Podcast
Questions and Answers
What is the primary goal of initial periodontal therapy?
What is the primary goal of initial periodontal therapy?
- Achieving a plaque score of less than 5%.
- Performing periodontal surgery to eliminate deep pockets.
- Reducing inflammation and modifying patient behavior to improve oral hygiene. (correct)
- Restoring function and aesthetics with implants or orthodontics.
A patient exhibits bleeding on probing (BOP) at 15% of sites and a plaque score (PS) of 20% after initial periodontal treatment. Probing depths are consistently 3mm with no furcation involvement. Which of the following is the MOST appropriate next step in management?
A patient exhibits bleeding on probing (BOP) at 15% of sites and a plaque score (PS) of 20% after initial periodontal treatment. Probing depths are consistently 3mm with no furcation involvement. Which of the following is the MOST appropriate next step in management?
- Re-emphasize oral hygiene instructions and monitor the patient more frequently. (correct)
- Initiate corrective periodontal therapy, including periodontal surgery.
- Transition to supportive periodontal therapy with 6-month recall intervals.
- Prescribe adjunctive antimicrobials and reassess in 3 months.
Which of the following clinical findings would indicate unsuccessful periodontal treatment?
Which of the following clinical findings would indicate unsuccessful periodontal treatment?
- Lack of furcation probeability.
- Low Plaque Score (PS).
- High Bleeding On Probing (BOP). (correct)
- Probing depths of 3mm or less.
After initial periodontal therapy, a patient presents with persistent pockets of 6mm with bleeding on probing. What phase of periodontal treatment should be considered next?
After initial periodontal therapy, a patient presents with persistent pockets of 6mm with bleeding on probing. What phase of periodontal treatment should be considered next?
What is the MOST important aspect of supportive periodontal therapy?
What is the MOST important aspect of supportive periodontal therapy?
A patient has completed initial periodontal therapy. Which finding suggests the need for corrective periodontal therapy?
A patient has completed initial periodontal therapy. Which finding suggests the need for corrective periodontal therapy?
Which of the following is typically included in initial periodontal therapy?
Which of the following is typically included in initial periodontal therapy?
A patient presents with a persistent high plaque score despite good oral hygiene. What additional factor should be evaluated?
A patient presents with a persistent high plaque score despite good oral hygiene. What additional factor should be evaluated?
What is a key characteristic of corrective periodontal therapy?
What is a key characteristic of corrective periodontal therapy?
A patient undergoing periodontal treatment has probing depths reduced to 3mm or less with no bleeding on probing. What is the next appropriate phase of treatment?
A patient undergoing periodontal treatment has probing depths reduced to 3mm or less with no bleeding on probing. What is the next appropriate phase of treatment?
Which of the following operator factors is MOST likely to contribute to the failure of periodontal treatment?
Which of the following operator factors is MOST likely to contribute to the failure of periodontal treatment?
A patient presents with continued periodontal issues despite initial non-surgical periodontal therapy (NSPT). Which patient factor would be MOST important to investigate FIRST?
A patient presents with continued periodontal issues despite initial non-surgical periodontal therapy (NSPT). Which patient factor would be MOST important to investigate FIRST?
Which site-related factor presents the GREATEST challenge to successful periodontal treatment and long-term maintenance?
Which site-related factor presents the GREATEST challenge to successful periodontal treatment and long-term maintenance?
What is the MOST appropriate initial step when encountering a patient who is not responding to periodontal treatment?
What is the MOST appropriate initial step when encountering a patient who is not responding to periodontal treatment?
A patient with generalized 5mm pockets, bleeding on probing (BOP), and adequate oral hygiene is undergoing supportive periodontal therapy. Which of the following is the MOST appropriate next step?
A patient with generalized 5mm pockets, bleeding on probing (BOP), and adequate oral hygiene is undergoing supportive periodontal therapy. Which of the following is the MOST appropriate next step?
What is the PRIMARY goal of supportive periodontal therapy?
