucosa?
What type of tissue is primarily involved in aiding the reflexes associated with speech?
What type of tissue is primarily involved in aiding the reflexes associated with speech?
What texture is associated with the healthy appearance of masticatory mucosa?
What texture is associated with the healthy appearance of masticatory mucosa?
What is hyperkeratinization primarily characterized by?
What is hyperkeratinization primarily characterized by?
What type of mucosa is associated with hyperkeratinization in the hard palate?
What type of mucosa is associated with hyperkeratinization in the hard palate?
What is a common cause of hyperkeratinization in the buccal mucosa?
What is a common cause of hyperkeratinization in the buccal mucosa?
Which characteristic identifies a hyperkeratinized area in the oral cavity?
Which characteristic identifies a hyperkeratinized area in the oral cavity?
What is the likely cause of a hyperkeratinized area at the occlusal line in the buccal mucosa?
What is the likely cause of a hyperkeratinized area at the occlusal line in the buccal mucosa?
How is hyperkeratinization describing the appearance of tissue?
How is hyperkeratinization describing the appearance of tissue?
What type of change does keratinized epithelium undergo when exposed to trauma?
What type of change does keratinized epithelium undergo when exposed to trauma?
In which type of mucosa is uneven keratinization commonly found?
In which type of mucosa is uneven keratinization commonly found?
What is a potential reversible change seen in non-keratinized epithelium?
What is a potential reversible change seen in non-keratinized epithelium?
What is a distinguishing histological feature of hyperkeratinized epithelium?
What is a distinguishing histological feature of hyperkeratinized epithelium?
What type of epithelium is most associated with masticatory mucosa?
What type of epithelium is most associated with masticatory mucosa?
Which area is least common in the masticatory mucosa?
Which area is least common in the masticatory mucosa?
What feature makes local anesthetic injections in masticatory mucosa more difficult?
What feature makes local anesthetic injections in masticatory mucosa more difficult?
What is the turnaround time for junctional epithelium?
What is the turnaround time for junctional epithelium?
In which type of mucosa does the nonkeratinized buccal mucosa turn over faster than keratinized gingiva?
In which type of mucosa does the nonkeratinized buccal mucosa turn over faster than keratinized gingiva?
What is a characteristic of epithelial tissue in masticatory mucosa regarding infection?
What is a characteristic of epithelial tissue in masticatory mucosa regarding infection?
What structures are associated with specialized mucosa?
What structures are associated with specialized mucosa?
Which of the following is NOT a feature of masticatory mucosa?
Which of the following is NOT a feature of masticatory mucosa?
Why may surgical procedures in masticatory mucosa require less suture usage?
Why may surgical procedures in masticatory mucosa require less suture usage?
Which characteristic differentiates keratinized from nonkeratinized epithelium?
Which characteristic differentiates keratinized from nonkeratinized epithelium?
Flashcards are hidden until you start studying
Study Notes
Oral Mucosa
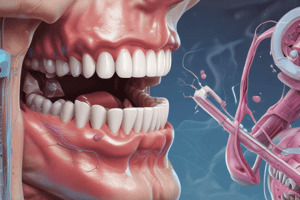
- The oral mucosa is a mucous membrane that lines the inside of the mouth.
- The oral mucosa can be divided into three main types: lining mucosa, masticatory mucosa, and specialized mucosa.
- Lining mucosa covers the inner surfaces of the cheeks, lips, floor of the mouth, ventral surface of the tongue, and soft palate.
- It is non-keratinized stratified squamous epithelium, with a softer surface texture, moist surface, and an ability to stretch and compress.
- Lining mucosa is more prone to infection and requires sutures after surgical incisions due to its ability to stretch and compress.
- Local anesthetic injections are easier in these areas with less discomfort.
- Masticatory mucosa covers the gingiva and hard palate.
- It is keratinized stratified squamous epithelium, with a rubbery surface texture, resiliency (firm base), and a thin submucosa.
- It is more resistant to trauma and less prone to infection due to the firm base.
- Sutures are rarely needed in these areas following surgical procedures.
- Local anesthetic injections are more difficult and cause more discomfort.
- Specialized mucosa covers the dorsal surface of the tongue.
- It includes taste buds and papillae
- It can be either keratinized or non-keratinized, depending on the location.
- Cell turnover times vary between different locations of the oral mucosa.
- The junctional epithelium turn over every 4-6 days.
- The hard palate turns over every 24 days.
- The non-keratinized buccal mucosa turns over faster than keratinized attached gingiva.
- Hyperkeratinization occurs in response to frictional or chemical trauma.
- Non-keratinized epithelium may transform into a keratinizing type.
- Histologically, the tissue will resemble orthokeratinized epithelium with a keratin and granular layer.
- It can be reversible but takes time.
- Oral pigmentation is caused by melanin, a pigment formed by melanocytes that originate from the neural crest.
- Melanocytes reside in the basal layer of the epithelium between dividing epithelial cells.
- They store melanin in cytoplasmic granules and inject it into newly formed epithelial cells.
- As the tissue ages, these pigmented epithelial cells migrate to the surface of the oral mucosa and appear as localized pigmented areas ranging from brown to brownish-black.
Oral Mucosa Variations
- Drug induced color changes can be caused by medication like tetracycline or chemotherapy.
- Infections can lead to changes in appearance, such as Kaposi sarcoma lesions associated with the progression of HIV to AIDS.
- Iatrogenic tattoos are caused by trauma during restoration placement, particularly with amalgam restorations.
- Self-inflicted tattoos are often seen in areas where people bite or chew their lips or cheeks.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.