Podcast
Questions and Answers
What structure primarily forms the diaphragm of the oral cavity floor?
What structure primarily forms the diaphragm of the oral cavity floor?
- Sublingual glands
- Buccinator
- Geniohyoid
- Mylohyoid (correct)
Which muscle is NOT supplied by the hypoglossal nerve?
Which muscle is NOT supplied by the hypoglossal nerve?
- Hyoglossus
- Styloglossus
- Palatoglossus (correct)
- Genioglossus
What is the primary function of the intrinsic muscles of the tongue?
What is the primary function of the intrinsic muscles of the tongue?
- Depress the soft palate
- Elevate the tongue
- Retract the tongue
- Alter the shape of the tongue (correct)
Which nerve provides innervation to the mylohyoid muscle?
Which nerve provides innervation to the mylohyoid muscle?
The fusion of the medial nasal processes forms which structure in the anterior oral cavity?
The fusion of the medial nasal processes forms which structure in the anterior oral cavity?
The terminal sulcus of the tongue separates which two surfaces?
The terminal sulcus of the tongue separates which two surfaces?
What is the primary role of the buccinator muscle in the oral cavity?
What is the primary role of the buccinator muscle in the oral cavity?
Which of the following muscles of the tongue is responsible for depressing the central part of the tongue?
Which of the following muscles of the tongue is responsible for depressing the central part of the tongue?
Which structure is located at the apex of the terminal sulcus?
Which structure is located at the apex of the terminal sulcus?
The oropharyngeal isthmus is defined by which structures?
The oropharyngeal isthmus is defined by which structures?
What is the primary action of the hyoglossus muscle?
What is the primary action of the hyoglossus muscle?
Which of the following describes the location of the geniohyoid muscle?
Which of the following describes the location of the geniohyoid muscle?
Which gland is primarily associated with the submandibular region?
Which gland is primarily associated with the submandibular region?
Which structure extends from the medial to the lateral aspects of the inferior surface of the tongue?
Which structure extends from the medial to the lateral aspects of the inferior surface of the tongue?
Which muscle is responsible for elevating and retracting the tongue?
Which muscle is responsible for elevating and retracting the tongue?
What is the oral fissure bordered by?
What is the oral fissure bordered by?
What is a potential consequence of a parotidectomy?
What is a potential consequence of a parotidectomy?
Which symptom is most commonly associated with mumps?
Which symptom is most commonly associated with mumps?
During surgery of the submandibular gland, which nerve must be carefully preserved to avoid complications?
During surgery of the submandibular gland, which nerve must be carefully preserved to avoid complications?
What systemic symptom may accompany salivary gland swelling in mumps?
What systemic symptom may accompany salivary gland swelling in mumps?
What signals the beginning of facial nerve injury in relation to salivary gland surgery?
What signals the beginning of facial nerve injury in relation to salivary gland surgery?
Which muscle of the soft palate is innervated by the mandibular nerve?
Which muscle of the soft palate is innervated by the mandibular nerve?
What is the primary function of the palatoglossus muscle?
What is the primary function of the palatoglossus muscle?
Which muscle is primarily responsible for pulling the uvula superiorly?
Which muscle is primarily responsible for pulling the uvula superiorly?
What is the role of the tensor veli palatini during yawning or swallowing?
What is the role of the tensor veli palatini during yawning or swallowing?
Which arteries supply the soft palate?
Which arteries supply the soft palate?
Which nerve provides sensory innervation to the hard palate?
Which nerve provides sensory innervation to the hard palate?
What anatomical structure forms the palatoglossal and palatopharyngeal arches?
What anatomical structure forms the palatoglossal and palatopharyngeal arches?
What is the lymphatic drainage pathway for the palate?
What is the lymphatic drainage pathway for the palate?
Which muscle is described as being anterior to the palatopharyngeus?
Which muscle is described as being anterior to the palatopharyngeus?
What is the innervation pathway for the levator veli palatini muscle?
What is the innervation pathway for the levator veli palatini muscle?
Which muscle of the tongue is responsible for depressing the central part and enabling the tongue to protrude?
Which muscle of the tongue is responsible for depressing the central part and enabling the tongue to protrude?
What is the primary action of the styloglossus muscle?
What is the primary action of the styloglossus muscle?
Which artery is responsible for supplying blood to the inferior surface of the tongue?
Which artery is responsible for supplying blood to the inferior surface of the tongue?
