Podcast
Questions and Answers
What is the primary function of the frontal lobe?
What is the primary function of the frontal lobe?
- Primarily responsible for vision
- Processing sound, auditory language, and speech comprehension
- Cognitive function, control of voluntary movement (correct)
- Processing information about temperature, taste, touch and movement
Which cranial nerve is responsible for vision?
Which cranial nerve is responsible for vision?
- CN IV - Trochlear
- CN III - Oculomotor
- CN I - Olfactory
- CN II - Optic (correct)
What is the purpose of the Romberg test?
What is the purpose of the Romberg test?
- To assess the patient's ability to understand and follow instructions
- To assess the patient's ability to perceive pain and temperature
- To test the patient's ability to maintain balance with their eyes open
- To evaluate proprioception and cerebellar function (correct)
Which cranial nerve is responsible for the gag reflex?
Which cranial nerve is responsible for the gag reflex?
Which of the following is NOT a function of the cerebellum?
Which of the following is NOT a function of the cerebellum?
Which cranial nerve is responsible for lateral eye movement?
Which cranial nerve is responsible for lateral eye movement?
What is the function of the occipital lobe?
What is the function of the occipital lobe?
Which cranial nerve is responsible for the sense of smell?
Which cranial nerve is responsible for the sense of smell?
What is the most common triggering event associated with Bell’s Palsy?
What is the most common triggering event associated with Bell’s Palsy?
Which of the following statements is true regarding the facial paralysis seen in Bell’s Palsy?
Which of the following statements is true regarding the facial paralysis seen in Bell’s Palsy?
What is the recommended management strategy for patients with Bell’s Palsy?
What is the recommended management strategy for patients with Bell’s Palsy?
Which laboratory test is NOT typically ordered for diagnosing Bell’s Palsy?
Which laboratory test is NOT typically ordered for diagnosing Bell’s Palsy?
Which of the following is a common symptom preceding the onset of facial paralysis in Bell’s Palsy?
Which of the following is a common symptom preceding the onset of facial paralysis in Bell’s Palsy?
What symptom is commonly associated with unilateral headaches?
What symptom is commonly associated with unilateral headaches?
Which of the following is a common trigger for cluster headaches?
Which of the following is a common trigger for cluster headaches?
What is an effective initial management option for an acute migraine attack?
What is an effective initial management option for an acute migraine attack?
Which of the following diagnostic tools is indicated for evaluating cluster headaches?
Which of the following diagnostic tools is indicated for evaluating cluster headaches?
What factor can lower seizure threshold?
What factor can lower seizure threshold?
Which medication is not effective for generalized seizures?
Which medication is not effective for generalized seizures?
What is a characteristic symptom of cluster headaches?
What is a characteristic symptom of cluster headaches?
What is a notable effect of Sinemet after 2 to 5 years of treatment?
What is a notable effect of Sinemet after 2 to 5 years of treatment?
Which medication should be taken at night due to the risk of orthostatic hypotension?
Which medication should be taken at night due to the risk of orthostatic hypotension?
What is a common non-pharmacological treatment for migraines?
What is a common non-pharmacological treatment for migraines?
Which treatment option for Parkinson's disease involves lesions of nuclei that inhibit basal ganglia?
Which treatment option for Parkinson's disease involves lesions of nuclei that inhibit basal ganglia?
Which type of scan can detect low levels of dopamine in the brain indicative of Parkinson's disease?
Which type of scan can detect low levels of dopamine in the brain indicative of Parkinson's disease?
Which of the following is incorrectly advised to a patient diagnosed with migraines?
Which of the following is incorrectly advised to a patient diagnosed with migraines?
Bell's palsy is characterized by symptoms except which of the following?
Bell's palsy is characterized by symptoms except which of the following?
What is a primary indication for using anticholinergics in young patients?
What is a primary indication for using anticholinergics in young patients?
Which of the following statements about MRI or CAT scans in Parkinson's disease is true?
Which of the following statements about MRI or CAT scans in Parkinson's disease is true?
What is a symptom that is NOT associated with Bell’s Palsy?
What is a symptom that is NOT associated with Bell’s Palsy?
What is most characteristic of a partial seizure?
What is most characteristic of a partial seizure?
