Podcast
Questions and Answers
What percentage of the global burden of disease is constituted by neurologic disorders?
What percentage of the global burden of disease is constituted by neurologic disorders?
- 12% (correct)
- 20%
- 14%
- 5%
Which of the following is NOT included in the health history assessment for neurological disorders?
Which of the following is NOT included in the health history assessment for neurological disorders?
- Medications
- Family history
- Blood pressure readings (correct)
- Allergies
What is one of the components assessed during a neurologic examination?
What is one of the components assessed during a neurologic examination?
- Nutritional status
- Gait, stance, and coordination (correct)
- Respiratory rate
- Visual acuity
What is the maximum score obtainable on the Glasgow Coma Scale?
What is the maximum score obtainable on the Glasgow Coma Scale?
Which aspect of the Glasgow Coma Scale assesses the best motor response?
Which aspect of the Glasgow Coma Scale assesses the best motor response?
What type of symptoms might indicate a disturbance in the gastrointestinal system in neurological disorders?
What type of symptoms might indicate a disturbance in the gastrointestinal system in neurological disorders?
Which of the following symptoms is associated with disturbances in the nervous system?
Which of the following symptoms is associated with disturbances in the nervous system?
What component of the Glasgow Coma Scale represents a score of 6?
What component of the Glasgow Coma Scale represents a score of 6?
What major complaint should the nurse anticipate in a patient post-surgery?
What major complaint should the nurse anticipate in a patient post-surgery?
Which action should NOT be taken if a patient develops a sore throat post-operation?
Which action should NOT be taken if a patient develops a sore throat post-operation?
What should the postoperative patient be monitored for regarding physical condition?
What should the postoperative patient be monitored for regarding physical condition?
After surgery, how long should the patient remain flat in bed?
After surgery, how long should the patient remain flat in bed?
Which of the following is an appropriate intervention for a patient who has undergone cervical surgery?
Which of the following is an appropriate intervention for a patient who has undergone cervical surgery?
What position should be avoided while the patient is sleeping post-surgery?
What position should be avoided while the patient is sleeping post-surgery?
What should the patient do if they experience increased pain postoperatively?
What should the patient do if they experience increased pain postoperatively?
What type of diet may be recommended for a patient complaining of dysphagia post-operation?
What type of diet may be recommended for a patient complaining of dysphagia post-operation?
What is the significance of a GCS score between 3 and 8?
What is the significance of a GCS score between 3 and 8?
Which imaging technique involves injecting a contrast medium to visualize cerebral circulation?
Which imaging technique involves injecting a contrast medium to visualize cerebral circulation?
What is the purpose of a PET scan combined with a CT scan?
What is the purpose of a PET scan combined with a CT scan?
What type of anesthesia is typically used for a lumbar puncture?
What type of anesthesia is typically used for a lumbar puncture?
What is a common finding in normal cerebrospinal fluid (CSF) analysis?
What is a common finding in normal cerebrospinal fluid (CSF) analysis?
Which condition could contraindicate a lumbar puncture?
Which condition could contraindicate a lumbar puncture?
What does an Electroencephalogram (EEG) record?
What does an Electroencephalogram (EEG) record?
Which type of disc herniation is the rarest?
Which type of disc herniation is the rarest?
Which of the following symptoms is NOT commonly associated with cervical issues?
Which of the following symptoms is NOT commonly associated with cervical issues?
What imaging technique is commonly used to evaluate spine disorders?
What imaging technique is commonly used to evaluate spine disorders?
Which of the following indicates a preparation for surgical intervention?
Which of the following indicates a preparation for surgical intervention?
What is the primary focus of discharge planning for a patient with lumbar spine issues?
What is the primary focus of discharge planning for a patient with lumbar spine issues?
What is a common non-surgical treatment method for muscle spasm control?
What is a common non-surgical treatment method for muscle spasm control?
What condition may result in chronic back and leg pain after spinal surgery?
What condition may result in chronic back and leg pain after spinal surgery?
In which scenario is a laminectomy most indicated?
In which scenario is a laminectomy most indicated?
Which practice should be avoided to prevent exacerbating cervical spine issues?
Which practice should be avoided to prevent exacerbating cervical spine issues?
Flashcards
Impact of Neurological Disorders
Impact of Neurological Disorders
Neurological disorders are common and impactful. They affect over 1 billion people worldwide, causing 12% of the global disease burden and 14% of global deaths.
Health History in Neurological Assessment
Health History in Neurological Assessment
The process of gathering information about a patient's medical history and symptoms to understand their neurological condition.
Chief Complaint and Onset
Chief Complaint and Onset
Information about the patient's main concern, when it started, specific symptoms, factors that cause it to worsen or improve, and any potential risk factors.
