Podcast
Questions and Answers
What percentage of cardiac output is taken by cerebral blood flow?
What percentage of cardiac output is taken by cerebral blood flow?
- 15% (correct)
- 10%
- 20%
- 25%
At what cerebral blood flow level is ischemia most likely to occur?
At what cerebral blood flow level is ischemia most likely to occur?
- 25 mL/100g
- 10 mL/100g
- 20 mL/100g (correct)
- 15 mL/100g
Which statement regarding the distribution of blood flow in the brain is true?
Which statement regarding the distribution of blood flow in the brain is true?
- Greater blood flow occurs in the subcortex compared to the cortex
- Blood flow is equal in gray and white matter
- Cortex (gray matter) receives greater blood flow than subcortex (white matter) due to higher metabolism (correct)
- Cortex and subcortex receive no blood flow
What is the consequence of an increase in the intracranial blood volume concerning the Monroe-Kellie hypothesis?
What is the consequence of an increase in the intracranial blood volume concerning the Monroe-Kellie hypothesis?
How does a decreased pH (increase in H+ ions) affect cerebral blood flow?
How does a decreased pH (increase in H+ ions) affect cerebral blood flow?
What is the Monroe-Kellie hypothesis? (select 2)
What is the Monroe-Kellie hypothesis? (select 2)
Match the critical thresholds for cerebral blood flow:
Match the critical thresholds for cerebral blood flow:
Which arterial structures primarily supply blood flow to the brain?
Which arterial structures primarily supply blood flow to the brain?
CBF = CPP/CVR
CBF = CPP/CVR
CPP= MAP-ICP or CVP
The higher the ICP, the lower the CPP if MAP is stable
CPP= MAP-ICP or CVP The higher the ICP, the lower the CPP if MAP is stable
How does Ohm's Law relate to cerebral blood flow (CBF)?
How does Ohm's Law relate to cerebral blood flow (CBF)?
How does Poiseuille's law relate to cerebral vascular resistance? (select 2)
How does Poiseuille's law relate to cerebral vascular resistance? (select 2)
Which of the following statements accurately describes Poiseuille's law?
Which of the following statements accurately describes Poiseuille's law?
Which of the following factors affect cerebral blood flow (CBF)? (Select all that apply)
Which of the following factors affect cerebral blood flow (CBF)? (Select all that apply)
Which of the following factors reduce cerebral metabolic rate of oxygen (CMRO2)? (Select all that apply)
Which of the following factors reduce cerebral metabolic rate of oxygen (CMRO2)? (Select all that apply)
What does it mean that cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2) are coupled?
What does it mean that cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2) are coupled?
How does age affect cerebral metabolic rate of oxygen (CMRO2)?
How does age affect cerebral metabolic rate of oxygen (CMRO2)?
Which of the following factors increase cerebral metabolic rate of oxygen (CMRO2)? (Select all that apply)
Which of the following factors increase cerebral metabolic rate of oxygen (CMRO2)? (Select all that apply)
What is the breakdown of oxygen utilization in the brain?
What is the breakdown of oxygen utilization in the brain?
What is the normal range for cerebral metabolic rate of oxygen (CMRO2) in adults?
What is the normal range for cerebral metabolic rate of oxygen (CMRO2) in adults?
What is the effect of altitude on cerebral blood flow (CBF)?
What is the effect of altitude on cerebral blood flow (CBF)?
What is the mechanism behind high altitude cerebral edema?
What is the mechanism behind high altitude cerebral edema?
Which physiological mechanisms contribute to compensation for increased cerebral blood flow (CBF) at high altitudes? (Select all that apply)
Which physiological mechanisms contribute to compensation for increased cerebral blood flow (CBF) at high altitudes? (Select all that apply)
At what temperature does cerebral blood flow cease due to protein denaturation and cellular death?
At what temperature does cerebral blood flow cease due to protein denaturation and cellular death?
What is cerebral autoregulation?
What is cerebral autoregulation?