What is the PRIMARY goal of supportive periodontal therapy?
Which of the following is the MOST critical aspect of addressing non-responsive sites during periodontal maintenance?
Which of the following is the MOST critical aspect of addressing non-responsive sites during periodontal maintenance?
In a patient with controlled periodontitis undergoing supportive periodontal therapy, which pocket depth measurement would typically warrant more aggressive intervention?
In a patient with controlled periodontitis undergoing supportive periodontal therapy, which pocket depth measurement would typically warrant more aggressive intervention?
Which systemic condition is MOST likely to negatively impact a patient's response to periodontal treatment?
Which systemic condition is MOST likely to negatively impact a patient's response to periodontal treatment?
What is the overarching goal of non-surgical periodontal treatment?
What is the overarching goal of non-surgical periodontal treatment?
After initial periodontal therapy, a patient continues to exhibit bleeding on probing and inflammation in localized areas despite good oral hygiene. What is the MOST appropriate next step in managing these non-responsive sites?
After initial periodontal therapy, a patient continues to exhibit bleeding on probing and inflammation in localized areas despite good oral hygiene. What is the MOST appropriate next step in managing these non-responsive sites?
Which of the following findings would suggest the failure of non-surgical periodontal treatment?
Which of the following findings would suggest the failure of non-surgical periodontal treatment?
A patient presents with continued inflammation and bleeding despite thorough scaling and root planing. What is the MOST likely reason for the persistent inflammation?
A patient presents with continued inflammation and bleeding despite thorough scaling and root planing. What is the MOST likely reason for the persistent inflammation?
A patient has persistent periodontal inflammation around a lower molar despite repeated non-surgical interventions. Radiographic examination reveals a furcation involvement not previously noted. What is the next appropriate step?
A patient has persistent periodontal inflammation around a lower molar despite repeated non-surgical interventions. Radiographic examination reveals a furcation involvement not previously noted. What is the next appropriate step?
Which factor is MOST important to include in a supportive periodontal therapy (SPT) appointment following active non-surgical treatment?
Which factor is MOST important to include in a supportive periodontal therapy (SPT) appointment following active non-surgical treatment?
A patient with well-controlled diabetes reports fluctuating blood sugar levels during periodontal maintenance. How does this affect periodontal treatment outcomes?
A patient with well-controlled diabetes reports fluctuating blood sugar levels during periodontal maintenance. How does this affect periodontal treatment outcomes?
A patient consistently demonstrates poor plaque control despite repeated oral hygiene instructions. What psychological or sociological factor is MOST likely contributing to this?
A patient consistently demonstrates poor plaque control despite repeated oral hygiene instructions. What psychological or sociological factor is MOST likely contributing to this?
After non-surgical periodontal therapy, a patient exhibits persistent bleeding on probing at several sites, but probing depths have decreased. What is the MOST likely explanation?
After non-surgical periodontal therapy, a patient exhibits persistent bleeding on probing at several sites, but probing depths have decreased. What is the MOST likely explanation?
A patient who underwent successful non-surgical periodontal treatment now wants to know how frequently they need to have maintenance appointments? Which recall frequency range is generally recommended for patients following active periodontal treatment to prevent disease recurrence?
A patient who underwent successful non-surgical periodontal treatment now wants to know how frequently they need to have maintenance appointments? Which recall frequency range is generally recommended for patients following active periodontal treatment to prevent disease recurrence?
What is the significance of recognizing changes in a patient’s reported oral health status during supportive periodontal therapy?
What is the significance of recognizing changes in a patient’s reported oral health status during supportive periodontal therapy?
Flashcards
Primary objective of periodontal treatment
Primary objective of periodontal treatment
To slow down or halt the progression of periodontal disease and minimize tooth loss.