Which nerve is responsible for the motor innervation of most of the tongue muscles?
Which nerve is responsible for the motor innervation of most of the tongue muscles?
Which cranial nerve is associated with the special sensation (taste) from the anterior two-thirds of the tongue?
Which cranial nerve is associated with the special sensation (taste) from the anterior two-thirds of the tongue?
What happens if there is an issue with the hypoglossal nerve [XII]?
What happens if there is an issue with the hypoglossal nerve [XII]?
Which muscle is innervated by the vagus nerve [X]?
Which muscle is innervated by the vagus nerve [X]?
What is the primary structure through which the lingual artery enters the oral cavity?
What is the primary structure through which the lingual artery enters the oral cavity?
What separates the nasopharynx from the nasal cavity?
What separates the nasopharynx from the nasal cavity?
Which space serves as a potential path for infections from the pharynx to the posterior mediastinum?
Which space serves as a potential path for infections from the pharynx to the posterior mediastinum?
Which structure is responsible for closing off the larynx during swallowing?
Which structure is responsible for closing off the larynx during swallowing?
Which of the following is NOT a division of the pharynx?
Which of the following is NOT a division of the pharynx?
Which artery primarily supplies blood to the palatine tonsils?
Which artery primarily supplies blood to the palatine tonsils?
Which cranial nerve provides motor innervation to the pharynx, excluding a specific muscle?
Which cranial nerve provides motor innervation to the pharynx, excluding a specific muscle?
What structure forms the primary venous drainage for the pharynx?
What structure forms the primary venous drainage for the pharynx?
Where do the pharyngeal muscles converge posteriorly?
Where do the pharyngeal muscles converge posteriorly?
What is the primary anatomical attachment of the pharynx superiorly?
What is the primary anatomical attachment of the pharynx superiorly?
What does the oropharyngeal isthmus separate?
What does the oropharyngeal isthmus separate?
What is the primary function of the pharyngeal plexus?
What is the primary function of the pharyngeal plexus?
What structure forms a C-shaped attachment at the base of the skull?
What structure forms a C-shaped attachment at the base of the skull?
Which of the following correctly describes the relationship of the danger space?
Which of the following correctly describes the relationship of the danger space?
Which nerve provides sensory innervation to the anterior/superior nasopharynx?
Which nerve provides sensory innervation to the anterior/superior nasopharynx?
Which muscle of the pharynx is innervated by the glossopharyngeal nerve?
Which muscle of the pharynx is innervated by the glossopharyngeal nerve?
What forms the palatopharyngeal arch and serves as a landmark for the palatine tonsil?
What forms the palatopharyngeal arch and serves as a landmark for the palatine tonsil?
Which structure is located between the middle and inferior constrictor muscles?
Which structure is located between the middle and inferior constrictor muscles?
How are the pharyngeal constrictor muscles arranged?
How are the pharyngeal constrictor muscles arranged?
Which of the following describes the primary function of the longitudinal muscles of the pharynx?
Which of the following describes the primary function of the longitudinal muscles of the pharynx?
What anatomical feature connects muscles from each side in the pharynx?
What anatomical feature connects muscles from each side in the pharynx?
Which tonsils are part of the Waldeyer’s ring?
Which tonsils are part of the Waldeyer’s ring?
Which cartilage of the larynx is specifically shaped with a thick posterior lamina and a narrow anterior arch?
Which cartilage of the larynx is specifically shaped with a thick posterior lamina and a narrow anterior arch?
What is the function of the vocal folds in the larynx?
What is the function of the vocal folds in the larynx?
Where does the thyroid cartilage attach to extrinsic muscles of the larynx?
Where does the thyroid cartilage attach to extrinsic muscles of the larynx?
Which ligament connects the epiglottis to the thyroid cartilage?
Which ligament connects the epiglottis to the thyroid cartilage?
What is the significance of the rima glottidis in the laryngeal anatomy?
What is the significance of the rima glottidis in the laryngeal anatomy?
Which muscle is innervated by the external branch of the superior laryngeal nerve?
Which muscle is innervated by the external branch of the superior laryngeal nerve?
Which two structures does the larynx divide its cavity into?
Which two structures does the larynx divide its cavity into?
Which structure acts to close off the larynx during the swallowing process?
Which structure acts to close off the larynx during the swallowing process?
Which muscle is responsible for relaxing the vocal ligament?
Which muscle is responsible for relaxing the vocal ligament?
Which muscle is primarily responsible for abducting the arytenoids?
