Podcast
Questions and Answers
What is the primary role of the tight junctions between endothelial cells in the blood vessels of the iris and retina?
What is the primary role of the tight junctions between endothelial cells in the blood vessels of the iris and retina?
- To facilitate the passage of blood-borne molecules into the eye.
- To promote rapid drainage of ocular fluids.
- To restrict entry of immune cells and large molecules into the eye. (correct)
- To actively transport nutrients to the retinal cells.
Why are there no patent lymphatic vessels within the anterior chamber, vitreous cavity, or retina of mammals?
Why are there no patent lymphatic vessels within the anterior chamber, vitreous cavity, or retina of mammals?
- To encourage direct transport of antigens to the trabecular meshwork.
- To force antigen and APC transport via the bloodstream to the spleen rather than through lymphatic channels. (correct)
- To reduce the reliance on the spleen for immune responses.
- To prevent the flow of aqueous humor to the canal of Schlemm.
Which of the following does NOT contribute to the defense mechanisms of the ocular surface (cornea and conjunctiva) against external antigens?
Which of the following does NOT contribute to the defense mechanisms of the ocular surface (cornea and conjunctiva) against external antigens?
- The constant blinking to remove surface antigens.
- The secretion of tears to irrigate and remove antigens.
- The lymphatic drainage system in the cornea to filter pathogens. (correct)
- The temperature of the central cornea.
What is the role of Langerhans cells in the conjunctival immune system?
What is the role of Langerhans cells in the conjunctival immune system?
What is the primary route of drainage for the aqueous humour in the eye?
What is the primary route of drainage for the aqueous humour in the eye?
Which of the following best describes the immune response of the eye?
Which of the following best describes the immune response of the eye?
The conjunctival MALT is mainly responsible for:
The conjunctival MALT is mainly responsible for:
Which of the following is NOT a primary function of the tear film in ocular surface defense?
Which of the following is NOT a primary function of the tear film in ocular surface defense?
What is the significance of the intact epithelial surface of the cornea and conjunctiva?
What is the significance of the intact epithelial surface of the cornea and conjunctiva?
Where do the lateral and nasal portions of the conjunctiva primarily drain lymphatically?
Where do the lateral and nasal portions of the conjunctiva primarily drain lymphatically?
Which of these is NOT a component of the tear film's antibacterial arsenal?
Which of these is NOT a component of the tear film's antibacterial arsenal?
In the context of ocular surface defense, what is the primary role of sIgA?
In the context of ocular surface defense, what is the primary role of sIgA?
What is a key characteristic of the sub-epithelial layer of the conjunctiva, especially during chronic infections?
What is a key characteristic of the sub-epithelial layer of the conjunctiva, especially during chronic infections?
Which of the following best describes the function of ceruloplasmin in the tear film?
Which of the following best describes the function of ceruloplasmin in the tear film?
What is most likely not implicated in the development of blepharitis?
What is most likely not implicated in the development of blepharitis?
What is the primary method by which the tear film combats foreign particles and bacteria on the ocular surface?
What is the primary method by which the tear film combats foreign particles and bacteria on the ocular surface?
In cases of Fuch's heterochromic cyclitis (FHC), which cytokine is typically observed at increased levels?
In cases of Fuch's heterochromic cyclitis (FHC), which cytokine is typically observed at increased levels?
What is the primary characteristic of carcinoma-associated retinopathy (CAR) and melanoma-associated retinopathy (MAR)?
What is the primary characteristic of carcinoma-associated retinopathy (CAR) and melanoma-associated retinopathy (MAR)?
Which cells are suggested to be involved with drusen development in age-related macular degeneration (AMD)?
Which cells are suggested to be involved with drusen development in age-related macular degeneration (AMD)?
What is a commonality in the immunopathology observed in the choroid and retinal tissues during uveitis?
What is a commonality in the immunopathology observed in the choroid and retinal tissues during uveitis?
Besides systemic diseases, what is another cause of posterior uveitis?
Besides systemic diseases, what is another cause of posterior uveitis?
What is the proposed mechanism behind the inflammatory response seen in retinitis pigmentosa?
What is the proposed mechanism behind the inflammatory response seen in retinitis pigmentosa?
