Podcast
Questions and Answers
Which of the following is NOT considered a significant risk factor for Obstructive Sleep Apnea (OSA)?
Which of the following is NOT considered a significant risk factor for Obstructive Sleep Apnea (OSA)?
- Low blood pressure (correct)
- Enlarged adenoids
- A history of cigarette smoking
- Neck circumference greater than 17 inches in males
A patient reports experiencing frequent nighttime awakenings, morning headaches, and excessive daytime sleepiness. According to the information provided, these symptoms are most consistent with which condition?
A patient reports experiencing frequent nighttime awakenings, morning headaches, and excessive daytime sleepiness. According to the information provided, these symptoms are most consistent with which condition?
- Insomnia
- Restless Leg Syndrome
- Obstructive Sleep Apnea (correct)
- Narcolepsy
What is the primary mechanism behind obstructive sleep apnea (OSA)?
What is the primary mechanism behind obstructive sleep apnea (OSA)?
- A dysfunction in the brain's respiratory center.
- Excessive production of carbon dioxide in the bloodstream.
- An overproduction of mucus in the lower respiratory tract.
- A narrowing or blockage of the upper airway. (correct)
Which of the following parameters is NOT typically measured during a polysomnography (sleep study)?
Which of the following parameters is NOT typically measured during a polysomnography (sleep study)?
In the context of sleep apnea, what is the significance of an apneic episode?
In the context of sleep apnea, what is the significance of an apneic episode?
Which nonpharmacologic therapy uses different pressures for inhalation and exhalation to treat OSA?
Which nonpharmacologic therapy uses different pressures for inhalation and exhalation to treat OSA?
Uvulopalatopharyngoplasty (UPPP) involves surgical removal of which structures?
Uvulopalatopharyngoplasty (UPPP) involves surgical removal of which structures?
What diagnostic criterion is commonly used for determining the presence of sleep apnea?
What diagnostic criterion is commonly used for determining the presence of sleep apnea?
How does sleep apnea affect a person's blood pH level?
How does sleep apnea affect a person's blood pH level?
Which structures are most commonly involved in causing airway obstruction in obstructive sleep apnea (OSA)?
Which structures are most commonly involved in causing airway obstruction in obstructive sleep apnea (OSA)?
Flashcards
Obstructive Sleep Apnea (OSA)
Obstructive Sleep Apnea (OSA)
A breathing disorder where the upper airway narrows during sleep, causing partial or complete blockage, leading to disruptions in breathing.
Apnea
Apnea
A complete or near complete stoppage of breathing while sleeping for at least 10-20 seconds.
What structures can obstruct the airway during OSA?
What structures can obstruct the airway during OSA?
The soft palate, tongue, and uvula can block the airway during sleep, leading to OSA.
How does sleep apnea affect the body's pH?
How does sleep apnea affect the body's pH?
Signup and view all the flashcards
How many apnea episodes are needed for an OSA diagnosis?
How many apnea episodes are needed for an OSA diagnosis?
Signup and view all the flashcards
STOP-BANG Score
STOP-BANG Score
Signup and view all the flashcards
Polysomnography (Sleep Study)
Polysomnography (Sleep Study)
Signup and view all the flashcards
Continuous Positive Airway Pressure (CPAP)
Continuous Positive Airway Pressure (CPAP)
Signup and view all the flashcards
Uvulopalatopharyngoplasty (UPPP)
Uvulopalatopharyngoplasty (UPPP)
Signup and view all the flashcards
Study Notes
Oxygenation and Sleep-Rest Disorders: Nursing Care of the Patient with Sleep Apnea
- Course Information: NURS 1250/1610, taught by Victoria Leonetti, MSN, RN, and Emily Raddell, MSN, RN
Student Course Learning Outcomes
- Provide: Provide safe, patient-centered, evidence-based nursing care guided by the Caritas philosophy.
- Demonstrate: Demonstrate intermediate levels of critical thinking and clinical reasoning to provide quality patient care.
- Relate: Relate the impact of quality improvement measures to improved patient care.
