Podcast
Questions and Answers
What is the primary action of H2 antagonists related to gastric secretions?
What is the primary action of H2 antagonists related to gastric secretions?
- Neutralize stomach acid rapidly
- Increase stomach acidity
- Suppress volume and acidity of parietal cell secretions (correct)
- Enhance parietal cell secretion volume
Why should antacids not be taken at the same time as H2 receptor antagonists?
Why should antacids not be taken at the same time as H2 receptor antagonists?
- Antacids can cause excessive gastric acid production
- Absorption of H2 receptor blockers will be diminished (correct)
- Antacids block the action of H2 blockers at receptors
- Both medications can cause excessive drowsiness
What is a common side effect of magnesium hydroxide when used as an antacid?
What is a common side effect of magnesium hydroxide when used as an antacid?
- Diarrhea
- Dizziness
- Nausea
- Constipation (correct)
What condition can result from administering calcium carbonate antacids with milk?
What condition can result from administering calcium carbonate antacids with milk?
What classification of obesity corresponds to a BMI of 25 to 29.9 kg/m²?
What classification of obesity corresponds to a BMI of 25 to 29.9 kg/m²?
What is Barrett's esophagus primarily caused by?
What is Barrett's esophagus primarily caused by?
What characterizes the tissue change seen in Barrett's esophagus?
What characterizes the tissue change seen in Barrett's esophagus?
Which of the following is a treatment option for Barrett's esophagus depending on the extent of epithelial damage?
Which of the following is a treatment option for Barrett's esophagus depending on the extent of epithelial damage?
Which class of GERD medication is activated by food intake?
Which class of GERD medication is activated by food intake?
How often should patients with Barrett's esophagus be monitored by endoscopy?
How often should patients with Barrett's esophagus be monitored by endoscopy?
When is loperamide typically prescribed to be taken for managing diarrhea?
When is loperamide typically prescribed to be taken for managing diarrhea?
What should a nurse record after initiating therapy for diarrhea?
What should a nurse record after initiating therapy for diarrhea?
Which of the following characteristics of pain is crucial for the nurse to inquire about?
Which of the following characteristics of pain is crucial for the nurse to inquire about?
What should be included in the pain management interventions for patients?
What should be included in the pain management interventions for patients?
How should a nurse monitor for fluid volume deficit?
How should a nurse monitor for fluid volume deficit?
Which of the following methods can help reduce diarrhea according to the provided content?
Which of the following methods can help reduce diarrhea according to the provided content?
What role does heat application play in pain management?
What role does heat application play in pain management?
What is a priority action for the nurse in maintaining fluid intake for a patient?
What is a priority action for the nurse in maintaining fluid intake for a patient?
What characteristic feature distinguishes Crohn’s disease from ulcerative colitis?
What characteristic feature distinguishes Crohn’s disease from ulcerative colitis?
Which symptom is most commonly associated with ulcerative colitis?
Which symptom is most commonly associated with ulcerative colitis?
What is a potential complication of Crohn's disease due to deep inflammation?
What is a potential complication of Crohn's disease due to deep inflammation?
Which diagnostic method is NOT typically used for assessing Crohn's disease?
Which diagnostic method is NOT typically used for assessing Crohn's disease?
What is a common gastrointestinal symptom of Crohn’s disease?
What is a common gastrointestinal symptom of Crohn’s disease?
Which disorder is associated with ulcerative colitis?
Which disorder is associated with ulcerative colitis?
Which of the following treatments is used to manage Crohn's disease?
Which of the following treatments is used to manage Crohn's disease?
What feature of diarrhea is typically associated with ulcerative colitis?
What feature of diarrhea is typically associated with ulcerative colitis?
In which area of the abdomen is pain typically felt in individuals with ulcers due to ulcerative colitis?
In which area of the abdomen is pain typically felt in individuals with ulcers due to ulcerative colitis?
Which of the following complications is more likely to occur due to Crohn’s disease?
Which of the following complications is more likely to occur due to Crohn’s disease?
What is the primary criterion for a person to qualify for bariatric surgery?
What is the primary criterion for a person to qualify for bariatric surgery?
Which dietary practice is recommended for patients post-bariatric surgery?
Which dietary practice is recommended for patients post-bariatric surgery?
Benzphetamine primarily acts by stimulating which neurotransmitters in the brain?
Benzphetamine primarily acts by stimulating which neurotransmitters in the brain?