What role does complement activation play in the development of age-related macular degeneration (AMD)?
What role does complement activation play in the development of age-related macular degeneration (AMD)?
What is the typical outcome of anti-retinal antibodies detected after laser photocoagulation of ischemic retina?
What is the typical outcome of anti-retinal antibodies detected after laser photocoagulation of ischemic retina?
What is the primary function of the immune system in relation to the eye?
What is the primary function of the immune system in relation to the eye?
Which type of cells are implicated in the tear production issues seen in early stages of some ocular conditions?
Which type of cells are implicated in the tear production issues seen in early stages of some ocular conditions?
What therapeutic approach has demonstrated success based on the content related to early gland destruction?
What therapeutic approach has demonstrated success based on the content related to early gland destruction?
Which of the following structures are not specifically mentioned in the text as having individual defense mechanisms?
Which of the following structures are not specifically mentioned in the text as having individual defense mechanisms?
What is the primary characteristic of the immune response in individuals with Atopic Keratoconjunctivitis (AKC), as opposed to Vernal Keratoconjunctivitis (VKC)?
What is the primary characteristic of the immune response in individuals with Atopic Keratoconjunctivitis (AKC), as opposed to Vernal Keratoconjunctivitis (VKC)?
Which cell type is primarily involved in T-cell interactions, potentially leading to fibrosis and scarring of the conjunctiva during inflammatory processes?
Which cell type is primarily involved in T-cell interactions, potentially leading to fibrosis and scarring of the conjunctiva during inflammatory processes?
What common theme underlies the conditions mentioned when discussing the role of defense mechanisms?
What common theme underlies the conditions mentioned when discussing the role of defense mechanisms?
Which of the following conditions mentioned is NOT primarily associated with an autoimmune response?
Which of the following conditions mentioned is NOT primarily associated with an autoimmune response?
In the context of ocular surface disorders, what is a significant risk associated with using topical corticosteroids in individuals with AKC?
In the context of ocular surface disorders, what is a significant risk associated with using topical corticosteroids in individuals with AKC?
What is the main concern driving the need for a balanced immune response in the eye?
What is the main concern driving the need for a balanced immune response in the eye?
Which of the following therapeutic agents is primarily responsible for reducing cytokine production by T cells and eosinophils in both VKC and AKC?
Which of the following therapeutic agents is primarily responsible for reducing cytokine production by T cells and eosinophils in both VKC and AKC?
What is the primary source of cellular corneal defense given the cornea's avascular nature?
What is the primary source of cellular corneal defense given the cornea's avascular nature?
According to content, what is the focus of the subsequent module (Unit 3) following the discussion of the immune system and ocular abnormalities?
According to content, what is the focus of the subsequent module (Unit 3) following the discussion of the immune system and ocular abnormalities?
What is a main characteristic of non-infectious immune-related responses of the cornea?
What is a main characteristic of non-infectious immune-related responses of the cornea?
In which specific situation is the systemic immune system known to have prior contact with ocular antigens, potentially leading to a more pronounced immune response?
In which specific situation is the systemic immune system known to have prior contact with ocular antigens, potentially leading to a more pronounced immune response?
Which of the following statements best describes the relationship between HLA-DR antigen expression and the growth rate of a pterygium?
Which of the following statements best describes the relationship between HLA-DR antigen expression and the growth rate of a pterygium?
Which of the following is a characteristic feature of Miller Fisher syndrome?
Which of the following is a characteristic feature of Miller Fisher syndrome?
In orbital myositis, what is a common symptom, according to the text?
In orbital myositis, what is a common symptom, according to the text?
Which of the following cell types is most commonly involved in the infiltration of orbital tissue in thyroid eye disease?
Which of the following cell types is most commonly involved in the infiltration of orbital tissue in thyroid eye disease?
Besides idiopathic causes, what is another potential cause of orbital myositis?
Besides idiopathic causes, what is another potential cause of orbital myositis?
What is the key autoantibody found in Miller Fisher syndrome?
What is the key autoantibody found in Miller Fisher syndrome?
Which of these is a characteristic of thyroid-associated ophthalmopathy regarding the extraocular muscles?