Mental Status Assessment
Mental Status Assessment
Signup and view all the flashcards
Neurologic Examination
Neurologic Examination
Signup and view all the flashcards
Cranial Nerve Examination
Cranial Nerve Examination
Signup and view all the flashcards
Motor System Evaluation
Motor System Evaluation
Signup and view all the flashcards
Sensation Assessment
Sensation Assessment
Signup and view all the flashcards
Glasgow Coma Scale (GCS)
Glasgow Coma Scale (GCS)
Signup and view all the flashcards
Cerebral Angiography
Cerebral Angiography
Signup and view all the flashcards
Lumbar Puncture (Spinal Tap)
Lumbar Puncture (Spinal Tap)
Signup and view all the flashcards
Myelography
Myelography
Signup and view all the flashcards
Positron Emission Tomography (PET) Scan
Positron Emission Tomography (PET) Scan
Signup and view all the flashcards
Disc Herniation
Disc Herniation
Signup and view all the flashcards
Electroencephalogram (EEG)
Electroencephalogram (EEG)
Signup and view all the flashcards
Cervical Spondylosis Symptoms
Cervical Spondylosis Symptoms
Signup and view all the flashcards
Lumbar Spondylosis Symptoms
Lumbar Spondylosis Symptoms
Signup and view all the flashcards
Laminectomy
Laminectomy
Signup and view all the flashcards
Myelogram
Myelogram
Signup and view all the flashcards
Computerized Tomography (CT Scan)
Computerized Tomography (CT Scan)
Signup and view all the flashcards
Electromyography (EMG)
Electromyography (EMG)
Signup and view all the flashcards
Failed Disc Syndrome
Failed Disc Syndrome
Signup and view all the flashcards
Arachnoiditis
Arachnoiditis
Signup and view all the flashcards
What is a laminectomy?
What is a laminectomy?
Signup and view all the flashcards
Why is bed rest essential after a laminectomy?
Why is bed rest essential after a laminectomy?
Signup and view all the flashcards
How is pain managed after a laminectomy?
How is pain managed after a laminectomy?
Signup and view all the flashcards
After a laminectomy, how should the patient change directions?
After a laminectomy, how should the patient change directions?
Signup and view all the flashcards
How long is the cervical collar worn after a laminectomy?
How long is the cervical collar worn after a laminectomy?
Signup and view all the flashcards
What specific movements should be avoided after a laminectomy?
What specific movements should be avoided after a laminectomy?
Signup and view all the flashcards
What sleeping position should be avoided after a laminectomy?
What sleeping position should be avoided after a laminectomy?
Signup and view all the flashcards
What signs should the patient monitor after a laminectomy?
What signs should the patient monitor after a laminectomy?
Signup and view all the flashcards
Study Notes
Neurological Disorders and Intervertebral Disk Prolapse
- Neurological diseases are common and costly, affecting over 1 billion people worldwide, accounting for 12% of the global disease burden and 14% of global deaths.
Introduction
- Neurologic diseases are common and costly.
- Neurological disorders affect over 1 billion people worldwide.
- They constitute 12% of the global burden of disease.
- They cause 14% of global deaths.
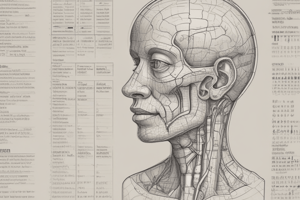
Neurological Assessment
-
Health History: Includes details about the patient's chief complaint, onset, signs and symptoms, predisposing factors, aggravating and relieving factors, medications, alcohol and recreational drug use, and any history of head or spinal cord trauma or falls. Also, allergies, habits/lifestyle changes, and family history are important factors.
-
General Signs/Symptoms: The assessment covers the nervous system, including disturbances in consciousness, memory loss, headaches, pain, dizziness, vertigo, and seizures. The musculoskeletal system assessment includes weakness, loss of coordination, tremors, numbness, and paralysis. Additional systems to consider include gastrointestinal and other systems (e.g., nausea/vomiting; bowel or bladder difficulties; swallowing difficulties; visual disturbance; speech difficulties).
Physical Examination
- Neurological Examination: The examination comprises mental status, cranial nerves, motor system assessment (muscle strength, gait, stance, coordination, sensation), reflexes, and the autonomic nervous system.
Assessment Tools
- Glasgow Coma Scale (GCS): Used to assess level of consciousness. It has three categories: Eye opening, Best motor response, and Best verbal response. The scores range from 3 to 15. A GCS between 3 and 8 indicates a severe head injury.
Diagnostic Testing
-
Positron Emission Tomography (PET) Scans: Assess blood flow, tissue composition, and brain function.