Which of these factors is directly related to cerebral autoregulation? select 2
Which of these factors is directly related to cerebral autoregulation? select 2
What happens to the brain at mean arterial pressures (MAPs) above 150 mmHg?
What happens to the brain at mean arterial pressures (MAPs) above 150 mmHg?
What happens to the brain at mean arterial pressures (MAPs) below 50?
What happens to the brain at mean arterial pressures (MAPs) below 50?
What happens to the cerebral blood flow (CBF) curve with chronic hypertension?
What happens to the cerebral blood flow (CBF) curve with chronic hypertension?
What is CPP?
What is CPP?
What effect do volatile anesthetics have on cerebral blood flow?
What effect do volatile anesthetics have on cerebral blood flow?
What is the general effect of vasodilation on cerebral blood flow (CBF)?
What is the general effect of vasodilation on cerebral blood flow (CBF)?
What is the general effect of vasoconstriction on cerebral blood flow (CBF)?
What is the general effect of vasoconstriction on cerebral blood flow (CBF)?
What can cause increased cerebral blood flow (CBF) due to vasodilation? (Select all that apply)
What can cause increased cerebral blood flow (CBF) due to vasodilation? (Select all that apply)
Which agents can cause decreased cerebral blood flow (CBF) due to vasoconstriction? (Select all that apply)
Which agents can cause decreased cerebral blood flow (CBF) due to vasoconstriction? (Select all that apply)
What is the relationship between PaCO2 and cerebral blood flow (CBF)? (select 2)
What is the relationship between PaCO2 and cerebral blood flow (CBF)? (select 2)
At what range does maximal cerebral vasodilation in response to PaCO2 occur?
At what range does maximal cerebral vasodilation in response to PaCO2 occur?
At what range does maximal cerebral vasoconstriction in response to PaCO2 occur?
At what range does maximal cerebral vasoconstriction in response to PaCO2 occur?
What mechanism directly controls cerebral vascular resistance?
What mechanism directly controls cerebral vascular resistance?
Why does metabolic acidosis not directly affect cerebral blood flow (CBF)?
Why does metabolic acidosis not directly affect cerebral blood flow (CBF)?
Which scenario exemplifies the classic steal phenomenon?
Which scenario exemplifies the classic steal phenomenon?
What is the clinical implication of using hyperventilation to cause vasoconstriction and inverse steal? (select 2)
What is the clinical implication of using hyperventilation to cause vasoconstriction and inverse steal? (select 2)
What is the goal range for permissive hypocapnia?
What is the goal range for permissive hypocapnia?
What is the relationship between paO2 and cerebral blood flow (CBF)?
What is the relationship between paO2 and cerebral blood flow (CBF)?
Why does a PaO2 level of less than 50mmHg of brain tissue result in immediate vasodilation?
Why does a PaO2 level of less than 50mmHg of brain tissue result in immediate vasodilation?
What is the difference between hypoxia and hypoxemia?
What is the difference between hypoxia and hypoxemia?
What is considered a normal cerebral perfusion pressure (CPP)?
What is considered a normal cerebral perfusion pressure (CPP)?
CPP = MAP-ICP or CVP
Higher CVP with a normal MAP will reduce CPP
CPP = MAP-ICP or CVP Higher CVP with a normal MAP will reduce CPP
Match the cerebral perfusion pressure (CPP) values with their corresponding clinical results:
Match the cerebral perfusion pressure (CPP) values with their corresponding clinical results:
How does an increased pH (a decrease in H+) affect cerebral blood flow (CBF)?
How does an increased pH (a decrease in H+) affect cerebral blood flow (CBF)?
What is the Circle of Willis?
What is the Circle of Willis?
What is considered normal intracranial pressure (ICP)?
What is considered normal intracranial pressure (ICP)?
What is defined as intracranial hypertension (HTN)?
What is defined as intracranial hypertension (HTN)?
What is Cushing's triad?
What is Cushing's triad?