Which muscle is primarily responsible for abducting the arytenoids?
What is the primary artery supplying the superior laryngeal area?
What is the primary artery supplying the superior laryngeal area?
Which branch of the vagus nerve innervates the cricothyroid muscle?
Which branch of the vagus nerve innervates the cricothyroid muscle?
Which nerve provides sensory innervation below the vocal folds?
Which nerve provides sensory innervation below the vocal folds?
Which muscle acts to close the rima glottidis?
Which muscle acts to close the rima glottidis?
The inferior laryngeal artery branches from which trunk?
The inferior laryngeal artery branches from which trunk?
Which nerve is responsible for motor innervation to the majority of laryngeal muscles?
Which nerve is responsible for motor innervation to the majority of laryngeal muscles?
What is the primary role of the external branch of the superior laryngeal nerve?
What is the primary role of the external branch of the superior laryngeal nerve?
Which complication is associated with bilateral damage to the recurrent laryngeal nerve during thyroid surgery?
Which complication is associated with bilateral damage to the recurrent laryngeal nerve during thyroid surgery?
Which of the following conditions is least likely to cause hoarseness?
Which of the following conditions is least likely to cause hoarseness?
Where is the piriform fossa located in relation to the laryngeal inlet?
Where is the piriform fossa located in relation to the laryngeal inlet?
What symptom might indicate damage to the external superior laryngeal nerve after thyroidectomy?
What symptom might indicate damage to the external superior laryngeal nerve after thyroidectomy?
What treatment is required for post-thyroidectomy hemorrhage if pressure obstructing the airway increases?
What treatment is required for post-thyroidectomy hemorrhage if pressure obstructing the airway increases?
Which structure is at risk of injury during the dissection of the inferior thyroid artery?
Which structure is at risk of injury during the dissection of the inferior thyroid artery?
Which of the following best describes the rima glottidis?
Which of the following best describes the rima glottidis?
During which week does the thyroid gland begin its development?
During which week does the thyroid gland begin its development?
What anatomical feature does the migration of the thyroid leave on the tongue?
What anatomical feature does the migration of the thyroid leave on the tongue?
Which structure forms from the fusion of the medial nasal prominences?
Which structure forms from the fusion of the medial nasal prominences?
What is the consequence of a failure in the fusion of the maxillary prominences?
What is the consequence of a failure in the fusion of the maxillary prominences?
Which condition can arise if the thyroglossal duct does not obliterate properly?
Which condition can arise if the thyroglossal duct does not obliterate properly?
The lateral nasal prominence is involved in forming which part of the nose?
The lateral nasal prominence is involved in forming which part of the nose?
What embryological structure forms the base of the oral cavity?
What embryological structure forms the base of the oral cavity?
The thickenings that form during the development of the frontonasal prominence are known as:
The thickenings that form during the development of the frontonasal prominence are known as:
How does the inferior parathyroid gland's origin differ from that of the superior parathyroid gland?
How does the inferior parathyroid gland's origin differ from that of the superior parathyroid gland?
What is the primary nerve responsible for the sensory innervation of the anterior two-thirds of the tongue?
What is the primary nerve responsible for the sensory innervation of the anterior two-thirds of the tongue?
Which structure develops from the copula of Arch 3, and what is its innervation?
Which structure develops from the copula of Arch 3, and what is its innervation?
What differentiates the intrinsic muscles of the tongue from the palatoglossus muscle regarding innervation?
What differentiates the intrinsic muscles of the tongue from the palatoglossus muscle regarding innervation?
During tongue development, what happens after the bilateral lingual swellings of Arch 1 and Arch 2?
During tongue development, what happens after the bilateral lingual swellings of Arch 1 and Arch 2?
Which structure is primarily involved in the formation of the ear canal?
Which structure is primarily involved in the formation of the ear canal?
What is the primary type of tissue found in the pharyngeal arch?
What is the primary type of tissue found in the pharyngeal arch?
During which Carnegie stage do ears begin to appear?
During which Carnegie stage do ears begin to appear?
Which cranial nerve is responsible for innervating the muscles of mastication?
Which cranial nerve is responsible for innervating the muscles of mastication?
What does the mesoderm give rise to in the pharyngeal arch structures?
What does the mesoderm give rise to in the pharyngeal arch structures?
The pharyngeal apparatus is primarily lined with which type of embryonic tissue?
The pharyngeal apparatus is primarily lined with which type of embryonic tissue?