Which of these is a characteristic of thyroid-associated ophthalmopathy regarding the extraocular muscles?
What is a key feature of the pathophysiology of myasthenia gravis, based on the material?
What is a key feature of the pathophysiology of myasthenia gravis, based on the material?
What is a typical characteristic finding in the extraocular muscles of patients with early thyroid associated ophthalmopathy?
What is a typical characteristic finding in the extraocular muscles of patients with early thyroid associated ophthalmopathy?
Flashcards
TH2 Response
TH2 Response
A type of immune response characterized by the production of certain cytokines like IL-4 and IL-5. It is often associated with allergic reactions and parasitic infections.
TH1 Response
TH1 Response
A type of immune response characterized by the production of cytokines like IFN-gamma and IL-2. It is often associated with intracellular infections and autoimmune diseases.
Vernal Keratoconjunctivitis (VKC)
Vernal Keratoconjunctivitis (VKC)
A condition affecting the conjunctiva characterized by a predominantly TH2 immune response, involving mast cells and eosinophils.
Atopic Keratoconjunctivitis (AKC)
Atopic Keratoconjunctivitis (AKC)
Signup and view all the flashcards
Cornea
Cornea
Signup and view all the flashcards
Langerhans Cells
Langerhans Cells
Signup and view all the flashcards
Limbus
Limbus
Signup and view all the flashcards
Mooren's Ulcer
Mooren's Ulcer
Signup and view all the flashcards
Conjunctival drainage
Conjunctival drainage
Signup and view all the flashcards
Conjunctiva's cellular makeup
Conjunctiva's cellular makeup
Signup and view all the flashcards
Tear film's role in defense
Tear film's role in defense
Signup and view all the flashcards
Antibacterial components of tear film
Antibacterial components of tear film
Signup and view all the flashcards
Tear film components: ceruloplasmin and complement
Tear film components: ceruloplasmin and complement
Signup and view all the flashcards
sIgA antibody's function
sIgA antibody's function
Signup and view all the flashcards
Blepharitis: What is it?
Blepharitis: What is it?
Signup and view all the flashcards
Blepharitis: Cause of inflammation
Blepharitis: Cause of inflammation
Signup and view all the flashcards
Blood-retinal barrier
Blood-retinal barrier
Signup and view all the flashcards
Blood-aqueous barrier
Blood-aqueous barrier
Signup and view all the flashcards
Absence of lymphatic vessels in the eye
Absence of lymphatic vessels in the eye
Signup and view all the flashcards
Antigen-presenting cells in the eye
Antigen-presenting cells in the eye
Signup and view all the flashcards
Conjunctival MALT
Conjunctival MALT
Signup and view all the flashcards
Langerhans cells in the conjunctiva
Langerhans cells in the conjunctiva
Signup and view all the flashcards
Cornea's innate defenses
Cornea's innate defenses
Signup and view all the flashcards
Corneal epithelial barrier
Corneal epithelial barrier
Signup and view all the flashcards
Immune System
Immune System
Signup and view all the flashcards
Innate Immune System
Innate Immune System
Signup and view all the flashcards
Posterior Uveitis
Posterior Uveitis
Signup and view all the flashcards
Adaptive Immune System
Adaptive Immune System
Signup and view all the flashcards
Uveitis
Uveitis
Signup and view all the flashcards
Posterior Uveitis
Posterior Uveitis
Signup and view all the flashcards
T Cells
T Cells
Signup and view all the flashcards
Uveitis
Uveitis
Signup and view all the flashcards
Fuch's Heterochromic Cyclitis (FHC)
Fuch's Heterochromic Cyclitis (FHC)
Signup and view all the flashcards
Myasthenia Gravis
Myasthenia Gravis
Signup and view all the flashcards
Immune Response in Age-Related Macular Degeneration (AMD)
Immune Response in Age-Related Macular Degeneration (AMD)
Signup and view all the flashcards
Scleritis
Scleritis
Signup and view all the flashcards
Retinal Antigen Sensitization
Retinal Antigen Sensitization
Signup and view all the flashcards
Retinitis Pigmentosa
Retinitis Pigmentosa
Signup and view all the flashcards
Thyroid Eye Disease
Thyroid Eye Disease
Signup and view all the flashcards
Autoimmune Retinopathy
Autoimmune Retinopathy
Signup and view all the flashcards
Autoimmune response
Autoimmune response
Signup and view all the flashcards
Study Notes
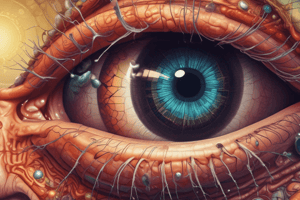
Ocular Immune System
- The eye has mechanisms to protect itself from pathogens, known as immune privilege. This involves limited inflammatory responses and modified immunity.