What best describes the condition of a child showing paralysis on the left side after a seizure?
What best describes the condition of a child showing paralysis on the left side after a seizure?
Which type of seizure is characterized by fluttering eyes and lip smacking in a child?
Which type of seizure is characterized by fluttering eyes and lip smacking in a child?
What is a potential consequence for a child with frequent seizures as noted on an EEG?
What is a potential consequence for a child with frequent seizures as noted on an EEG?
In the case of a child experiencing status epilepticus, which medication should the nurse prepare for administration?
In the case of a child experiencing status epilepticus, which medication should the nurse prepare for administration?
Which action should NOT be included in the care of a child during status epilepticus?
Which action should NOT be included in the care of a child during status epilepticus?
Secondary headaches can arise due to which of the following situations?
Secondary headaches can arise due to which of the following situations?
What is the most common subtype of Parkinson's Disease?
What is the most common subtype of Parkinson's Disease?
How much dopamine loss is typically required before Parkinson's Disease symptoms are noticeable?
How much dopamine loss is typically required before Parkinson's Disease symptoms are noticeable?
What is a common early sign of Parkinson’s Disease that involves muscular rigidity?
What is a common early sign of Parkinson’s Disease that involves muscular rigidity?
Which demographic group is 1½ times more likely to be affected by Parkinson's Disease?
Which demographic group is 1½ times more likely to be affected by Parkinson's Disease?
What is the primary mechanism of action of Selegiline (Eldepryl) in the treatment of Parkinson's Disease?
What is the primary mechanism of action of Selegiline (Eldepryl) in the treatment of Parkinson's Disease?
What does the 'pill rolling' tremor in Parkinson's Disease refer to?
What does the 'pill rolling' tremor in Parkinson's Disease refer to?
Which condition or symptom may appear in advanced stages of Parkinson's Disease?
Which condition or symptom may appear in advanced stages of Parkinson's Disease?
What would be the Gold Standard for diagnosing Parkinson's Disease?
What would be the Gold Standard for diagnosing Parkinson's Disease?
Which cranial nerve is responsible for shrugging your shoulders?
Which cranial nerve is responsible for shrugging your shoulders?
Which of the following are associated with classic migraines?
Which of the following are associated with classic migraines?
What is the most common type of headache?
What is the most common type of headache?
What is a common trigger for migraine headaches?
What is a common trigger for migraine headaches?
Which of the following is NOT a symptom of tension headaches?
Which of the following is NOT a symptom of tension headaches?
Which over-the-counter medication is commonly used to manage tension headaches?
Which over-the-counter medication is commonly used to manage tension headaches?
What does the mnemonic "Oh Oh Oh To Touch And Feel A Girl’s Vagina So Happy" refer to?
What does the mnemonic "Oh Oh Oh To Touch And Feel A Girl’s Vagina So Happy" refer to?
Which of the following is a characteristic symptom of migraine headaches?
Which of the following is a characteristic symptom of migraine headaches?
Which of the following tests is used to evaluate proprioception and cerebellar function?
Which of the following tests is used to evaluate proprioception and cerebellar function?
Which cranial nerve is responsible for hearing and equilibrium?
Which cranial nerve is responsible for hearing and equilibrium?
What is the primary function of the temporal lobe?
What is the primary function of the temporal lobe?
What is the typical timeframe for maximum paralysis to occur in Bell's Palsy?
What is the typical timeframe for maximum paralysis to occur in Bell's Palsy?
Which of the following is NOT a typical symptom associated with Bell's Palsy?
Which of the following is NOT a typical symptom associated with Bell's Palsy?
What is a characteristic symptom of cluster headaches, often present in affected patients?
What is a characteristic symptom of cluster headaches, often present in affected patients?
What is the correct sequence of steps for the heel to shin test?
What is the correct sequence of steps for the heel to shin test?
Which of the following medications would be most appropriate for acute management of a migraine attack with severe nausea and vomiting?
Which of the following medications would be most appropriate for acute management of a migraine attack with severe nausea and vomiting?
In the context of seizure management, which of the following medications is typically used to treat focal seizures but not generalized seizures?
In the context of seizure management, which of the following medications is typically used to treat focal seizures but not generalized seizures?
Which cranial nerve is responsible for both motor and sensory function?