Which pharyngeal arch is associated with the glossopharyngeal nerve?
Which pharyngeal arch is associated with the glossopharyngeal nerve?
What structure marks the transition from the mouth to the pharynx in embryonic development?
What structure marks the transition from the mouth to the pharynx in embryonic development?
What happens to the 5th pharyngeal arch during development?
What happens to the 5th pharyngeal arch during development?
Which artery is associated with the 4th pharyngeal arch?
Which artery is associated with the 4th pharyngeal arch?
Study Notes
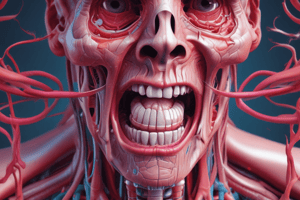
Oral Cavity
- Connects to: oropharynx via the oropharyngeal isthmus, nasal cavity via the incisive canal, and the external environment via the oral fissure.
- Boundaries: roof - hard and soft palate, floor - mylohyoid and geniohyoid muscles, lateral - cheeks (mainly buccinator muscle), anterior - oral fissure, posterior - oropharyngeal isthmus.
- Structures: Lips, philtrum (formed by fusion of medial nasal processes), median labial frenulum connecting lip to gum.
Soft Palate
- Composed of 4 muscles: tensor veli palatini, levator veli palatini, palatoglossus, palatopharyngeus.
- Innervation: All muscles are innervated by the vagus nerve (X) via the pharyngeal branch to the pharyngeal plexus except the tensor veli palatini, which is innervated by the mandibular nerve (V3) via a branch to the medial pterygoid.
- Palatoglossus acts to depress the soft palate and pull the pharynx upward, forward, and medially during swallowing.
- Tensor veli palatini opens the pharyngotympanic tube during yawning and swallowing.
- Musculus uvulae pulls the uvula superiorly.
Palate - Neurovasculature
- Arteries: greater and lesser palatine arteries which branch from the maxillary artery.
- Veins: follow the arteries and drain into the pterygoid or pharyngeal plexus.
- Lymphatics: drain to the deep cervical nodes.
- Innervation: branches of the pterygopalatine ganglion including the greater/lesser palatine nerve, and the nasopalatine nerve.
Tongue (glossus)
- Terminal sulcus separates the oral and pharyngeal surfaces.
- Divided left/right by the median sagittal septum.
- Papillae on the oral surface increase surface area.
- Lingual tonsil sits on the pharyngeal surface.
- Inferior surface: frenulum, lingual vein, fibriated fold.
Tongue - Muscles
- Intrinsic muscles alter the shape of the tongue.
- Extrinsic muscles control the tongue's position.
- All muscles are innervated by the hypoglossal nerve (XII) except palatoglossus, which is innervated by the vagus nerve (X).
- Hyoglossus, Styloglossus, and Palatoglossus are extrinsic muscles.
Tongue - Vessels
- Lingual artery enters the tongue through the oropharyngeal triangle, traveling above genioglossus and under hyoglossus.
- Dorsal lingual artery/vein: supplies the back of the tongue.
- Deep lingual artery/vein: supplies the inferior surface of the tongue and travels with the hypoglossal nerve.
- Sublingual artery/vein: supplies the underside of the tongue.
Tongue - Innervation
- Motor: Hypoglossal nerve (XII)- muscles of the tongue, Vagus nerve (X) - Palatoglossus
- Sensory: Anterior ⅔ - Trigeminal nerve (V) - general sensation, Facial nerve (VII) via chorda tympani - special sensation (taste).
- Posterior ⅓ - Glossopharyngeal nerve (IX) - general and special sensory.
- Epiglottis and soft palate: Vagus nerve (X) - PNS
- PNS: glossopharyngeal nerve (IX) via otic ganglion → auriculotemporal nerve.
- SNS: T1 via external carotid.
Salivary Glands
- Mostly small glands in the submucosa or mucosa of the oral epithelium.
- Larger glands are paired: parotid, submandibular, and sublingual.
Surgery of Salivary Glands
- Parotid gland: Injury to the facial nerve during parotidectomy can cause facial muscle weakness or complete palsy which can lead to eye complications.
- Submandibular gland: During surgery of the submandibular duct, nerves such as the lingual and marginal mandibular branch of the facial nerve can be injured.
Mumps
- Viral infection most commonly affecting the parotid gland.
- Symptoms include swelling, pain, fever, headache, fatigue, and weight loss.
