Podcast
Questions and Answers
During the general survey, when does the process of observing the patient typically begin?
During the general survey, when does the process of observing the patient typically begin?
- After vital signs have been recorded.
- During the interviewing and history-taking process. (correct)
- After the initial physical assessment is completed.
- Only when objective data collection starts.
What is the primary reason for healthcare professionals to conduct a general survey of a patient?
What is the primary reason for healthcare professionals to conduct a general survey of a patient?
- To only collect subjective data reported by the patient.
- To formulate detailed care plans without delay.
- To develop initial impressions and plans for further data collection. (correct)
- To immediately begin treatment interventions.
Why are vital signs considered important indicators in patient assessment?
Why are vital signs considered important indicators in patient assessment?
- They primarily guide the collection of subjective data.
- They are solely used to confirm the patient's self-reported symptoms.
- They are only relevant in emergency situations.
- They directly reflect both physiological status and response to interventions. (correct)
Which of the following assessment findings would indicate the need to activate a rapid response team?
Which of the following assessment findings would indicate the need to activate a rapid response team?
What immediate action should a nurse take when a patient exhibits acute distress and a change in mental status?
What immediate action should a nurse take when a patient exhibits acute distress and a change in mental status?
Which of the following is the MOST appropriate equipment to use when assessing a patient's oxygen saturation?
Which of the following is the MOST appropriate equipment to use when assessing a patient's oxygen saturation?
What does the general survey primarily help healthcare providers form?
What does the general survey primarily help healthcare providers form?
Which elements are key components of the 'physical appearance' aspect within a general survey?
Which elements are key components of the 'physical appearance' aspect within a general survey?
When assessing a patient's hygiene and dress, what is a key consideration beyond cleanliness?
When assessing a patient's hygiene and dress, what is a key consideration beyond cleanliness?
What should a healthcare provider observe when assessing a patient's skin color during a general survey?
What should a healthcare provider observe when assessing a patient's skin color during a general survey?
During the assessment of a patient’s behavior, what aspect of facial expressions is most important to note?
During the assessment of a patient’s behavior, what aspect of facial expressions is most important to note?
What are the key elements to assess when evaluating a patient's level of consciousness?
What are the key elements to assess when evaluating a patient's level of consciousness?
When assessing mobility, what should be noted about a patient's posture?
When assessing mobility, what should be noted about a patient's posture?
Which of the following best describes the assessment of a patient’s gait?
Which of the following best describes the assessment of a patient’s gait?
What is the primary purpose of monitoring vital signs?
What is the primary purpose of monitoring vital signs?
What is the normal range for oral temperature in degrees Celsius?
What is the normal range for oral temperature in degrees Celsius?
If a patient's oral temperature is 37°C, what would be the approximate normal axillary temperature?
If a patient's oral temperature is 37°C, what would be the approximate normal axillary temperature?
What does the pulse rate primarily reflect?
What does the pulse rate primarily reflect?
What is the normal heart rate range for an adult, measured in beats per minute (bpm)?
What is the normal heart rate range for an adult, measured in beats per minute (bpm)?
When assessing respiration, what two components are observed?
When assessing respiration, what two components are observed?
What is the typical respiratory rate range for adults?
What is the typical respiratory rate range for adults?
Pulse oximetry measures which of the following?
Pulse oximetry measures which of the following?
A healthy adult's pulse oximetry reading (SpO2) should typically fall within what range?
A healthy adult's pulse oximetry reading (SpO2) should typically fall within what range?
What physiological event is indicated by systolic blood pressure?
What physiological event is indicated by systolic blood pressure?
What does the diastolic blood pressure reading represent?
What does the diastolic blood pressure reading represent?
According to adult blood pressure guidelines, what range is indicative of Stage 1 hypertension?
According to adult blood pressure guidelines, what range is indicative of Stage 1 hypertension?
What is the numeric pain intensity scale used for?
What is the numeric pain intensity scale used for?
When assessing pain, what aspects should be evaluated?
When assessing pain, what aspects should be evaluated?
What type of question assists in determining the 'quality' of a patient's pain?
What type of question assists in determining the 'quality' of a patient's pain?
Flashcards
General Survey
General Survey
Begins during the interviewing and history taking process.