GDC Learning Outcome 1.1.2
GDC Learning Outcome 1.1.2
Describe oral diseases and their relevance to prevention, diagnosis and treatment
GDC Learning Outcome 1.1.11
GDC Learning Outcome 1.1.11
Recognise psychological and sociological factors that contribute to poor oral health, the course of diseases and the success of treatment
GDC Learning Outcome 1.2.2
GDC Learning Outcome 1.2.2
Signup and view all the flashcards
GDC Learning Outcome 1.2.3
GDC Learning Outcome 1.2.3
Signup and view all the flashcards
GDC Learning Outcome 1.5.3
GDC Learning Outcome 1.5.3
Signup and view all the flashcards
GDC Learning Outcome 1.7.3
GDC Learning Outcome 1.7.3
Signup and view all the flashcards
GDC Learning Outcome 1.7.8
GDC Learning Outcome 1.7.8
Signup and view all the flashcards
GDC Learning Outcome 1.10.5
GDC Learning Outcome 1.10.5
Signup and view all the flashcards
GDC Learning Outcome 1.11.1
GDC Learning Outcome 1.11.1
Signup and view all the flashcards
Ideal BOP after treatment
Ideal BOP after treatment
Signup and view all the flashcards
Ideal Plaque Score After Treatment
Ideal Plaque Score After Treatment
Signup and view all the flashcards
Ideal Pocket Depth After Treatment
Ideal Pocket Depth After Treatment
Signup and view all the flashcards
Unsuccessful Treatment: High PS
Unsuccessful Treatment: High PS
Signup and view all the flashcards
Unsuccessful Treatment: High BOP
Unsuccessful Treatment: High BOP
Signup and view all the flashcards
Unsuccessful Treatment: Pockets >5mm
Unsuccessful Treatment: Pockets >5mm
Signup and view all the flashcards
Initial Periodontal Therapy
Initial Periodontal Therapy
Signup and view all the flashcards
Corrective Periodontal Therapy
Corrective Periodontal Therapy
Signup and view all the flashcards
Supportive Periodontal Therapy
Supportive Periodontal Therapy
Signup and view all the flashcards
Key Steps in Initial Therapy
Key Steps in Initial Therapy
Signup and view all the flashcards
Operator Factors
Operator Factors
Signup and view all the flashcards
Patient Factors
Patient Factors
Signup and view all the flashcards
Site Factors
Site Factors
Signup and view all the flashcards
Poor operator technique
Poor operator technique
Signup and view all the flashcards
Patient-related obstacles
Patient-related obstacles
Signup and view all the flashcards
Site-specific complicating factors
Site-specific complicating factors
Signup and view all the flashcards
Addressing Operator Factors
Addressing Operator Factors
Signup and view all the flashcards
Managing Non-Responding Patients
Managing Non-Responding Patients
Signup and view all the flashcards
Addressing Non-Responding Sites
Addressing Non-Responding Sites
Signup and view all the flashcards
Supportive Periodontal Therapy Components
Supportive Periodontal Therapy Components
Signup and view all the flashcards
Study Notes
- Non-surgical periodontal treatment addresses the non-responding patient
GDC Learning Outcomes
- Oral diseases and their significance to prevention, diagnosis, and treatment should be described
- Psychological and sociological factors that contribute to poor oral health, disease progression, and treatment success must be recognized
- The importance of recording a comprehensive and contemporaneous patient history needs to be recognised
- Changes in a patient's reported oral health status need to be recognised, and appropriate action taken
- Delivery of care must be planned and carried out in the patient's best interests
- The need to monitor and review treatment outcomes needs to be recognised
- The need for and arrangements for appropriate follow-up care must be recognised
- Treatment results must be assessed and appropriate aftercare with ongoing preventive advice is needed
- The health of periodontal and soft tissues must be assessed and managed, taking into consideration risk and lifestyle factors
- The impact of a patient's periodontal and general health on the overall treatment plan and outcomes must be accounted for
- Non-surgical treatments should be undertaken to remove hard and soft deposits and stains using various methods
- Changes in periodontal health should monitored and recorded using appropriate indexes
- Complications associated with periodontal therapy should be recognised and appropriately managed
- The role of surgical management of periodontal diseases should be recognised, antimicrobials applied, and appropriate patient care provided
Learning Outcomes
- The aims of non-surgical periodontal treatment should be explained
- Clinical indications that treatment has been unsuccessful need to be identified
- The common reasons why treatment may fail require a list
- Possible future treatment options to address non-responding sites should be described
- The factors to be included in a supportive periodontal therapy appointment need a list
Primary Objective
- The primary objective of periodontal treatment is to slow down or halt the disease's progression and minimize tooth loss
Treatment Aims
- Bleeding on probing should be less than 10%
- Plaque Score should be less than 15%
- Periodontal Probing Depths should be less than 4mm
- No furcations should be probable
- Function needs to be maintained
- Aesthetics need to be maintained
- These aims as defined by the British Society of Periodontology
Clinical Indications of Unsuccessful Treatment
- High Plaque Score (PS)
- High Bleeding on Probing (BOP)
- Pockets greater than 5mm
- A "mixed response" can occur in a patient.