Which cranial nerve is responsible for both motor and sensory function?
What is the single most important management goal for patients with Bell's Palsy?
What is the single most important management goal for patients with Bell's Palsy?
What is a common factor that can lower a person's seizure threshold, making them more prone to seizures?
What is a common factor that can lower a person's seizure threshold, making them more prone to seizures?
Which of the following statements accurately describes the function of the frontal lobe?
Which of the following statements accurately describes the function of the frontal lobe?
A patient reports experiencing a sudden, intense, unilateral headache that feels like an 'ice pick' being jabbed into their head. They mention these episodes occur almost daily for a few weeks, followed by months or weeks of relief. This pattern is most consistent with:
A patient reports experiencing a sudden, intense, unilateral headache that feels like an 'ice pick' being jabbed into their head. They mention these episodes occur almost daily for a few weeks, followed by months or weeks of relief. This pattern is most consistent with:
Which cranial nerve is involved in the gag reflex?
Which cranial nerve is involved in the gag reflex?
What diagnostic tool is typically employed to rule out underlying structural abnormalities, such as AVM or aneurysms, in patients experiencing frequent cluster headaches?
What diagnostic tool is typically employed to rule out underlying structural abnormalities, such as AVM or aneurysms, in patients experiencing frequent cluster headaches?
What daily medication is commonly prescribed for cluster headache prophylaxis, aiming to prevent the recurrence of these excruciating headaches?
What daily medication is commonly prescribed for cluster headache prophylaxis, aiming to prevent the recurrence of these excruciating headaches?
Which of the following is a common management strategy for a patient experiencing an acute cluster headache?
Which of the following is a common management strategy for a patient experiencing an acute cluster headache?
What is the recommended treatment for a patient with a high-risk TIA (ABCD score ≥ 4)?
What is the recommended treatment for a patient with a high-risk TIA (ABCD score ≥ 4)?
Which of the following investigations is most suitable for detecting ischemic infarcts?
Which of the following investigations is most suitable for detecting ischemic infarcts?
Which of the following medications is NOT recommended as a treatment for hypertension in patients with TIA?
Which of the following medications is NOT recommended as a treatment for hypertension in patients with TIA?
A patient with an ABCD score of 2 would fall into which risk category?
A patient with an ABCD score of 2 would fall into which risk category?
Which of the following is a cardinal feature of Parkinson's Disease?
Which of the following is a cardinal feature of Parkinson's Disease?
Which of the following is NOT a recommended management strategy for patients with Parkinson's Disease?
Which of the following is NOT a recommended management strategy for patients with Parkinson's Disease?
What is the significance of a high ESR and CRP in a patient with suspected TIA?
What is the significance of a high ESR and CRP in a patient with suspected TIA?
Which of the following is a potential risk factor for developing TIA?
Which of the following is a potential risk factor for developing TIA?
Based on the cerebrospinal fluid results, which of the following is indicative of bacterial meningitis?
Based on the cerebrospinal fluid results, which of the following is indicative of bacterial meningitis?
The nurse practitioner is evaluating a child with a concussion who is still experiencing sleepiness 2 weeks after the injury. What is the MOST appropriate recommendation for this child?
The nurse practitioner is evaluating a child with a concussion who is still experiencing sleepiness 2 weeks after the injury. What is the MOST appropriate recommendation for this child?
Which of the following actions should the nurse take after receiving results indicating bacterial meningitis from a cerebrospinal fluid test?
Which of the following actions should the nurse take after receiving results indicating bacterial meningitis from a cerebrospinal fluid test?
What is the primary reason for the elevated protein count in the cerebrospinal fluid of a patient with bacterial meningitis?
What is the primary reason for the elevated protein count in the cerebrospinal fluid of a patient with bacterial meningitis?
Which of the following statements accurately describes the role of the nurse in caring for a child with suspected meningitis?
Which of the following statements accurately describes the role of the nurse in caring for a child with suspected meningitis?
Cerebellar function is responsible for
Cerebellar function is responsible for
All tests can evaluate cerebellar function except
All tests can evaluate cerebellar function except
The NP will test which CN by having the patient sniff a familiar scent and blocking one nostril at a time?
The NP will test which CN by having the patient sniff a familiar scent and blocking one nostril at a time?