- Complications can include facial nerve damage and localized ear pain.
Pharynx Overview
- The pharynx is a muscular tube located at the back of the throat, extending from the base of the skull to the level of the C5-6 vertebrae.
- It's a common pathway for both air and food, and is divided into three sections: nasopharynx, oropharynx, and laryngopharynx.
- These sections are separated by anatomical structures:
- Choanae: connect the nasopharynx to the nasal cavity.
- Oropharyngeal isthmus: connects the oropharynx to the oral cavity, formed by the palatoglossal folds, soft palate, and sulcus terminalis of the tongue.
- Laryngeal inlet: connects the laryngopharynx to the larynx and is gated by the epiglottis.
- Pharyngeal isthmus: connects the nasopharynx to the oropharynx, formed by the palatopharyngeal sphincter.
Pharynx Attachment
- The pharynx is made up of soft tissue and requires attachments for support.
- It's anchored to the base of the skull:
- Medial plate of the pterygoid process of sphenoid.
- Petrous part of the temporal bone.
- Pharyngeal tubercle.
- Superiorly, it's attached to the pterygomandibular raphe, connecting the superior constrictor muscle to the buccinator muscle.
- Posteriorly, the pharyngeal raphe, running from the esophagus to the pharyngeal tubercle, joins the pharyngeal muscles from each side.
- Anteriorly, it attaches to structures related to the hyoid bone:
- Stylohyoid, thyrohyoid, hyoepiglottic ligaments.
- Geniohyoid, mylohyoid, stylohyoid, thyrohyoid, sternohyoid, omohyoid muscles.
- Digastric muscle.
- Hyoglossus and genioglossus muscles.
- Inferiorly, it attaches to the thyroid and cricoid cartilages of the larynx.
Pharyngeal Tonsils
- These are collections of lymphoid tissue located in the pharynx.
- They drain into the deep cervical nodes and form the Waldeyer's ring, which is a ring of lymphatic tissue in the pharynx and back of the mouth, providing an immune defense against pathogens.
Pharyngeal Muscles
- These muscles are responsible for swallowing and other pharyngeal functions.
- They are divided into constrictor (circular) and longitudinal (vertical) muscles.
- All are innervated by the pharyngeal branch of the vagus nerve (CN X), except for the stylopharyngeus muscle which is innervated by the glossopharyngeal nerve (CN IX).
- Constrictor Muscles:
- Superior, middle, and inferior constrictors arranged like a telescope (inferior being the outermost).
- Form two sphincters:
- Palatopharyngeal sphincter: located at the pharyngeal isthmus.
- Inferior constrictor: acts as a sphincter at the junction with the esophagus.
- Oropharyngeal triangle (formed by the superior and middle constrictors) is associated with the oral cavity and the glossopharyngeal, stylopharyngeus, and lingual nerves.
- The space between the middle and inferior constrictors leads to the larynx, containing the internal laryngeal nerve and laryngeal arteries and veins.
- The recurrent laryngeal nerve and vessels are located under the inferior constrictor.
- Longitudinal Muscles (-pharyngeus):
- Stylopharyngeus: originates from the styloid process (innervated by glossopharyngeal nerve).
- Salpingopharyngeus: originates from the pharyngotympanic tube (cartilage part).
- Palatopharyngeus: originates from the soft palate, forms the palatopharyngeal arch (landmark for the palatine tonsil), also closes the oropharyngeal isthmus.
- These muscles run from the pharyngeal aponeurosis (inside the inner constrictor) and elevate the pharyngeal wall, helping to pull it up and over a bolus during swallowing.
Pharyngeal Spaces
- Parapharyngeal Space: located from the base of the skull to the greater horn of the hyoid bone, contains the internal maxillary artery, ascending pharyngeal artery, pterygoid venous plexus, and the mandibular division of the trigeminal nerve.
- Retropharyngeal Space: located posterior to the pharynx and esophagus, between the pretracheal and prevertebral fascia, containing retropharyngeal lymph nodes, fat, and vessels. It extends from the C6 to T5 vertebrae, joining the posterior mediastinum.
- Danger Space: located posterior to the retropharyngeal space, between the alar fascia and prevertebral fascia. It represents a potential path for infection from the pharynx to the superior and posterior mediastinum, extending from the skull to the thorax and from the superior mediastinum to the base of the diaphragm.
Pharyngeal Vasculature
- Arteries: supplied by branches of the external carotid artery:
- Ascending pharyngeal artery.
