Podcast
Questions and Answers
Which nerve fibers innervate skeletal muscle fibers?
Which nerve fibers innervate skeletal muscle fibers?
- Gamma-myelinated nerve fibers
- Delta-myelinated nerve fibers
- Alpha-myelinated nerve fibers (correct)
- Beta-myelinated nerve fibers
What happens to the axon as it approaches the muscle?
What happens to the axon as it approaches the muscle?
- It narrows and becomes less defined
- It branches into axon terminals (correct)
- It thickens and myelinates further
- It transforms into a sensory receptor
What is another name for the axon terminals that innervate muscle fibers?
What is another name for the axon terminals that innervate muscle fibers?
- End Feet (correct)
- Terminal Plates
- Gamma Buttons
- Motor Strip
Which structure covers the tips of each axon branch at the neuromuscular junction?
Which structure covers the tips of each axon branch at the neuromuscular junction?
What is characteristic of the continuity between the nerve and muscle at the neuromuscular junction?
What is characteristic of the continuity between the nerve and muscle at the neuromuscular junction?
What happens to the axon at the point where it establishes contact with the muscle fiber?
What happens to the axon at the point where it establishes contact with the muscle fiber?
What is the neurilemma continuous with at the neuromuscular junction?
What is the neurilemma continuous with at the neuromuscular junction?
What is the motor end plate?
What is the motor end plate?
What are the invaginations of the muscle membrane under the sole feet called?
What are the invaginations of the muscle membrane under the sole feet called?
What is the space between the sole feet and the muscle fiber membrane called?
What is the space between the sole feet and the muscle fiber membrane called?
What is the main purpose of the subneural clefts?
What is the main purpose of the subneural clefts?
Which of the following is contained within the sole foot?
Which of the following is contained within the sole foot?
What anchors acetylcholine vesicles to the cytoskeleton in the presynaptic terminal?
What anchors acetylcholine vesicles to the cytoskeleton in the presynaptic terminal?
What is found on the inside surface of the neural membrane, adjacent to voltage-gated calcium channels?
What is found on the inside surface of the neural membrane, adjacent to voltage-gated calcium channels?
What is the role of cholinesterase at the border of the synaptic gutter?
What is the role of cholinesterase at the border of the synaptic gutter?
Approximately what percentage of released acetylcholine is hydrolyzed before reaching the receptors?
Approximately what percentage of released acetylcholine is hydrolyzed before reaching the receptors?
What happens to choline after acetylcholine is hydrolyzed?
What happens to choline after acetylcholine is hydrolyzed?
What is the amplitude of the subthreshold depolarization in muscle fibers during rest, known as the miniature end plate potential (MEPP)?
What is the amplitude of the subthreshold depolarization in muscle fibers during rest, known as the miniature end plate potential (MEPP)?
What causes a miniature end plate potential (MEPP)?
What causes a miniature end plate potential (MEPP)?
Which of the following ions is directly responsible for triggering the release of acetylcholine at the presynaptic terminal?
Which of the following ions is directly responsible for triggering the release of acetylcholine at the presynaptic terminal?
What is the first step in the mechanism of neuromuscular transmission?
What is the first step in the mechanism of neuromuscular transmission?
How many vesicles of acetylcholine are typically released from the nerve terminals into the synaptic space?
How many vesicles of acetylcholine are typically released from the nerve terminals into the synaptic space?
What type of acetylcholine receptors are located in the muscle membrane at the neuromuscular junction?
What type of acetylcholine receptors are located in the muscle membrane at the neuromuscular junction?
Which ion has a greater diffusion across the muscle membrane during the development of the end plate potential (EPP)?
Which ion has a greater diffusion across the muscle membrane during the development of the end plate potential (EPP)?
What happens to acetylcholine after it detaches from its receptors?
What happens to acetylcholine after it detaches from its receptors?
What defines the end plate potential (EPP)?