The NP will test which CN for visual field testing by having the patient stand 2 feet in front of the examiner and covering one eye at a time, test peripheral vision, and stand 20 feet from Snellen chart?
The NP will test which CN for visual field testing by having the patient stand 2 feet in front of the examiner and covering one eye at a time, test peripheral vision, and stand 20 feet from Snellen chart?
The NP will test which CN for EOM and pupillary reaction?
The NP will test which CN for EOM and pupillary reaction?
Which CN get tested together for sight and EOM?
Which CN get tested together for sight and EOM?
The NP will test which CN to look for downward and inward eye movement?
The NP will test which CN to look for downward and inward eye movement?
The NP will test which CN to asses mastication, sensation scalp/face/cornea/nose (lightly brushes face with whisp)
The NP will test which CN to asses mastication, sensation scalp/face/cornea/nose (lightly brushes face with whisp)
The NP will test which CN to asses for lateral eye movement?
The NP will test which CN to asses for lateral eye movement?
The NP will test which CN to see if they can move the face, close mouth, and generate tear & saliva secretion?
The NP will test which CN to see if they can move the face, close mouth, and generate tear & saliva secretion?
The NP will test which CN for hearing and equilibrium by whispering words and asking if they can hear the words?
The NP will test which CN for hearing and equilibrium by whispering words and asking if they can hear the words?
The NP will test which CN for 1/3 phonation, gag reflex, swallowing, taste (posterior) and have them say Ah?
The NP will test which CN for 1/3 phonation, gag reflex, swallowing, taste (posterior) and have them say Ah?
The NP will test which CN for talking, swallowing, and carotid reflex ?
The NP will test which CN for talking, swallowing, and carotid reflex ?
The NP will test which CN for shrugging shoulders and head rotation?
The NP will test which CN for shrugging shoulders and head rotation?
The NP will test which CN for tongue movement by telling them to stick out their tongue and move it side to side?
The NP will test which CN for tongue movement by telling them to stick out their tongue and move it side to side?
Flashcards
Cerebral Function
Cerebral Function
Involves higher brain functions like touch, vision, hearing, speech, reasoning, and emotions.
Frontal Lobe
Frontal Lobe
Responsible for cognitive function and voluntary movement control.
Parietal Lobe
Parietal Lobe
Processes sensory information related to temperature, taste, touch, and movement.
Occipital Lobe
Occipital Lobe
Signup and view all the flashcards
Temporal Lobe
Temporal Lobe
Signup and view all the flashcards
Cerebellar Function
Cerebellar Function
Signup and view all the flashcards
Romberg Test
Romberg Test
Signup and view all the flashcards
Cranial Nerves
Cranial Nerves
Signup and view all the flashcards
Bell's Palsy
Bell's Palsy
Signup and view all the flashcards
Cranial Nerve VII
Cranial Nerve VII
Signup and view all the flashcards
Symptoms of Bell's Palsy
Symptoms of Bell's Palsy
Signup and view all the flashcards
Diagnosis of Bell's Palsy
Diagnosis of Bell's Palsy
Signup and view all the flashcards
Management of Bell's Palsy
Management of Bell's Palsy
Signup and view all the flashcards
Migraine Symptoms
Migraine Symptoms
Signup and view all the flashcards
Migraine Diagnostics
Migraine Diagnostics
Signup and view all the flashcards
Acute Migraine Management
Acute Migraine Management
Signup and view all the flashcards
Cluster Headaches
Cluster Headaches
Signup and view all the flashcards
Cluster Headache Symptoms
Cluster Headache Symptoms
Signup and view all the flashcards
Seizure Definition
Seizure Definition
Signup and view all the flashcards
Seizure Causes
Seizure Causes
Signup and view all the flashcards
Focal Seizures
Focal Seizures
Signup and view all the flashcards
Sinemet
Sinemet
Signup and view all the flashcards
Dopamine agonists
Dopamine agonists
Signup and view all the flashcards