- Branches of the facial, lingual, and maxillary arteries.
- The tonsillar branch of the facial artery is the major blood supply to the palatine tonsil.
- Veins: drain into the pharyngeal venous plexus which then drains:
- Superiorly: pterygoid plexus → retromandibular vein → internal jugular vein (IJV).
- Inferiorly: directly into the IJV.
Pharyngeal Innervation
- Pharyngeal Plexus: located over the middle constrictor in the retropharyngeal space.
- Functions: innervates the pharynx and soft palate.
- Innervation Details:
- Motor: All pharyngeal muscles are innervated by the vagus nerve (CN X), except the stylopharyngeus, which is innervated by a branch of the glossopharyngeal nerve (CN IX).
- Sensory: Sensory innervation is primarily by the glossopharyngeal nerve (CN IX), except for:
- Anterior and superior nasopharynx: maxillary nerve (CN V2).
- Inferior laryngopharynx: internal branch of the vagus nerve (CN X).
- This combination of nerves explains the gag reflex, where stimulation of the pharyngeal mucosa triggers a response mediated by both the glossopharyngeal (sensory) and vagus (motor) nerves.
- Pharyngeal Plexus Formation:
- Pharyngeal branches (CN X): major motor branches.
- External laryngeal nerve.
Larynx
- Function: Respiration, phonation, effort closure, swallowing
- Structure: Made up of paired and unpaired cartilages
- Unpaired: Epiglottis, thyroid, cricoid
- Paired: Arytenoid, corniculate, cuneiform
- Relations:
- Laryngopharynx via laryngeal inlet (gated by epiglottis)
- Trachea at C5-6
Laryngeal Cartilages
- Cricoid: Thick lamina posteriorly, narrow arch anteriorly
- Two depressions on posterior surface for esophagus at center and posterior cricoarytenoid muscle
- Thyroid: Superior and inferior horns
- Laryngeal prominence: Adam's apple
- Oblique line: Site of attachment for extrinsic muscles of the larynx (sternothyroid, thyrohyoid, inferior constrictor)
- Epiglottis: Attaches via thyroepiglottic ligament to thyroid cartilage
- Arytenoids:
- Base: Articulates with cricoid cartilage
- Apex: Articulates with corniculate cartilage
- Attachment for vocal ligament, vocalis muscle, vestibular ligament, and cricoarytenoid muscle
- Cuneiform: Floats in quadrangular membrane
Laryngeal Ligaments
-
Extrinsic Ligaments:
- Hyoepiglottic and thyroepiglottic ligaments
- Thyrohyoid membrane: Forms median and lateral thyrohyoid ligaments
- Cricotracheal ligament
-
Intrinsic Ligaments:
- Quadrangular membrane: Forms vestibular ligament (false vocal cord)
- Cricothyroid ligament: Forms vocal ligament (true vocal cord)
- Vestibular ligament: Attaches from epiglottis to thyroid cartilage and arytenoids
- Vocal ligament: Attaches from lateral epiglottis to thyroid and arytenoid cartilage
- Vestibular fold: Covered by vestibular ligament
- Vocal fold: Covered by vocal ligament
- Rima vestibuli: Triangular space formed by vestibular folds
- Rima glottidis: Triangular space formed by vocal folds
Laryngeal Muscles
- Innervation: All innervated by vagus nerve (X)
- Cricothyroid: Via external branch of superior laryngeal nerve (of vagus nerve)
- All others: Via recurrent laryngeal branch
- Muscles:
- Cricothyroid: Tenses the vocal ligament
- Vocalis: Relaxes the vocal ligament (runs adjacent to vocal ligament)
- Thyroarytenoids: Relax the vocal ligament
- Lateral cricoarytenoids: Adduct arytenoids (closes rima glottidis)
- Transverse arytenoids: Adduct arytenoids (closes rima glottidis)
- Oblique arytenoids: Adduct arytenoids (closes rima glottidis)
- Posterior cricoarytenoids: Abducts arytenoids (opens rima glottidis)
Laryngeal Cavities
- Vestibule: Superior to vestibular folds
- Middle: Between vestibular and vocal folds, bulges to form laryngeal ventricle and saccule (produces mucus for lubrication)
- Infraglottic space: Inferior to vocal folds
Neurovasculature
-
Superior Branches:
- Arteries: Superior laryngeal (external carotid)