-
Cerebral Angiography: Uses contrast medium to visualize cerebral circulation and detect aneurysms or tumors, often accessing the femoral artery.
-
Lumbar Puncture (Spinal Tap): Involves inserting a needle into the subarachnoid space between the third and fifth lumbar vertebrae; useful for measuring cerebrospinal fluid (CSF) fluid or pressure or injecting a medication or contrast medium. Contraindicated with increased intracranial pressure.
-
Myelography: An X-ray of the spinal subarachnoid space after injecting a contrast agent; used to visualize the vertebral column and intervertebral disks.
-
Electroencephalogram (EEG): Measures electrical activity in the brain; used to diagnose and evaluate seizures, identify tumors or brain abscesses/infections, and confirm brain death.
Laboratory Testing
- Cerebrospinal Fluid (CSF) Analyses: Analyzing CSF can reveal normal findings, such as a pH of 7.35-7.45, specific gravity of 1.007, and a clear, colorless, odorless appearance. Additionally, minimal WBCs and no RBCs along with positive protein and glucose are normal findings.
Nursing Management for Patients with Cervical Disc Prolapse
- Immobilization: Immobilize/rest the cervical spine using methods like a cervical collar, cervical traction, and bed rest.
- Muscle Spasm Control: Administer muscle relaxants to control muscle spasm.
- Surgical Intervention: Prepare for surgical intervention if necessary, due to significant neurological deficit from nerve root compression.
- Discharge planning: Teach patients to avoid extreme flexion, extension and rotation of the cervical spine during activity, keep the head in a neutral position while sleeping, avoid excessive automobile riding while experiencing acute phase symptoms.
Nursing Management for Patients with Lumbar Disc Prolapse
- Bed Rest: Encourage the patient to remain on bed rest.
- Drug Therapy: Administer appropriate analgesic and anti-inflammatory drugs.
- Heat and Massage: Utilize heat and massage treatments by a physiotherapist to relax muscles.
- Neurological Deficit Monitoring: Watch for any neurological deficits, such as muscle weakness, atrophy, loss of sensory/motor function, or unrelieved acute pain.
- Gradual Activity Increase: Have the patient increase activity gradually.
- Surgical Intervention: Prepare for surgical intervention (laminectomy) when indicated, to remove the ruptured disc.
- Discharge Planning & Health Teaching: Encourage patient to do lumbar flexion exercises. Advise the patient to sleep on side with knees and hips flexed. Encourage proper posture. Consider a lumbar support (corset).
Management of Patients Following Laminectomy
- Laminectomy: Removal of the lamina to expose the neural elements of the spinal canal. Allows for inspection, identification, and removal of pathology/compression from the spinal cord and roots.
Post-Operative Nursing Management for Cervical Disc
- Vital signs and neuro checks: Monitor vital signs and neurological status frequently.
- Sore throat management: Be aware of sore throats as a common complaint and avoid throat numbing sprays.
- Pulmonary secretions: Observe for pulmonary secretions.
Nursing Process - Assessment (Pre-operative)
- Past injury: Assess for past neck injury
- Pain: Assess pain onset, location, radiation
- Cervical spine area: Assess area around the cervical spine by palpation to assess muscle tone and tenderness
- Range of motion: Assess range of motion in the neck and shoulders
- Surgical info: Determine the patient's need for information about the planned operative procedure.
Post-Operative Assessment
- Vital signs monitoring: Monitor blood pressure (BP) and pulse.
- Bleeding evaluation: Evaluate any bleeding.
- Drainage inspection: Inspect the dressing for serosanguineous drainage.
- Headache assessment: Assess for headaches.
- Extremity weakness evaluation: Check for weakness in upper and lower extremities.
Nursing Diagnoses
- Pain: Pain related to surgical procedure.
- Interventions: Keep the patient flat in bed for 12-24 hours. Administer analgesics as needed. Consider a soft diet if dysphagia is present.
- Impaired Physical Mobility: Impaired physical mobility related to post-operative surgical regimen.
- Interventions: Use of cervical collar. Teach patient to turn the body instead of the neck when looking from side to side. Encourage wearing shoes when ambulating.
Patient Teaching & Home Health Care
- Cervical collar use: The cervical collar is usually worn for 6 weeks.
- Neck movement restrictions: caution against extreme neck movements (flexing, extending, rotating) during activities/exercises. Avoid the prone position while sleeping.
- Symptom monitoring: Encourage monitoring of signs and symptoms, such as fever and wound drainage.
- Positioning and activity: Avoid prolonged sitting or standing periods (more than 30 minutes). Alternate tasks that don't involve body movement.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.