Anticholinergics
Anticholinergics
Signup and view all the flashcards
Deep Brain Stimulation
Deep Brain Stimulation
Signup and view all the flashcards
MRI/CAT scans
MRI/CAT scans
Signup and view all the flashcards
PET scan
PET scan
Signup and view all the flashcards
Migraine triggers
Migraine triggers
Signup and view all the flashcards
Bell’s palsy
Bell’s palsy
Signup and view all the flashcards
Parkinson’s Disease (PD)
Parkinson’s Disease (PD)
Signup and view all the flashcards
Primary Parkinson’s Disease
Primary Parkinson’s Disease
Signup and view all the flashcards
Secondary Parkinsonism
Secondary Parkinsonism
Signup and view all the flashcards
Familial Parkinson’s Disease
Familial Parkinson’s Disease
Signup and view all the flashcards
Dopamine Loss Threshold
Dopamine Loss Threshold
Signup and view all the flashcards
Symptoms of PD
Symptoms of PD
Signup and view all the flashcards
Bradykinesia
Bradykinesia
Signup and view all the flashcards
Levodopa Therapy
Levodopa Therapy
Signup and view all the flashcards
Postictal paralysis
Postictal paralysis
Signup and view all the flashcards
Absence seizure
Absence seizure
Signup and view all the flashcards
EEG
EEG
Signup and view all the flashcards
Status epilepticus
Status epilepticus
Signup and view all the flashcards
Secondary headaches
Secondary headaches
Signup and view all the flashcards
Kernig's sign
Kernig's sign
Signup and view all the flashcards
Brudzinski's sign
Brudzinski's sign
Signup and view all the flashcards
Diagnostics for Bell's Palsy
Diagnostics for Bell's Palsy
Signup and view all the flashcards
Tension Headaches
Tension Headaches
Signup and view all the flashcards
Migraine Headaches
Migraine Headaches
Signup and view all the flashcards
Classic Migraine
Classic Migraine
Signup and view all the flashcards
Common Migraine
Common Migraine
Signup and view all the flashcards
Cerebellum
Cerebellum
Signup and view all the flashcards
Finger to Nose Test (FNT)
Finger to Nose Test (FNT)
Signup and view all the flashcards
Heel to Shin Test
Heel to Shin Test
Signup and view all the flashcards
Cranial Nerve I (Olfactory)
Cranial Nerve I (Olfactory)
Signup and view all the flashcards
Cranial Nerve II (Optic)
Cranial Nerve II (Optic)
Signup and view all the flashcards
Cranial Nerve VII (Facial)
Cranial Nerve VII (Facial)
Signup and view all the flashcards
Cranial Nerve IX (Glossopharyngeal)
Cranial Nerve IX (Glossopharyngeal)
Signup and view all the flashcards
Proprioception
Proprioception
Signup and view all the flashcards
Bacterial Meningitis Indicators
Bacterial Meningitis Indicators
Signup and view all the flashcards
Concussion Management
Concussion Management
Signup and view all the flashcards
Neurological Assessment Steps
Neurological Assessment Steps
Signup and view all the flashcards
Lumbar Puncture Preparation
Lumbar Puncture Preparation
Signup and view all the flashcards
Post-Concussion Symptoms
Post-Concussion Symptoms
Signup and view all the flashcards
Cluster Headache Characteristics
Cluster Headache Characteristics
Signup and view all the flashcards
Sumatriptan (Imitrex) Uses
Sumatriptan (Imitrex) Uses
Signup and view all the flashcards
Prophylactic Treatment for Migraines
Prophylactic Treatment for Migraines
Signup and view all the flashcards
MRI vs CT in Stroke Diagnosis
MRI vs CT in Stroke Diagnosis
Signup and view all the flashcards
ABCD Score
ABCD Score
Signup and view all the flashcards
Management of High-Risk TIA
Management of High-Risk TIA
Signup and view all the flashcards
Carotid Endarterectomy
Carotid Endarterectomy
Signup and view all the flashcards
Stroke Risk at ABCD Scores
Stroke Risk at ABCD Scores
Signup and view all the flashcards
Low-Risk TIA Management
Low-Risk TIA Management
Signup and view all the flashcards
Cardinal Features of Parkinson's Disease
Cardinal Features of Parkinson's Disease
Signup and view all the flashcards
Dopamine Loss in PD
Dopamine Loss in PD
Signup and view all the flashcards
Study Notes
Adult Neurological Disorders
- Adult Neurological Disorders is the subject.
- The presenter is Dr. Kim Ballone, FNP-BC.