Indicators of acute situation
Indicators of acute situation
Extreme anxiety, acute distress, pallor, cyanosis, change in mental status
Concerning respiratory findings
Concerning respiratory findings
Less than 10 or greater than 32 breaths/min, increased effort to breathe, oxygen saturation less than 92%
Concerning pulse findings
Concerning pulse findings
Signup and view all the flashcards
Concerning systolic blood pressure
Concerning systolic blood pressure
Signup and view all the flashcards
Concerning temperature findings
Concerning temperature findings
Signup and view all the flashcards
Concerning symptoms
Concerning symptoms
Signup and view all the flashcards
Objective Data Collection Equipment
Objective Data Collection Equipment
Signup and view all the flashcards
General survey
General survey
Signup and view all the flashcards
Components of mental notes
Components of mental notes
Signup and view all the flashcards
Physical appearance elements
Physical appearance elements
Signup and view all the flashcards
Behavior assessment focus
Behavior assessment focus
Signup and view all the flashcards
Level of consciousness
Level of consciousness
Signup and view all the flashcards
Speech Assessment Aspects
Speech Assessment Aspects
Signup and view all the flashcards
Mobility assessment areas
Mobility assessment areas
Signup and view all the flashcards
Normal posture
Normal posture
Signup and view all the flashcards
Normal gait
Normal gait
Signup and view all the flashcards
Anthropometric measurements
Anthropometric measurements
Signup and view all the flashcards
Vital signs reflect
Vital signs reflect
Signup and view all the flashcards
Common Vital Signs
Common Vital Signs
Signup and view all the flashcards
Normal oral temperature range
Normal oral temperature range
Signup and view all the flashcards
Adult heart rate range
Adult heart rate range
Signup and view all the flashcards
What respiration does
What respiration does
Signup and view all the flashcards
Normal respiration rate
Normal respiration rate
Signup and view all the flashcards
Pulse oximetry
Pulse oximetry
Signup and view all the flashcards
SpO2 range
SpO2 range
Signup and view all the flashcards
Blood pressure (BP)
Blood pressure (BP)
Signup and view all the flashcards
Systolic blood pressure
Systolic blood pressure
Signup and view all the flashcards
1-10 numeric pain scale
1-10 numeric pain scale
Signup and view all the flashcards
Dimensions of pain
Dimensions of pain
Signup and view all the flashcards
Study Notes
Istinye University
- Founded in 2015 by the 21st Century Anatolian Foundation, continuing the 25-year legacy of the MLPCare Group.
- MLPCare Group united three hospital brands: Liv Hospital, Medical Park, and VM Medical Park.
- The university aims to be among the distinguished universities in Turkey and the world, and produce new knowledge.
- Istinye University aims to provide quality and accessible healthcare services to the community.
General Survey, Vital Signs, and Pain Assessment
- Lecturer: Asst. Prof. Gizem Yağmur Yalçın
- HSF /Nursing (English) department
- Lecture: NUR012-Health Assessment
Outline
- The general survey is the first component of assessment.
- Vital signs include temperature, pulse, respirations, oxygen saturation, blood pressure, and pain.
- Pain assessment is important.
General Survey
- Begins during the interviewing and history-taking process.
- Healthcare professionals observe patients and develop initial impressions while collecting subjective data.
- Formulate plans for collecting objective physical data.
- Vital signs indicate the patient’s physiological status and response to the environment.
Acute Assessment
- Indicators include extreme anxiety, acute distress, pallor, cyanosis, and changes in mental status.
- The nurse begins interventions while continuing assessment.
- The nurse obtains all vital signs and requests help.
- A rapid response team may be called if something is going wrong or if the patient displays:
- Respirations less than 10 breaths/min or greater than 32 breaths/min
- Increased effort to breathe
- Oxygen saturation less than 92%
- Pulse less than 55 beats/min or greater than 120 beats/min
- Systolic BP less than 100 or greater than 170
- Temperature less than 35°C or greater than 39.5°C
- New onset of chest pain
- Agitation or restlessness
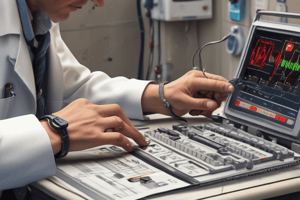
Objective Data Collection Equipment
- Scale
- Tape measure (for infants)
- Height bar
- Stethoscope
- Pulse oximeter
- Watch with second hand
- Thermometer
General Survey Components
- Mental notes of the patient’s overall behavior, physical appearance, and mobility
- Helps to form a global impression of the person.