- Veins: Superior laryngeal → superior thyroid → internal jugular vein (IJV)
- Lymph: Superior deep cervical
- Nerves: Superior laryngeal
- External branch: Motor to cricothyroid muscle
- Internal branch: Sensory down to vocal folds
-
Inferior Branches:
- Arteries: Inferior laryngeal (thyrocervical trunk)
- Veins: Inferior laryngeal → inferior thyroid vein → brachiocephalic vein
- Lymph: Inferior deep cervical
- Nerves: Recurrent laryngeal
- Sensory: below vocal folds
- Motor: To all other laryngeal muscles (except cricothyroid)
- Travels: Around arch of aorta on left or under subclavian artery on right
Hoarseness
- Symptomatic: Not a disease
- Aetiology:
- Overuse: Screaming, singing, excessive coughing
- Toxins: Tobacco, caffeine, alcohol
- Polyps: On vocal cords
- Cancer: Throat, thyroid, lung
- Nerve or muscle conditions: Recurrent laryngeal nerve
- Left: Often affected during cardiac surgery
- Right: Apical lung tumor, thyroid cancer, aortic aneurysm
- Stomach acid reflux:
Thyroidectomy
- Structures at Risk:
- External superior laryngeal nerve: → cricothyroid muscle weakness (usually tenses vocal cord) → weak voice, inability to sing, lower pitch
- Recurrent laryngeal nerve: During dissection of inferior thyroid artery → vocal cord towards midline
- Unilateral: Hoarse voice
- Bilateral: Airway obstruction requiring tracheostomy
- Parathyroid glands: → hypocalcemia
Common Sites of Foreign Body Lodgement
- Piriform Fossa: On either side of laryngeal inlet, branches of internal laryngeal and recurrent laryngeal nerves at risk
- Vallecula: Depression anterior to epiglottis
- Rima Glottidis: Narrowest part of larynx, objects or their removal can damage vocal cords
- Dehiscence of Killian: Between cricopharyngeal muscle and upper esophagus
- Vocal folds: May have a globus sensation (feeling of a lump in the throat)
- Retropharyngeal space: Posterior wall of pharynx, may have a retropharyngeal abscess
- Hypopharynx: Inferior part of pharynx, may have a hypopharyngeal cancer
Time Frame of Head and Neck Development
- Carnegie Stage 15 (Week 4): Pharyngeal apparatus, tongue, thyroid, and face begin developing.
- Carnegie Stage 16 (Week 6): Ears appear.
- Carnegie Stage 23 (Week 8): Eyes move medially, ears move superiorly.
Pharyngeal Apparatus Development
- Develops between the 4th and 8th week after fertilization.
- Location: Future head and neck.
- Key outcomes: Craniofacial development.
- Associated with the gut tube, lined with endoderm.
- At the oropharyngeal membrane (between mouth and pharynx), endoderm transitions to ectoderm.
Pharyngeal Apparatus
- Pharyngeal arch: Entire structure including ectoderm, mesoderm, and endoderm.
- Pharyngeal clefts (external): Invaginations of ectoderm.
- Pharyngeal pouches (internal): Evaginations of endoderm.
- Cranial nerves innervate each arch and its structures.
Pharyngeal Arches
- Separated by pharyngeal clefts and pouches.
- Contain 4 structural components:
- Skeletal/cartilage tissue: Mesoderm.
- Muscular tissue: Mesoderm.
- Sensory and motor nerves: Neural tissue from the brain.
- Arch artery.
Pharyngeal Arches: Summary
- Arch 1: Skeletal tissue - Zygomatic bone, maxilla, mandible, incus, malleus; Muscular derivative - Muscles of mastication; Innervation - Trigeminal nerve (CN V2 and V3); Vasculature - Maxillary artery.
- Arch 2: Skeletal tissue - Lower part of the inner ear bone (upper part of the hyoid bone), stapes, styloid process, stylohyoid ligament (upper hyoid); Muscular derivative - Muscles of facial expression (superior to muscles of mastication); Innervation - Facial nerve (CN VII); Vasculature - Stapedial artery (embryo)/caroticotympanic artery.
- Arch 3: Skeletal tissue - Lower part of hyoid bone; Muscular derivative - Stylopharyngeus muscle; Innervation - Glossopharyngeal nerve (CN IX); Vasculature - Common carotid artery and 1st part of internal carotid.