What defines the end plate potential (EPP)?
How does the end plate potential (EPP) lead to muscle contraction?
How does the end plate potential (EPP) lead to muscle contraction?
What happens to neuromuscular transmission if magnesium ion concentration overwhelms calcium ion concentration?
What happens to neuromuscular transmission if magnesium ion concentration overwhelms calcium ion concentration?
Which of the following drugs stimulates neuromuscular transmission by resisting hydrolysis by cholinesterase?
Which of the following drugs stimulates neuromuscular transmission by resisting hydrolysis by cholinesterase?
How does curare affect neuromuscular transmission?
How does curare affect neuromuscular transmission?
What is the primary mechanism by which botulinum toxin inhibits neuromuscular transmission?
What is the primary mechanism by which botulinum toxin inhibits neuromuscular transmission?
How does Hemicholinium affect neuromuscular transmission?
How does Hemicholinium affect neuromuscular transmission?
What is a primary characteristic of Myasthenia Gravis?
What is a primary characteristic of Myasthenia Gravis?
What is the cause of Myasthenia Gravis?
What is the cause of Myasthenia Gravis?
Why is eserine typically avoided in the management of myasthenia gravis?
Why is eserine typically avoided in the management of myasthenia gravis?
How does Lambert-Eaton syndrome primarily disrupt neuromuscular transmission?
How does Lambert-Eaton syndrome primarily disrupt neuromuscular transmission?
What effect does the administration of prostagmine have on neuromuscular transmission?
What effect does the administration of prostagmine have on neuromuscular transmission?
If a patient is treated with atropine following possible exposure to Eserine, which of the following best describes the rationale for this treatment strategy?
If a patient is treated with atropine following possible exposure to Eserine, which of the following best describes the rationale for this treatment strategy?
A researcher discovers a new drug that selectively enhances the activity of synapsin in motor neurons. What effect would this drug likely have on neuromuscular transmission?
A researcher discovers a new drug that selectively enhances the activity of synapsin in motor neurons. What effect would this drug likely have on neuromuscular transmission?
Flashcards
Neuromuscular Junction
Neuromuscular Junction
The point of contact between a nerve fibre and the muscle it innervates.
Alpha Motor Neurons
Alpha Motor Neurons
Large, myelinated nerve fibers that innervate skeletal muscle fibers.
Axon Terminals
Axon Terminals
Expanded endings of motor neuron axons that form the neuromuscular junction.
Neurolemma
Neurolemma
Signup and view all the flashcards
Neuromuscular Junction
Neuromuscular Junction
Signup and view all the flashcards
Sarcolemma
Sarcolemma
Signup and view all the flashcards
Motor End Plate
Motor End Plate
Signup and view all the flashcards
Synaptic Gutters
Synaptic Gutters
Signup and view all the flashcards
Synaptic Cleft
Synaptic Cleft
Signup and view all the flashcards
Subneural Clefts
Subneural Clefts
Signup and view all the flashcards
Synaptic Vesicles
Synaptic Vesicles
Signup and view all the flashcards
Acetylcholine (ACh)
Acetylcholine (ACh)
Signup and view all the flashcards
Synapsin
Synapsin
Signup and view all the flashcards
Voltage-Gated Calcium Channels
Voltage-Gated Calcium Channels
Signup and view all the flashcards
Cholinesterase
Cholinesterase
Signup and view all the flashcards
Miniature End Plate Potential (MEPP)
Miniature End Plate Potential (MEPP)
Signup and view all the flashcards
End Plate Potential (EPP)
End Plate Potential (EPP)
Signup and view all the flashcards
Unidirectional Transmission
Unidirectional Transmission
Signup and view all the flashcards
Synaptic Delay
Synaptic Delay
Signup and view all the flashcards