What mechanism does Liraglutide (semaglutide) utilize to curb appetite?
What mechanism does Liraglutide (semaglutide) utilize to curb appetite?
Which dietary substance should be avoided after bariatric surgery?
Which dietary substance should be avoided after bariatric surgery?
What type of drug is Lorcaserin classified as?
What type of drug is Lorcaserin classified as?
A body mass index (BMI) of 35 kg/m2 is sufficient for bariatric surgery if the patient has what condition?
A body mass index (BMI) of 35 kg/m2 is sufficient for bariatric surgery if the patient has what condition?
What is a common reason for complications and long-term failure after bariatric surgery?
What is a common reason for complications and long-term failure after bariatric surgery?
Study Notes
Maintaining Normal Elimination Pattern
- Administer antidiarrheal medications as prescribed.
- Loperamide can be prescribed 30 minutes before meals.
- Record the frequency and consistency of stools after therapy initiation.
Relieving Pain
- Describe the pain as dull, burning, or crampy.
- Determine if the pain occurs before or after meals, during the night, or before elimination.
- Assess if the pain is constant or intermittent and if it is relieved with medications.
- Administer analgesics as prescribed.
- Position changes, local application of heat (as prescribed), diversional activities, and prevention of fatigue can reduce pain.
Maintaining Fluid Intake
- Keep an accurate record of intake and output to detect fluid volume deficit.
- Encourage oral intake of fluids and monitor the flow rate of any IV fluids.
- Initiate measures to decrease diarrhea (e.g., dietary restrictions, stress reduction, antidiarrheal agents).
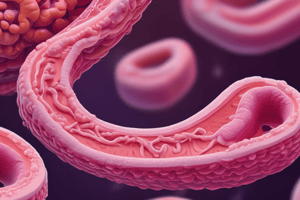
Crohn’s Disease
- Chronic inflammation involving all layers of the bowel wall.
- Occurs anywhere in the gastrointestinal (GI) tract.
- “Skip” lesions – areas of disease alternating with healthy GI tract.
- Ulcerations are deep and have a cobblestone appearance.
- Strictures at areas of inflammation may cause bowel obstruction.
- Microscopic leaks can allow bowel contents to enter the peritoneal cavity due to the inflammation going through the entire wall.
- Peritonitis or abscesses are possible and can be life-threatening.
Ulcerative Colitis
- Chronic inflammatory bowel disease (IBD) in which abnormal reactions of the immune system cause inflammation and ulcers on the inner lining of the large intestine.
- Disease of the mucosal layer of the colon and rectum, typically starting in the rectum and moving inward.
- Left lower abdominal pain and bloody diarrhea would indicate ulcerative colitis.
- Damage to mucosa, breakdown of cells, and possible formation of pseudopolyps occur.
Crohn’s Disease vs. Ulcerative Colitis: Signs and Symptoms
- Crohn's Disease: Diarrhea (unrelieved by defecation), crampy abdominal pain, especially after meals, weight loss, malnourishment, fatigue, secondary anemia, steatorrhea (excessive fat in the feces), anorexia, malnutrition, ocular disorders (uveitis), oral ulcers, skin lesions (erythema nodosum), prominent right lower quadrant abdominal pain unrelieved by defecation.
- Ulcerative Colitis: Diarrhea with marked fluid loss, stool with passage of mucus, pus, or blood, left lower quadrant abdominal pain, intermittent tenesmus (unable to relieve the urge to stool), anemia, pallor, fatigue, anorexia, weight loss, fever, vomiting, dehydration, hypoalbuminemia, electrolyte imbalance, skin lesions, eye lesions (uveitis), arthritis, liver disease.
Crohn’s Disease Diagnosis and Treatment
- Diagnosis: MRI, CT scan (to assess bowel wall thickening, mesenteric edema, obstructions, abscesses, or fistula), CBC (H&H and WBC), erythrocyte sedimentation rate (ERS) (elevated).
- Treatment: Cannot be cured. Medications like steroids and immunosuppressants are used to slow disease progression. Milk increases gastric acid secretion.
GERD Potential Complications
- Barrett’s Esophagus (Esophageal Metaplasia):
- A condition where the lining of the esophageal mucosa is altered.
- Replacement of normal squamous epithelium with columnar epithelium.
- Precancerous lesion thought to be primarily due to GERD (other causes: smoking, obesity).
- Similar symptoms to GERD: frequent pyrosis (heartburn).
- Signs and symptoms range from none to perforation.