- Arch 4 & 6: Skeletal tissue - Pharyngeal and laryngeal cartilages (merge to form thyroid and pharynx); Muscular derivative - Laryngeal muscles; Innervation - Branches of vagus nerve (Arch 4 - superior laryngeal nerve, Arch 6 - recurrent laryngeal nerve); Vasculature - Arch 4 - right subclavian artery and aortic arch, Arch 6 - ductus arteriosus and pulmonary artery.
- Arch 5: Disappears.
Pharyngeal Clefts and Pouches: Summary
- 1st Cleft and Pouch: Merge to form the ear canal; Tympanic membrane formed by intermediate mesoderm between ectoderm and endoderm.
- 2nd Cleft and Pouch: Pouch 2 invades mesenchyme to form palatine tonsils (lymphatic tissue invades later); Cleft 2 migrates downwards to fuse with clefts 3 and 4 for smooth neck (persistence of clefts can lead to fluid accumulation).
- 3rd Cleft and Pouch: Inferior parathyroid gland and thymus develop from Pouch 3; Thymus moves inferiorly, pulling inferior parathyroid gland with it (hence inferior parathyroid gland is superior to the superior parathyroid gland).
- 4th Cleft and Pouch: Superior parathyroid gland - Pouch 4; Attaches to thyroid and becomes superior to Pouch 3 derivatives.
Tongue Development
-
Timing: Week 4.
-
Location: Swelling of pharyngeal apparatus.
-
Key outcomes: Structures near pharyngeal apparatus.
-
Relating tongue, pharyngeal apparatus, and sensory innervation:
- Anterior ⅔ of tongue: Develops from bilateral lingual swellings of Arch 1 and 2; Innervated by lingual nerve (branch of V3) and carries additional special sensory fibers from CN7 (facial nerve) via the chorda tympani.
- Posterior ⅓ of tongue: Develops from the copula of Arch 3; Innervated by glossopharyngeal nerve (general and special sensation).
- Epiglottis: Develops from Arch 6; Innervated by the vagus nerve (general and special sensation).
Musculature of the Tongue
- Originates from post-otic somites.
- Intrinsic muscles are innervated by hypoglossal nerve, except palatoglossus muscle.
Thyroid Development
-
Timing: Week 3.5.
-
Location: Floor of the primordial pharynx.
-
Key outcomes: Adult anatomical development of thyroid gland.
-
Embryological origin and development: Thyroid gland develops from thyroid diverticulum (between anterior ⅔ and posterior ⅓ of the tongue); Migrates inferiorly, anterior to hyoid bone during development; Migration leaves a depression in the tongue (foramen cecum) and creates a duct (thyroglossal duct) that can lead to infection or develop into the pyramidal/third lobe of the thyroid.
Facial and Palatine Development
-
Timing: Week 4 to 8 (continuous development through fetal and post-partum life).
-
Location: Cephalic region.
-
Key outcomes: Bilateral fusion, division of oral and nasal cavities.
-
Development involves 5 prominences:
- 1 frontonasal prominence.
- 2 maxillary prominences.
- 2 mandibular prominences.
Frontonasal Prominence
-
Formed from mesenchyme near the brain.
-
Develops 2 thickenings near the lateral edges (nasal placodes) during week 5.
-
Each nasal placode develops a central depression (nasal pit) by week 6.
-
Nasal pit opens to form nostril and connect to the gut tube.
-
Nasal Placodes
- Medial nasal prominence: Forms intermaxillary process, philtrum, columella, and primary palate; Fuses during week 7 to form the intermaxillary process (nasal septum, philtrum, and primary palate); Failure of fusion creates medial cleft lip.
- Lateral nasal prominence: Forms ala of the nose; Separated from the maxillary prominence by the nasolacrimal groove (failure of fusion creates an oblique facial cleft).
Maxillary Prominence
- Formed by the upper part of Arch 1.
- Gives rise to 2 palatine shelves which form the secondary palate after midline fusion (also forms the uvula); Failure of fusion creates bifid uvula and cleft palate.
- Secondary palate fuses with primary palate, leaving an incisive foramen (conducting nasopalatine nerve and sphenopalatine arteries).
- Forms the cheeks.
Mandibular Prominence
- Formed by the lower part of Arch 1.
- Forms the mandible and base of the oral cavity.
- Insufficient expansion can prevent the tongue from coming down.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the detailed anatomy of the oral cavity and soft palate. This quiz covers essential structures, boundaries, and the muscles involved in palate functions. Test your knowledge on the connections and innervations pertinent to these areas.