- Explain: Explain management of care concepts for adult patients.
Pathophysiology & Etiology: Sleep Apnea (Obstructive)
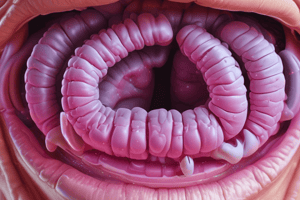
- OSA: A breathing disorder marked by a narrowing of the upper airway, obstructing airflow during sleep. This can be complete or partial.
- Obstruction Cause: Soft palate, tongue, and uvula.
- Apnea: Significant reduction or cessation of breathing during sleep.
- Frequency: Unofficially, greater than 10-20 seconds of pauses followed by loud snoring or awakening; episodes can occur hundreds of times per night.
- Diagnostic Threshold: 5 or more apneic episodes per hour is considered diagnostic.
- Disruption of Sleep: Repeated disruption of deep sleep.
- Physiological Impact: Increased blood CO2 levels, decreased blood pH (acidotic).
- Prevalence: Estimated >12 million people affected (18-25 million estimated).
Pathophysiology and Etiology: Obstructive Sleep Apnea
- Upper Airway Relaxation: Oral and upper airway soft tissues relax during sleep.
- Airflow Blockage: Relaxed tissues block the passage of air to the lungs.
- Apneic Episodes: Result in hypoxemia (low blood oxygen), particularly for the brain, triggering arousal from sleep to resume breathing.
- Sleep Return: Patient falls back into deeper sleep cycles.
Obstructed vs. Normal Airway
- Obstructed: The airway collapses during sleep, no air movement, typically a gasp/snort at the end of the apnea phase.
- Normal: The airway remains open and unobstructed during sleep.
Risk Factors
- Obesity: Men affected more than women (14% for men compared to 5% for women). Neck circumference (>17 inches in males, >16 inches in females indicate increased risk.
- Anatomy: Enlarged tongue, uvula, tonsils, adenoids, small upper airway, recessed chin.
- Genetics: Possible genetic predisposition.
- Other Factors: Diabetes, hypertension, cigarette smoking.
Clinical Manifestations
- Snoring: Loud snoring.
- Gasping/Choking: Occurrence during sleep.
- Frequent Nighttime Awakenings.
- Apnea Episodes: Five or more episodes per hour, each lasting 10-20 seconds
- Irritability: Common symptom
- Morning Headaches: Common symptom
- Daytime Drowsiness. Common symptoms.
Diagnostic Tests: STOP-BANG Score
- Snoring: Loud snoring.
- Tired: Excessive tiredness or sleepiness during the day.
- Observed: Has anyone observed you stop breathing or gasp/choke during sleep?
- Pressure: Have high blood pressure?
- Body Mass Index (BMI): More than 35 kg/m2?
- Age: Over 50 years old?
- Neck Size: Large neck size (measured around Adam's apple).
- Gender: Male.
Diagnostic Tests: Additional Procedures
- Polysomnography (Sleep Study): Measures to assess issues during sleep: air flow, blood oxygen levels, heart rate, breathing patterns, eye/leg movements, and brain waves (EEG) linked with NREM and REM stages.
Nonpharmacologic Therapy
- Weight Reduction: Significant weight loss linked to apnea improvements
- Avoid Alcohol: Avoid consumption before sleep.
- Smoking Cessation: Beneficial for respiratory health
- Side-Lying Position: Avoid supine sleep position.
- Continuous Positive Airway Pressure (CPAP): Prevents airway collapse during sleep.
- Bi-Level Positive Airway Pressure (BiPAP): Offers different pressures during exhalation and inhalation for improved ventilation.
Surgery
- Surgical options: Used if non-pharmacologic therapy is ineffective. Includes:
- Tonsillectomy/Adenoidectomy: Removing tonsils and adenoids.
- Partial soft palate/uvula removal: Portions removing soft palate/uvula.
- Uvulopalatopharyngoplasty (UPPP): Surgery to remove the uvula, soft palate, and pharyngeal tissue to open airways.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.