Podcast
Questions and Answers
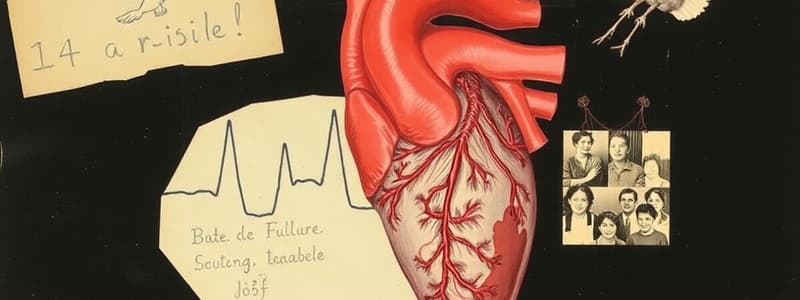
What characterizes heart failure?
What characterizes heart failure?
- Prolonged life expectancy
- Impaired cardiac pumping or filling (correct)
- Increased cardiac output
- Improved exercise tolerance
Which factor does NOT affect cardiac output?
Which factor does NOT affect cardiac output?
- Myocardial contractility
- Afterload
- Preload
- Serum cholesterol level (correct)
What is a primary risk factor for developing heart failure?
What is a primary risk factor for developing heart failure?
- Obesity
- Diabetes
- Coronary artery disease (correct)
- Tobacco use
Which type of heart failure is most common?
Which type of heart failure is most common?
Which of the following is a precipitating cause of heart failure?
Which of the following is a precipitating cause of heart failure?
What is preload in the context of cardiac function?
What is preload in the context of cardiac function?
What describes heart failure with preserved ejection fraction?
What describes heart failure with preserved ejection fraction?
Which of the following is a contributing risk factor for heart failure?
Which of the following is a contributing risk factor for heart failure?
Flashcards
What is Heart Failure?
What is Heart Failure?
A condition where the heart cannot pump enough blood to meet the body's needs. This leads to reduced blood supply to organs and tissues.
What are the main risk factors for Heart Failure?
What are the main risk factors for Heart Failure?
The primary risk factors are coronary artery disease (CAD) and hypertension (high blood pressure).
What is Preload in Heart Failure?
What is Preload in Heart Failure?
The amount of blood in the ventricles at the end of diastole (relaxation) before the next contraction.
What is Afterload in Heart Failure?
What is Afterload in Heart Failure?
Signup and view all the flashcards
What are the Primary Causes of Heart Failure?
What are the Primary Causes of Heart Failure?
Signup and view all the flashcards
What are Precipitating Causes of Heart Failure?
What are Precipitating Causes of Heart Failure?
Signup and view all the flashcards
Heart Failure with Reduced Ejection Fraction (HFrEF)
Heart Failure with Reduced Ejection Fraction (HFrEF)
Signup and view all the flashcards
Heart Failure with Preserved Ejection Fraction (HFpEF)
Heart Failure with Preserved Ejection Fraction (HFpEF)
Signup and view all the flashcards
Study Notes
Nursing 2055: Adult Illness Concepts - Heart Failure
- Heart failure (HF) is an abnormal condition causing impaired cardiac pumping, filling, or both. The heart struggles to produce sufficient cardiac output (CO) to meet metabolic needs.
- Key characteristics include ventricular dysfunction, reduced exercise tolerance, diminished quality of life, and shortened life expectancy.
Etiology and Pathophysiology
- Primary risk factors: Coronary artery disease (CAD), hypertension.
- Contributing risk factors: Diabetes, tobacco use, obesity, high serum cholesterol.
- Factors affecting cardiac output:
- Preload: Blood volume in ventricles at the end of diastole (before contraction).
- Afterload: Peripheral resistance against which the left ventricle (LV) pumps.
- Myocardial contractility: Ability of the heart muscle to contract.
- Heart rate: Number of heartbeats per minute.
- HF can be caused by any interference with the normal mechanisms regulating cardiac output.
Primary Causes of HF
- Chronic: Coronary artery disease, hypertension, rheumatic heart disease, congenital heart disease, ventricular septal defect, pulmonary disease, cardiomyopathy.