Physical Appearance Factors
- Overall appearance
- Hygiene and dress
- Skin color
- Body structure and development
Mobility Factors
- Posture
- Range of motion
- Gait
Behaviour Factors
- Facial expressions
- Level of consciousness
- Speech
Physical Appearance - Overall Appearance
- Assess if the patient appears the stated age
- Check if the face and body is symmetrical
- Note obvious deformities
- Assess if the patient looks, well, ill, is in distress
Physical Appearance - Hygiene and Dress
- Observe clothes, hair, nails, and skin
- Assess if the clothing is appropriate for age, gender, culture, and weather
- Check is clothes is clean and neat, and for breath or body odors
- Assess if the hair and nails are well-kept and clean
Physical Appearance - Skin Color
- Observe skin tones and symmetry
- Note any redness, pallor, or cyanosis
- Check for lesions or variations in pigmentation.
- Note the amount, texture, quality, and distribution of hair.
Physical Appearance - Body Structure and Development:
- Assess if physical and sexual development is consistent with stated age
- Determine if the patient is obese or not
- Measure how tall the patient is
- Assess if the body parts are symmetrical
- Note fingertips
- Check for any joint abnormalities
Behavior - Facial Expressions
- Assess the face for symmetry
- Note expressions while the patient is at rest and during speech.
- Assess if movements are symmetrical
- Assess if the patient maintains eye contact appropriate to culture
Behavior - Level of Consciousness
- Check if the patient can state name, location, date, month, season, and time
- Assess if the patient is awake, alert, and oriented.
- Note any agitation, lethargy, or inattentiveness.
Behavior - Speech
- Listen to the speech pattern
- Measure how quickly someone is speaking
- Check if speech is clear
- Assess if words are appropriate
- Note fluency in language and need for an interpreter
Mobility - Posture
- Note how the patient sits and stands.
- Assess if the patient is sitting upright.
- When standing, check if the body is straight and aligned.
Mobility - Range of Motion
- Assess if the patient can move all limbs equally
- Check for any limitations
Mobility - Gait
- For the ambulatory patient, observe movements around the room
- Check if movements are coordinated
- Note any tremors or tics, as well as body parts that do not move
- Determine if the patient uses assistive devices.
Anthropometric Measurements
- Height and weight
- Body mass index (BMI)
Vital Signs
- Reflect health status, cardiopulmonary function, and overall body function.
- Establish a baseline to monitor a patient's condition.
- Evaluate responses to treatment and identify problems by monitoring risks for alterations in health.
Vital Signs - Temperature Normal Ranges
- Oral temperature: 35.8°C to 37.3°C
- Axillary temperature: 36.5°C or approximately 1°C lower than oral
- Tympanic temperature: 37.5°C or approximately equal to oral
- Temporal temperature: 37°C or approximately equal to oral
- Rectal temperature: 37.5°C or approximately 1°C warmer than oral
Pulse
- Contraction of the heart causes blood to flow forward, which creates a pressure wave.
- Normal Heart rate for an adult: 60 to 100 beats/min (bpm)
- Apical pulse: 60 to 100 beats/min and regular
Respiration
- Supplies oxygen to the body and eliminates carbon dioxide.
- One should discretely observe both inspiration and expiration.
- Count for 30 seconds and multiply by two to obtain breaths per minute.
- Normal respiratory rates for adults: 12 to 20 breaths/min and regular
Oxygen Saturation (SpO2)
- SpO2 should be 95% to 100
- Pulse oximetry measures oxygen saturation, and indicates arterial blood filling with oxygen
- Use a noninvasive technique to measure noninvasively
- Can indicate abnormal gas exchange; replace measurement of arterial blood gases for assessment of abnormalities
Blood Pressure (BP)
- Blood flow against arterial wall measurement
- This changes alongside contraction and relaxation of the heart
- Systolic blood pressure is max measured pressure when the artery walls contract
- Diastolic blood pressure is measured by arterial walls with contraction of the left ventricle
Pain
- This is the fifth vital sign
- It is important for assessments
- Location, duration, severity, quality, and alleviating/aggravating factors should be determined
- The numeric pain intensity scale with 10 numbers ranks pain from 0 (no pain) to 10 (worst possible pain)
- The higher the number selected, the more severe is the pain.
Symptoms Assessment
- Location - Find where the pain is and how intense it is in different locations
- Duration - Find when the patients first has pain
- Intensity - How much pain you have on a 0 to 10 scale
- Determine if there pain medications decrease intensity
Questions to Assess Symptoms:
- Describe the quality/description of the pain
- Describe what your pain feels like in your own words
- Describe alleviating/aggravating factors, what makes the pain worse, managing, heat packs helping, cold packs helping, activity, and sitting
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.