- The presentation is a review of many neurological disorders.
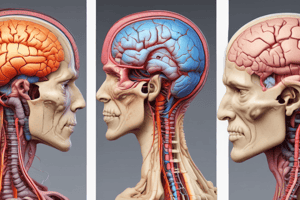
Cerebral Function
- The cerebrum performs higher functions like interpreting touch, vision, hearing, speech, reasoning, emotions, learning, and fine motor control.
- The brain has four lobes:
- Frontal lobe: controls voluntary movement and cognitive function.
- Parietal lobe: processes information about temperature, taste, touch, and movement.
- Occipital lobe: primarily responsible for vision.
- Temporal lobe: processes sound, auditory language, and speech comprehension.
Cerebellar Function
- The cerebellum is responsible for balance and coordination.
- Assessment techniques to evaluate cerebellar function:
- Romberg Test: assesses proprioception and cerebellar function by having the patient stand with feet together, eyes closed, and arms at their sides.
- Finger to nose test: evaluates the patient's ability to correctly touch their finger to their nose, assessing visual-motor coordination and proprioception.
- Heel to shin test: evaluates the patient's ability to run the heel of one foot along the shin of the opposite leg, assessing proprioception and coordination.
Review of 12 Cranial Nerves
- Cranial nerves are numbered from I to XII.
- Each nerve has a specific function and can be either sensory, motor, or both. See the list below.
| Cranial Nerve | Function | Type |
|---|---|---|
| CNI (Olfactory) | Smell | Sensory |
| CNII (Optic) | Vision | Sensory |
| CNIII (Oculomotor) | Eye movement (EOMs) and pupillary reaction | Motor |
| CNIV (Trochlear) | Down and in eye movement | Motor |
| CNV (Trigeminal) | Mastication, sensation of scalp, face, cornea, nose | Both |
| CNVI (Abducens) | Lateral eye movement | Motor |
| CNVII (Facial) | Facial movements, tears, saliva secretion | Both |
| CNVIII (Acoustic) | Hearing and equilibrium | Sensory |
| CNIX (Glossopharyngeal) | Taste (posterior), phonation, gag, swallowing; Say Ah | Both |
| CNX (Vagus) | Talking, swallowing, carotid reflex | Both |
| CNXI (Spinal Accessory) | Shrug the shoulders | Motor |
| CNXII (Hypoglossal) | Moves the tongue | Motor |
- CN III, IV, and VI test extraocular movements together.
Review of Headaches
- Tension headaches are the most common type of headache (90%).
- Signs and symptoms of tension headaches include a vise-like or band-like pain around the neck and back of the head, stiffness in the shoulders, and usually lasting several hours.
- Triggering factors include emotional/physical stress, head and neck movements.
- Management includes over-the-counter analgesics (Naproxen, Ibuprofen, Aspirin, Tylenol), combinations, and relaxation techniques.
Headaches (Migraines)
- Migraines are related to dilation and excessive pulsation of the external carotid artery branches.
- They can last from 2 to 72 hours.
- Migraines can have an aura (classic) or no aura (common).
- Common triggers include stress, missed meals, changes in weather, certain foods (nitrates, aspartame), sleep disturbance, alcohol, and menstruation.
- Diagnosis includes a clinical evaluation, symptom assessment (unilateral, throbbing pain, visual disturbances, nausea, vomiting).
- Management of acute attacks includes rest in a dark room and simple analgesics (aspirin, etc.), antiemetics (if needed), or triptans (severe cases).
- Prophylactic therapy is useful for frequent migraines.
Cluster Headaches
- Cluster headaches are very painful, abrupt, and unilateral.
- Pain is typically periorbital, but it can occur daily for several weeks.
- Triggers include alcohol consumption, tobacco use, or head trauma and are more common in men.
- Signs include nasal congestion, tearing, and redness in the affected eye (Horner's syndrome).
- Diagnosis is done via MRI for vascular abnormalities.
- Management includes triptans, 100% oxygen, ergotamine, and preventives (e.g., verapamil).
Review of Seizures
-
A seizure is a transient disturbance of brain function due to abnormal paroxysmal neuronal discharge.
-
Causes include congenital or perinatal injuries, metabolic disorders, trauma, tumors, infectious diseases, and fever.