Phases of Periodontal Treatment
- Initial periodontal therapy
- Corrective periodontal therapy
- Supportive periodontal therapy
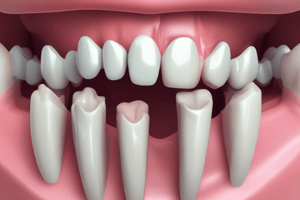
Initial Periodontal Therapy
- Plaque and bleeding indices following Basic Periodontal Examination (BPE)
- Oral Hygiene Instructions (OHI)
- Advice on smoking cessation
- Managing other risk factors
- Instrumentation/Root Surface Debridement (RSD)/removal of overhangs
- Extracting hopeless teeth, other dental work
- Monitoring response to initial therapy
- If pockets over 4mm with BOP remain, switch to corrective therapy
- If there are no pockets over 4mm or no bleeding, continue to supportive therapy
Corrective Periodontal Therapy
- Includes More Non-Surgical Periodontal Treatment (NSPT)
- +/- adjunctive antimicrobials
- Periodontal surgery may be required
- Restore function or aesthetics- definitive restorative treatment
- Implant options
- Orthodontics
Supportive Periodontal Therapy
- Supportive Periodontal Therapy embraces the philosophy that both the patient and dental professional maintain the patient's periodontal health
- It is weighted heavily towards contribution from the patient
Reasons for Treatment Failure
- Operator Factors
- Patient Factors
- Site Factors
Operator Factors
- Poor instrumentation technique
- Poor instruments
- Inexperience
- Time constraints
Patient Factors
- Poor Oral Hygiene (OH)
- Smoking
- Systemic disease/impaired host response like stress or nutrition
- Cooperation for treatment, example, Local Anaesthetic(LA) use or access
Site Factors
- Very deep pockets
- Infra-bony pockets
- Tooth and root morphology
- Failure of treatment might be due to the case's severity/complexity rather than inadequacy.
Addressing Operator Factors
- Practice is needed
- Advice from more experienced clinicians help
- Use appropriate instruments like sharp and good condition instruments.
- Time management is paramount
Addressing Non-Responding Patients
- Investigate reasons for non-response
- Address motivation, like any compounding factor, need reviewing
- Reinforce Oral Hygiene(OH)
- Review progress and treatment
Addressing Non-Responding Sites
- Corrective periodontal therapy comes into play
- Refer to specialists like periodontists
- Further Non-Surgical Periodontal Treatment (NSPT) with antimicrobials +/-
- Periodontal surgery is an option
- Extractions in some cases
- Acceptance and move to supportive periodontal therapy:
- Pockets 4-5 mm with good OH and no BOP can usually be maintained
- Pockets greater than 6mm have an increased risk of progression and tooth loss
Supportive Periodontal Therapy Appointment Factors
- Check Plaque Score (PS)
- Bleeding On Probing (BOP) check
- Motivation levels needs to be checked
- Oral Hygiene (OH) should be reinforced
- Intervention/disruption of biofilm is necessary
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.