What causes hypertension in response to increased intracranial pressure (ICP)?
What causes hypertension in response to increased intracranial pressure (ICP)?
Why does bradycardia occur in increased intracranial pressure (ICP)?
Why does bradycardia occur in increased intracranial pressure (ICP)?
Why do irregular respirations occur during increased intracranial pressure (ICP)?
Why do irregular respirations occur during increased intracranial pressure (ICP)?
What are immediate ways to reduce intracranial pressure (ICP)? (Select all that apply)
What are immediate ways to reduce intracranial pressure (ICP)? (Select all that apply)
What methods can be used to reduce intracranial pressure (ICP)?
What methods can be used to reduce intracranial pressure (ICP)?
What is the mechanism of action of mannitol?
What is the mechanism of action of mannitol?
How does Positive End-Expiratory Pressure (PEEP) affect cerebral blood flow (CBF)?
How does Positive End-Expiratory Pressure (PEEP) affect cerebral blood flow (CBF)?
How does mannitol affect cerebral autoregulation to reduce intracranial pressure (ICP)?
How does mannitol affect cerebral autoregulation to reduce intracranial pressure (ICP)?
What are the complications associated with mannitol use? (Select all that apply)
What are the complications associated with mannitol use? (Select all that apply)
How does hypertonic saline reduce intracranial pressure (ICP) more effectively than mannitol?
How does hypertonic saline reduce intracranial pressure (ICP) more effectively than mannitol?
What are complications associated with hypertonic saline treatment for increased intracranial pressure (ICP)? (Select all that apply)
What are complications associated with hypertonic saline treatment for increased intracranial pressure (ICP)? (Select all that apply)
What effect does hypertonic saline have on glutamate release?
What effect does hypertonic saline have on glutamate release?
What is the relationship between intracranial compliance and intracranial elastance?
What is the relationship between intracranial compliance and intracranial elastance?
What is a consequence of high elastance?
What is a consequence of high elastance?
Which of the following factors can increase intracranial volume? (Select all that apply)
Which of the following factors can increase intracranial volume? (Select all that apply)
What causes vasogenic brain edema?
What causes vasogenic brain edema?
What is the blood-brain barrier?
What is the blood-brain barrier?
In which of the following structures is the blood-brain barrier (BBB) absent? (Select all that apply)
In which of the following structures is the blood-brain barrier (BBB) absent? (Select all that apply)
What can cause the blood-brain barrier (BBB) to become dysfunctional? (Select all that apply)
What can cause the blood-brain barrier (BBB) to become dysfunctional? (Select all that apply)
What is unique about the blood-brain barrier (BBB) in neonates?
What is unique about the blood-brain barrier (BBB) in neonates?
Match the agent with its permeability to the blood-brain barrier (BBB):
Match the agent with its permeability to the blood-brain barrier (BBB):
What is a space occupying lesion?
What is a space occupying lesion?
Where is a supratentorial tumor located?
Where is a supratentorial tumor located?
Where is an infratentorial tumor located?
Where is an infratentorial tumor located?
Which types of cancers commonly spread to the brain when they metastasize? (Select all that apply)
Which types of cancers commonly spread to the brain when they metastasize? (Select all that apply)
What state is considered the beginning of loss of consciousness?
What state is considered the beginning of loss of consciousness?
What state indicates the deepest level of consciousness that is still responsive to stimulus?
What state indicates the deepest level of consciousness that is still responsive to stimulus?
What type of breathing indicates a rapidly deteriorating condition due to a medullary lesion?
What type of breathing indicates a rapidly deteriorating condition due to a medullary lesion?
What is decerebrate posturing? (select 2)
What is decerebrate posturing? (select 2)
What is decorticate posturing? (select 2)
What is decorticate posturing? (select 2)
What does posturing indicate?
What does posturing indicate?