Synaptic Fatigue
Synaptic Fatigue
Signup and view all the flashcards
Acetylcholine-Like Drugs
Acetylcholine-Like Drugs
Signup and view all the flashcards
Curare
Curare
Signup and view all the flashcards
Botulinum Toxin
Botulinum Toxin
Signup and view all the flashcards
Hemicholinium
Hemicholinium
Signup and view all the flashcards
Myasthenia Gravis
Myasthenia Gravis
Signup and view all the flashcards
Study Notes
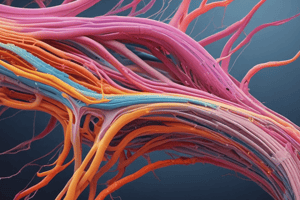
- Skeletal muscle fibers are innervated by large α-myelinated nerve fibres
α-motor neuron branches
- As the α-motor neuron branches, it approaches the muscle
- The motor neuron ends in expanded endings called axon terminals, otherwise known as end feet or terminal buttons
- The tips of each branch (sole feet) are covered by the neurolemma
Neuromuscular Junction
- Neuromuscular junction is the area of contact between the nerve fiber and the muscle fiber
- There is no cytoplasmic continuity between the nerve and the muscle
- The axon loses its myelin sheath
- Each skeletal muscle fiber receives only one axon terminal
- Each nerve ending makes a junction, called neuromuscular junction
Motor End Plate
- At the neuromuscular junction, the neurilemma becomes continuous with the sarcolemma
- The muscle membrane is thickened and is called motor end plate
- The muscle membrane under the sole feet is invaginated to enclose them, called the synaptic gutter
Synaptic Cleft
- The space between the sole feet and the muscle fiber membrane is called the synaptic cleft, otherwise known as synaptic space, and is 25 nM wide.
- At the bottom of the gutter are numerous smaller folds of the muscle membrane called subneural clefts, increasing surface area where the synaptic transmitter can act.
Acetylcholine
- The sole foot contains many vesicles filled with acetylcholine (Ach); the chemical transmitter and many mitochondria which is necessary for its synthesis.
- Proteins called synapsin anchor the Ach vesicles to the cytoskeleton of the presynaptic terminal
Dense Bars
- On the inside surface of the neural membrane are linear dense bars
- Voltage-gated calcium channels are to each side of each dense bar
Cholinesterase
- At the border of the gutter, there is a large quantities of the enzyme cholinesterase, which hydrolyzes Ach
- It destroys Ach a few msec after it has been released from the synaptic vesicles
- The short time that the Ach remains in the synaptic space is sufficient to excite the muscle fiber
- About 60% of the released Ach is hydrolyzed before reaching the Ach receptors
- The remaining 40% is hydrolyzed after activating the channels
- Choline is taken up again by the nerve ending to form new Ach, and acetate escapes to the blood stream
- Rapid removal of Ach prevents continued muscle re-excitation
Miniature End Plate Potential (M.E.P.P.)
- M.E.P.P. is a state of persistent localized subthreshold DP (0.5 mV in amplitude) of the muscle fibres at the M.E.P. during rest
- It does not reach the firing level, so it does not lead to an AP
- The cause of this is due to the continuous release of small amounts of Ach (due to continuous rupture of a few vesicles that contain this chemical transmitter at the nerve terminals).
Mechanism of Neuromuscular Transmission
- Action potential propagates down a motor neuron
- Voltage-gated Ca++ channels open in terminal buttons
- Subsequently causing a Ca++ influx
- Synapsin proteins are phosphorylated, which anchor the Ach vesicles to the cytoskeleton of the presynaptic terminal
- Ach vesicles are freed from the cytoskeleton and are allowed to move to the active zone of the presynaptic neural membrane adjacent to the dense bars.
- The vesicles dock at the release sites, fuse with the neural membrane, and empty their Ach into synaptic space via exocytosis.
- About 125 vesicles of Ach are released from the terminals into the synaptic space.