- Acute: Acute myocardial infarction, dysrhythmias, pulmonary embolus, thyrotoxicosis, hypertensive crisis, rupture of papillary muscle, myocarditis, bacterial endocarditis.
Types of Heart Failure
- Heart failure with reduced ejection fraction (HFrEF): The heart's ability to pump blood forward is diminished, indicated by an ejection fraction (EF) of 40% or less.
- Heart failure with preserved ejection fraction (HFpEF): The ventricles' ability to relax and fill during diastole is diminished, impacting stroke volume and cardiac output despite having a normal EF.
- Mixed heart failure: Combination of both HFrEF and HFpEF characteristics. Seen in conditions like dilated cardiomyopathy
Heart Failure Compensatory Mechanisms
- Sympathetic nervous system (SNS) activation: Release of catecholamines (epinephrine and norepinephrine) - First and least effective.
- Neurohormonal responses: Kidneys release renin, activating the renin-angiotensin-aldosterone system (RAAS), Decreased cerebral blood flow triggers ADH release and endothelin production.
Consequences of Compensatory Mechanisms
- Dilation: Enlargement of heart chambers in response to elevated pressure, initially adaptive, which can become inadequate and decrease cardiac output.
- Hypertrophy: Increase in heart muscle mass due to chronic dilation, leading to poor contractility, higher oxygen needs, and a higher risk of ventricular dysrhythmias.
Counterregulatory Processes
- Natriuretic peptides: Atrial natriuretic peptide (ANP) and B-type natriuretic peptide (BNP) released in response to increased atrial and ventricular pressure. Promote venous/arterial vasodilation, reducing preload and afterload. Chronic HF leads to depletion of these natriuretic peptides.
Types of Heart Failure: Left-sided HF
- Common cause is left ventricular dysfunction due to conditions like myocardial infarction (MI), hypertension, and coronary artery disease (CAD).
- Fluid backs up into the left atrium and lungs, causing pulmonary congestion.
- Key symptoms: Dyspnea, orthopnea, cough, and paroxysmal nocturnal dyspnea (PND).
Types of Heart Failure: Right-sided HF
- Often a consequence of left-sided HF, cor pulmonale, or right ventricular MI.
- Blood backs up into systemic circulation causing venous congestion.
- Key symptoms: Jugular venous distension (JVD), hepatomegaly and splenomegaly, vascular congestion of GI tract, and peripheral edema.
Heart Failure Clinical Manifestations
- Pulmonary edema: Accumulation of fluid in the alveoli and interstitial spaces of the lungs, causing shortness of breath.
- Chronic HF clinical manifestations: Progressive worsening of ventricular function and chronic neurohormonal activation, fatigue, dyspnea, orthopnea, paroxysmal nocturnal dyspnea, persistent cough, weight changes, tachycardia, edema, skin changes, and chest pain.
Complications of HF
- Pleural effusion, dysrhythmias, risk of thrombus/embolus formation (increasing risk of stroke), left ventricular thrombus, severe hepatomegaly, renal insufficiency.
Diagnostic Studies
- Primarily determine the underlying cause of HF.
- Includes history, physical examination, chest x-ray, ECG, laboratory studies (cardiac enzymes, BNP), hemodynamic assessment, echocardiogram, stress testing, cardiac catheterization, and ejection fraction measurement.
Nursing and Collaborative Management: Acute HF
- Goal 1: Decrease intravascular volume (loop diuretics, High Fowler's position, IV nitroglycerin)
- Goal 2: Improve gas exchange and oxygenation (O2, Morphine, BiPAP)
- Goal 3: Improve Cardiac function (Inotropic support, hemodynamic monitoring)
- Goal 4: Decrease afterload and Anxiety/Distress (Carefully monitor vital signs)
Nursing and Collaborative Management: Chronic HF
- Goal 1: Treat the underlying cause and contributing factors (maximize CO).
- Goal 2: Alleviate symptoms (treatment).
- Goal 3: Improve ventricular function.
- Goal 4: Improve quality of life (patient education, support).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers critical concepts related to heart failure, including its etiology, pathophysiology, and risk factors. Learn about how heart failure affects cardiac output and the implications for patient care in nursing. Utilize this knowledge to enhance your understanding of adult illness management.