- Perforation can be evidenced by increased temperature.
- Diagnosis: EGD & biopsy for pathology to check for alterations in epithelial lining.
- Treatment: Depends on the extent of epithelial damage: Possible ablation, surveillance, use of PPI, endoscopic resection.
- Must be monitored every 2-3 years by endoscopy.
GERD Medication Management
- Proton Pump Inhibitors (PPIs):
- “-prazole”: Esomeprazole, Lansoprazole, Omeprazole, Panteprazole, Rabeprazole.
- Proton pump is activated by food intake.
- Block the enzyme responsible for secreting hydrochloric acid (HCl) in the stomach.
- Drugs of choice for short-term therapy of peptic ulcer disease (PUD) and GERD.
- Take 20-30 minutes before the first meal of the day.
- Histamine-2 Receptor (H2R) Antagonists:
- “-tidine”: (Tagamet) Cimetidine, (Zantac) Ranitidine, (Axid) Nizatidine, (Pepcid) Famotidine.
- Histamine 2 increases acid secretion in the stomach.
- H2 antagonists suppress the volume and acidity of parietal cell secretions.
- Antacids should NOT be taken at the same time because absorption of H2 receptor blockers will be diminished.
- Once a day dose of H2 RAs should be taken at bedtime.
- Antacids:
- Maalox (magnesium hydroxide/aluminum hydrate):
- Watch for high magnesium levels (Mg++) especially in patients with cardiac or renal issues.
- Side effect: Constipation.
- TUMS (Calcium carbonate)
- Sodium bicarbonate.
- Neutralize stomach acid by raising the pH of stomach contents.
- Does NOT reduce volume.
- Acts within 10-15 minutes, duration of action is only 2 hours.
- Milk-alkali syndrome: Administering calcium carbonate antacids with milk or items with vitamin D can cause it. Early symptoms are like hypercalcemia (headache, urinary frequency, anorexia, nausea, and fatigue).
- Antacids should be taken one and three hours after meals.
- Maalox (magnesium hydroxide/aluminum hydrate):
Histamine 2 Receptor Antagonists (H2RA) and Proton Pump Inhibitors (PPI)
- Decrease gastric acid secretion.
- Sucralfate provides a barrier between mucosal erosions or ulcers and gastric secretions, and misoprostol restores prostaglandin activity.
Obesity
- Defined as abnormal or excessive fat accumulation impairing health.
- Classification: Overweight or pre-obese have a Body Mass Index (BMI) of 25 to 29.9 kg/m2.
- Causes:
- Greater access to food with poor nutritional quality.
- Lack of physical exercise.
- Low socioeconomic status.
Obesity Nursing Actions and Interventions
- Bariatric Surgery:
- Viable and popular option for treating obesity.
- Currently the only treatment found to have a successful and lasting impact on sustained weight loss for severely obese individuals.
- Criteria for Surgery:
- BMI ≥40 kg/m2.
- BMI ≥35 kg/m2 with one or more obesity-related complications (e.g., hypertension, type 2 diabetes, heart failure, sleep apnea).
- Patient Education:
- Very specific diet: Most common reason for complications and lack of long-term success.
- Small, frequent meals (≤ 1 Cup per meal).
- Low carb and glucose.
- Nutrient-dense foods (protein and fiber).
- Drinking should be 30 minutes prior or 30-60 minutes after eating.
- Avoid alcohol (ETOH) and carbonation.
- Very specific diet: Most common reason for complications and lack of long-term success.
- Medications:
- Benzphetamine (Didrex):
- Noradrenergic sympathomimetic anorexiants.
- Stimulate the release of norepinephrine and dopamine in the brain.
- Affects the nerve terminals of the hypothalamic feeding center.
- Suppresses appetite.
- Lorcaserin:
- Selective serotonergic 5-HT2C receptor agonist.
- Causes appetite suppression.
- Liraglutide (Semaglutide):
- Glucagon-like peptide-1 (GLP-1) receptor agonist.
- Mimics the effects of incretins, resulting in delayed gastric emptying, thus curbing appetite.
- Benzphetamine (Didrex):
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers essential nursing interventions for managing Crohn’s Disease, focusing on maintaining normal elimination patterns, relieving pain, and ensuring adequate fluid intake. It includes guidelines for medication administration and symptom assessment. Ideal for nursing students and healthcare professionals looking to enhance their understanding of patient care in gastrointestinal disorders.