What does the progression from decorticate to decerebrate posturing indicate in terms of brain herniation? (select 2)
What does the progression from decorticate to decerebrate posturing indicate in terms of brain herniation? (select 2)
Which cranial nerves does the oculocephalic reflex assess? (Choose all that apply)
Which cranial nerves does the oculocephalic reflex assess? (Choose all that apply)
What is the alternate name for the oculocephalic reflex?
What is the alternate name for the oculocephalic reflex?
What is a normal response to the oculocephalic reflex test?
What is a normal response to the oculocephalic reflex test?
Which cranial nerves are assessed by the oculovestibular reflex?
Which cranial nerves are assessed by the oculovestibular reflex?
Calorics test eye movement to injection of water
COWS = cold opposite, warm same
Calorics test eye movement to injection of water COWS = cold opposite, warm same
Which cranial nerves are used to test the corneal reflex?
Which cranial nerves are used to test the corneal reflex?
Which cranial nerves are involved in the gag reflex?
Which cranial nerves are involved in the gag reflex?
By what mechanism do volatile anesthetics uncouple cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2)? (select 2)
By what mechanism do volatile anesthetics uncouple cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2)? (select 2)
What occurs to cerebral blood flow (CBF) at a minimum alveolar concentration (MAC) of 0.5?
What occurs to cerebral blood flow (CBF) at a minimum alveolar concentration (MAC) of 0.5?
What is the effect of 1.5 MAC on cerebral blood flow (CBF)?
What is the effect of 1.5 MAC on cerebral blood flow (CBF)?
What is an immediate way to balance a reduction in cerebral blood flow (CBF) caused by volatile agents?
What is an immediate way to balance a reduction in cerebral blood flow (CBF) caused by volatile agents?
At what MAC level do the effects of vasodilation balance with cerebral metabolic rate of oxygen consumption (CMRO2)?
At what MAC level do the effects of vasodilation balance with cerebral metabolic rate of oxygen consumption (CMRO2)?
How should you manage volatile agent delivery for patients with increased intracranial pressure (ICP)?
How should you manage volatile agent delivery for patients with increased intracranial pressure (ICP)?
What is a known negative side effect of enflurane?
What is a known negative side effect of enflurane?
What effect do induction agents have on cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2)?
What effect do induction agents have on cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2)?
Which of the following agents are used as anticonvulsants? (Select all that apply)
Which of the following agents are used as anticonvulsants? (Select all that apply)
Which induction agent is unique for its cerebral vasodilatory properties?
Which induction agent is unique for its cerebral vasodilatory properties?
Which anesthetic agent is noted to decrease cerebral blood flow (CBF) without changes in intracranial pressure (ICP) or cerebral metabolic rate of oxygen (CMRO2)?
Which anesthetic agent is noted to decrease cerebral blood flow (CBF) without changes in intracranial pressure (ICP) or cerebral metabolic rate of oxygen (CMRO2)?
Which anesthetic agent is noted for its increased concentration and effect with longer infusions?
Which anesthetic agent is noted for its increased concentration and effect with longer infusions?
What effects do opioids have on cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2)?
What effects do opioids have on cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2)?
How do opioids alter intracranial pressure (ICP) through hypercarbia?
How do opioids alter intracranial pressure (ICP) through hypercarbia?
What is unique about the response of large muscles to non-depolarizing neuromuscular blockade?
What is unique about the response of large muscles to non-depolarizing neuromuscular blockade?
Which induction agent causes the least reduction in cerebral metabolic rate of oxygen (CMRO2) and cerebral blood flow (CBF)?
Which induction agent causes the least reduction in cerebral metabolic rate of oxygen (CMRO2) and cerebral blood flow (CBF)?
What is unique about quaternary amide anticholinergic agents such as glycopyrrolate?
What is unique about quaternary amide anticholinergic agents such as glycopyrrolate?
What is the effect of hyperthermia on the brain? (Select all that apply)
What is the effect of hyperthermia on the brain? (Select all that apply)
What is the endothelial mechanism of cerebral autoregulation? (select 2)
What is the endothelial mechanism of cerebral autoregulation? (select 2)
What is the primary way in which cerebral autoregulation is maintained?