- Factors contributing to immune privilege include a blood-ocular barrier, composed of tight junctions that prevent blood-borne immune cells from entering the eye, and the absence of lymphatic vessels. Instead, the spleen plays the main role in processing antigens.
- Cells lining the anterior chamber and subretinal space actively suppress responses to intraocular antigens, a process called Anterior Chamber Associated Immune Deviation (ACAID).
- Tears act as a barrier against foreign antigens through mechanical removal, temperature inhibition of microbes, and irrigation.
- The cornea and conjunctiva have immune cells that protect against pathogens, including Langerhans cells, T cells, and B cells.
- The tear film components like slgA, IgG, IgE, lysozyme, lactoferrin, transferrin, and complement protect against microbes.
- Blepharitis, an inflammation of the eyelid margins, is frequently associated with bacterial infections, particularly staphylococci.
- Conjunctival scarring can occur in certain inflammatory conditions, impacting the lacrimal glands (leading to dry eye)
Tear Film and Function
- The tear film protects the ocular surface in four ways: trapping foreign particles with mucins, washing away microbes, containing antimicrobial proteins (like lysozyme), and containing immune cells.
- Specific proteins are crucial for tear film function in protecting the eye.
Corneal Immunology
- The cornea is avascular, so defence relies on the limbus and anterior chamber.
- Non-infectious corneal inflammatory disorders like Mooren's ulcer and Terrien's marginal degeneration can occur.
- Viral infections (like herpes simplex) can have an immune response. This response can be mild or significant.
- Corneal transplantation has a high success rate due to corneal avascularity and lack of immune cell activation. This can be impaired/lower in conditions where the integrity of the vasculature is affected.
Scleral Immunology
- Sclera inflammation (scleritis) can have different localizations and causes. This can effect the cornea (leading to melt).
- Systemic diseases (like rheumatoid arthritis, SLE, Wegener's granulomatosis, and PAN) and infections (like acanthamoeba) can be associated with scleritis.
Immunology of the Uvea
- The uvea (iris, ciliary body, choroid) has limited lymphatic drainage and tight junctions to prevent immune infiltration.
- Inflammation in the uvea (uveitis) can have various causes and involve different immune cells.
- Acute anterior uveitis, involving PMNs and T cells is common, typically characterized by a red eye.
- A variety of ocular inflammations can occur elsewhere affecting the uvea, and potentially involve systemic diseases.
Immunology of the Neuroretina and RPE
- The neuroretina has antigen components, including retinal s-antigen and IRBP, that can trigger an immune response.
- The retina's immune response is complex, possibly related to systemic issues like melanoma-associated retinopathy.
Immunology of the Orbit
- The optic nerve can be affected by inflammation, sometimes associated with multiple sclerosis, with an immune response similar to conditions in the brain.
- Grave's disease, characterized by exophthalmos, involves the extraocular muscles and orbital fat, which are infiltrated by T cells.
- Myasthenia gravis, results in weakness of the muscles, because of antibodies targeting the acetylcholine receptor. Damage to the muscles can lead to strabismus (eye misalignment).
- Orbital myositis involves inflammation of the orbital muscles, either idiopathic or associated with systemic diseases or infection.
Dry Eye and Role of the Lacrimal Gland
- Damage to the lacrimal gland (part of the tear production system) results in decreased tear volume and changes in tears. This is observed in some dry eye syndromes, like Sjögren syndrome and sarcoidosis.
- T cell activation is suspected to cause tear production issue and destruction of the secretory cells (acinar) in the early stages of the issue, possibly respondable to treatment (like topical cyclosporin).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.