-
Different seizure types include partial and generalized, and specific classifications can further describe the manifestation:
- Partial Seizures - Focal origin, usually unilateral
- Simple Partial - Retained awareness, motor, sensory, or autonomic symptoms
- Complex Partial Seizures - Impaired awareness
- Generalized Seizures - Both hemispheres involved
- Tonic-Clonic or Grand Mal - Loss of consciousness, bilateral jerking, and coma
- Tonic - Sudden muscle stiffening
- Clonic - Rhythmic jerking
- Absence (Petit Mal) - Brief staring episodes, common in children
-
Diagnosis techniques include CBC, electrolytes, testing for infectious agents, and EEG.
Management of Seizures
- Management actions involve maintaining airway, protecting from injury, oxygen if cyanotic, anticonvulsant medication (e.g., Lorazepam, Keppra, etc.).
- Broad-spectrum anticonvulsants are used for both focal and generalized seizures (e.g., Keppra).
Bell's Palsy
- Bell's Palsy is an acute, unilateral facial nerve palsy.
- It is of unknown etiology possibly triggered by nerve ischemia or a viral infection.
- This type of palsy can occur within 24 hours, often preceded by pain behind the ear of affected side.
- Cranial nerve VII is involved.
- Diagnosis is based on clinical presentation (unilateral facial paralysis, inability to close eye, forehead movement, etc).
- It is commonly diagnosed as HSV.
- Management involves protection of the eye/cornea (artificial tears), eye exercises, massage of affected area, antivirals (Valacyclovir or acyclovir), glucocorticoids.
- It is more common in women of all ages.
Trigeminal Neuralgia
- Trigeminal neuralgia is a nerve disorder causing unilateral pain in the maxillary or mandibular branches.
- Triggering factors can include stimulation like chewing, brushing, hot/cold food, or touch.
- It is characterized by sudden, severe, stabbing pain in the face.
- Treatment involves medications that suppress nerve activity and may include tricyclic antidepressants.
- Diagnosis includes an assessment of neurological function and imaging (MRI) to rule out tumors.
Multiple Sclerosis (MS)
- MS is a chronic autoimmune disease affecting the central nervous system.
- The immune system attacks the myelin sheath surrounding neurons.
- Initial and often early symptoms include numbness, trouble with coordination and balance, problems with vision, speech, and bladder control; episodes may subside and return as exacerbations and remissions.
- Management includes immunomodulatory therapy (IMT) to reduce relapses, including interferons, immunosuppressants, and plasmapheresis.
Myasthenia Gravis
- Myasthenia gravis is a neuromuscular junction disorder. It causes muscle weakness and fatigability.
- The disorder results from a reduction in the number of acetylcholine receptors.
- This commonly affects women in their 30s/40s and 50s/60s and can affect any age.
- Testing techniques include antibodies to acetylcholine receptors, and/or Edrophonium.
- Management involves anticholinesterase drugs (pyridostigmine), immunosuppressives, and possibly plasmapheresis.
Acute Cerebral Vascular Syndrome (ACVS)/Transient Ischemic Attack (TIA)
- A Transient Ischemic Attack (TIA) is a temporary disruption of blood supply to the brain.
- Symptoms and Signs are sudden changes in vision, speech, strength/movement (numbness), or sensation.
- Risk factors include older age, hypertension; Diabetes, history of TIA.
- Diagnosis often involves a CT scan or MRI to rule out bleeding or tumor, followed by a carotid ultrasound to evaluate the blood vessels, and a blood test.
- The goal is to address the underlying cause of the TIA.
Parkinson's Disease
- Parkinson's disease is a slowly progressive neurodegenerative disorder.
- The cardinal signs include tremor, rigidity, and bradykinesia, commonly with postural changes.
- The disease develops from a depletion of dopamine in the substantia nigra.
- The disorder may be primary (idiopathic), secondary, or familial. (genetic).
Tips to Remember
- For suspected cerebral vascular accidents, immediate ED referral is required.
Other Information
- The ABCD score is used to evaluate acute cerebral vascular syndrome (TIA).
- Specific foods (high in tyramine) can trigger migraines.
- Avoiding high potassium foods is not related to migraines.
- Swallowing is not directly affected by Bell's palsy.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.