What is the primary way in which cerebral autoregulation is maintained?
Which channel primarily regulates membrane potential?
Which channel primarily regulates membrane potential?
What are the results of K+ channel inhibition? (select 2)
What are the results of K+ channel inhibition? (select 2)
What is the result of hyperpolarization on cerebral blood flow (CBF)? (select 2)
What is the result of hyperpolarization on cerebral blood flow (CBF)? (select 2)
Which of the following would cause vasoconstriction and therefore decreased cerebral blood flow (CBF)?
Which of the following would cause vasoconstriction and therefore decreased cerebral blood flow (CBF)?
What is the effect of hyperbaric oxygen therapy on cerebral blood flow (CBF)?
What is the effect of hyperbaric oxygen therapy on cerebral blood flow (CBF)?
Which arteries are part of the anterior circle of Willis? (Select all that apply)
Which arteries are part of the anterior circle of Willis? (Select all that apply)
What effect does nitrous oxide have on CMRO2 and ICP?
What effect does nitrous oxide have on CMRO2 and ICP?
Why do certain induction agents cause cerebral vasoconstriction?
Why do certain induction agents cause cerebral vasoconstriction?
At what level does MAC amnesia occur?
At what level does MAC amnesia occur?
Which of the following factors increase intracranial compliance? (Select all that apply)
Which of the following factors increase intracranial compliance? (Select all that apply)
Which of the following factors decreases intracranial compliance? (Select all that apply)
Which of the following factors decreases intracranial compliance? (Select all that apply)
How do astrocytes affect cerebral blood flow (CBF)?
How do astrocytes affect cerebral blood flow (CBF)?
What causes cytotoxic brain edema?
What causes cytotoxic brain edema?
Which type of neoplasm is noted for its rapid growth?
Which type of neoplasm is noted for its rapid growth?
Flashcards are hidden until you start studying
Study Notes
Monroe-Kellie Hypothesis
- The sum of brain, CSF, and intracranial blood volumes remains constant.
- An increase in one volume requires a decrease in one or both of the others.
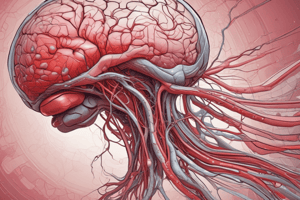
Cerebral Blood Flow (CBF)
- Normal range is 50mL/100g of brain tissue.
- Greater blood flow in the cortex (gray matter) compared to the subcortex (white matter).
- CBF represents 15% of the body's cardiac output.
- It is influenced by blood supply, perfusion, and cerebral vascular resistance.
CBF Critical Thresholds
- Ischemia occurs at 20mL/100g of brain tissue per minute.
- Cortical suppression occurs at approximately 15mL/100g per minute.
- Cell death can result from prolonged CBF below critical thresholds.
Cerebral Blood Flow
- The volume of the brain, cerebrospinal fluid (CSF), and intracranial blood is constant. If one volume increases, one or both of the other volumes must decrease.
- Cerebral blood flow (CBF) is typically 50mL/100g of brain tissue.
- The cortex (grey matter) receives more blood flow than the subcortex (white matter).
- CBF receives 15% of the total cardiac output.
- Factors influencing CBF include blood supply, perfusion, and cerebral vascular resistance.
- Ischemia (restriction of blood flow) occurs at CBF of 20mL/100g.
- CBF of approximately 15mL/100g leads to cortical suppression.
- Cell death occurs when CBF falls below a certain threshold.
Steal Phenomena
- Cerebral vessels supplying ischemic areas are already maximally dilated.
- Situations causing cerebral vasodilation, such as hypercapnia, can divert blood flow from ischemic areas to healthy areas, worsening ischemia.
- Inverse steal is the concept that situations causing cerebral vasoconstriction, such as hypocapnia, can redirect blood flow from healthy areas to ischemic areas, potentially improving perfusion in the ischemic region.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.