- Acetylcholine diffuses across the cleft
- Binds to specific nicotinic Ach receptors in the muscle membrane
- Na+ and K+ channels open, these are ligand-gated
- More Na+ than K+ diffuses (more Na+ ions flow than K+ ions)
- Development of end plate potential and the formation of end plate potential result.
- When EPP reaches the firing level, an AP is generated
- Ach then detaches from receptors
- Ach then diffuses into the folds of MEP
- Ach is then rapidly hydrolyzed by cholinesterase, which prevents re-excitation of the muscle
- This process is the termination of Ach action
End Plate Potential (E.P.P.)
- A state of nonpropagated transient DP of the postjunctional membrane of the motor end plate
- Follows the arrival of an impulse to the motor nerve ending
- It is a state of partial DP
- When EPP reaches the firing level, an AP is generated
Properties of Neuromuscular Transmission
- Transmission of impulse is Unidirectional; they are allowed to pass from the nerve to the muscle.
- Transmission of impulses at the MEP is delayed by 0.5 mS
- This time is needed for:
- Release of the Ach.
- Its diffusion through the synaptic cleft and combination with the its receptors. -Na + influx till the firing level is reached
- It is easily fatigued by repeated stimulation mostly due to exhaustion of Ach.
- There is also an effect by ions:
- Excess Ca++ causes increased release of Ach and increase transmission due to rupture of Ach vesicles.
- Excess Mg++ causes decreased release of Ach and decreased transmission due to block rupture of vesicles.
Drugs That Stimulate Neuromuscular Transmission
- Act by Acetylcholine-Like Action: these are not rapidly hydrolyzed by cholinesterase enzyme, for e.g. methacholine and carbachol.
- Inactivating Acetylcholinesterase: these drugs preserve the liberated Ach at the MEP, for e.g. neostigmine, physostigmine (eserine).
Drugs That Block Neuromuscular Transmission
- Curare (tubocurarine) and some other related drugs (e.g. Flaxedil) block the action of Ach by occupying its receptors at MEP (competitive inhibition).
- These drugs are used as muscle relaxants during surgical operations
- Botulinum toxin inhibits the release of Ach
- Clostridium botulinum is specific bacteria that cause potent botulinum toxins
- These act by preventing the release of neurotransmitters in the CNS and at the neuromuscular junction which causes flaccid paralysis.
- Botulism can result from ingestion of contaminated food or wound infection.
- Hemicholinium blocks the reuptake of choline into nerve terminals, thereby depleting stores of Ach.
Conditions and Drugs that Affect Neuromuscular Transmission
- Acetylcholine-Like Action: methacholine and carbachol stimulate Neuromuscular Transmission
- Curare blocks nicotinic receptors at MEΡ, hindering the binding of acetylcholine to receptors
- Myasthenia gravis destroys Ach receptors
- Affect Acetylcholinesterase: Eserine and prostagmine (a drug) inhibit acetylcholinesterase
Myasthenia Gravis
- Hereditary disease that affects females more than males
- Characterized by marked progressive weakness and easy fatigability of muscles
Myasthenia Gravis Cause
- Due to the formation of autoantibodies (autoimmune) that cause the destruction of Ach receptors at the MEP, the response to Ach is reduced
- treated by drugs which inhibit cholinestrase e.g. prostagmine thereby preserving Ach which leads to better neuromuscular transmission and prolongs the action of ACh at the ΜΕΡ
- Eserine is NOT used in the treatment because, besides muscle contraction, it produces dangerous parasympathetic effects like hypotension due to V.D. and bradycardia.
- excessive salivation, defecation and micturition
Drug interactions
- The antagonist of eserine is atropine
- The antagonist of atropine is either Ach or eserine
Lambert-Eaton syndrome
- Neuromuscular disease that has symptoms of progressive muscle weakness and fatigue
- Caused by circulating antibodies to presynaptic Ca2+ channels, prevents nerve terminals preventing DP and release of Ach.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.