Podcast
Questions and Answers
Which type of neurons receives input from Aδ, C, and Aβ fibers?
Which type of neurons receives input from Aδ, C, and Aβ fibers?
- Second-order neurons
- Wide-dynamic-range (WDR) neurons (correct)
- Primary afferent neurons
- Nociceptive neurons
Where do the second-order neurons synapse with third-order neurons?
Where do the second-order neurons synapse with third-order neurons?
- Lateral thalamus and intralaminar nuclei (correct)
- Substantia gelatinosa
- Anterior commissure
- Rexed laminae I, II, and V
What is the primary function of the tract of Lissauer?
What is the primary function of the tract of Lissauer?
- To ascend pain signals to the thalamus
- To segregate and ascending/descending pain signals (correct)
- To transmit pain signals from the trunk and lower extremities
- To synapse with second-order neurons
What happens to substance P release when enkephalin binds to opiate receptors?
What happens to substance P release when enkephalin binds to opiate receptors?
Which structure is involved in the descending efferent pathway that suppresses pain transmission?
Which structure is involved in the descending efferent pathway that suppresses pain transmission?
What is the consequence of poorly controlled acute pain?
What is the consequence of poorly controlled acute pain?
Where are the cell bodies of primary afferent neurons located?
Where are the cell bodies of primary afferent neurons located?
What is necessary for the perception of pain?
What is necessary for the perception of pain?
What is the classification of pain based on?
What is the classification of pain based on?
Which type of pain is associated with stimulation of specific nociceptors?
Which type of pain is associated with stimulation of specific nociceptors?
What is the characteristic of somatic pain?
What is the characteristic of somatic pain?
What is the characteristic of visceral pain?
What is the characteristic of visceral pain?
What is the result of sensitization of nociceptive pathway from mx mediators released at site of tissue inflammation?
What is the result of sensitization of nociceptive pathway from mx mediators released at site of tissue inflammation?
What is the process of transformation of noxious stimuli into an action potential?
What is the process of transformation of noxious stimuli into an action potential?
What type of pain is caused by damage to peripheral or central neural structures?
What type of pain is caused by damage to peripheral or central neural structures?
What type of nociceptors elicit fast-sharp pain?
What type of nociceptors elicit fast-sharp pain?
Which of the following neurotransmitters is released from peripheral afferent nociceptor C fibers and involved in slow, chronic pain?
Which of the following neurotransmitters is released from peripheral afferent nociceptor C fibers and involved in slow, chronic pain?
What is the primary effect of bradykinin on peripheral nociceptors?
What is the primary effect of bradykinin on peripheral nociceptors?
Which of the following chemical mediators is released from mast cells, basophils, and platelets via substance P?
Which of the following chemical mediators is released from mast cells, basophils, and platelets via substance P?
What is the primary effect of prostaglandins on peripheral nociceptors?
What is the primary effect of prostaglandins on peripheral nociceptors?
Which of the following chemical mediators is released from platelets after tissue injury?
Which of the following chemical mediators is released from platelets after tissue injury?
What is the primary effect of calcitonin gene-related peptide (CGRP) on peripheral nociceptors?
What is the primary effect of calcitonin gene-related peptide (CGRP) on peripheral nociceptors?
What is the primary effect of cytokines on prostaglandin production?
What is the primary effect of cytokines on prostaglandin production?
What is the sequence of events that occurs when chemical mediators and neurotransmitters stimulate peripheral nociceptors?
What is the sequence of events that occurs when chemical mediators and neurotransmitters stimulate peripheral nociceptors?
What is a contraindication for the use of SNRIs?
What is a contraindication for the use of SNRIs?
What is the primary use of SSRIs?
What is the primary use of SSRIs?
What is a characteristic of serotonin syndrome?
What is a characteristic of serotonin syndrome?
What is the mechanism of action of corticosteroids in pain management?
What is the mechanism of action of corticosteroids in pain management?
What is a potential side effect of corticosteroids?
What is a potential side effect of corticosteroids?
What is the mechanism of action of methadone's D-isomer?
What is the mechanism of action of methadone's D-isomer?
What is a characteristic of methadone?
What is a characteristic of methadone?
What is a potential benefit of methadone in chronic pain management?
What is a potential benefit of methadone in chronic pain management?
Why may opioids need to be increased by 30-100% in intraoperative anesthesia?
Why may opioids need to be increased by 30-100% in intraoperative anesthesia?
What is a useful indicator for estimating adequate analgesia with general anesthesia?
What is a useful indicator for estimating adequate analgesia with general anesthesia?
What is a recommendation for postoperative pain management in elderly patients?
What is a recommendation for postoperative pain management in elderly patients?
What is a characteristic of pain processing in aging adults?
What is a characteristic of pain processing in aging adults?
What is a consequence of repeated exposure to untreated painful stimuli in premature and full-term infants?
What is a consequence of repeated exposure to untreated painful stimuli in premature and full-term infants?
What is the primary reason for using opioid analgesics as first-line therapy in elderly patients?
What is the primary reason for using opioid analgesics as first-line therapy in elderly patients?
What is a characteristic of pain perception in pediatric patients?
What is a characteristic of pain perception in pediatric patients?
What is a consideration for postoperative pain management in elderly patients?
What is a consideration for postoperative pain management in elderly patients?
Flashcards are hidden until you start studying
Study Notes
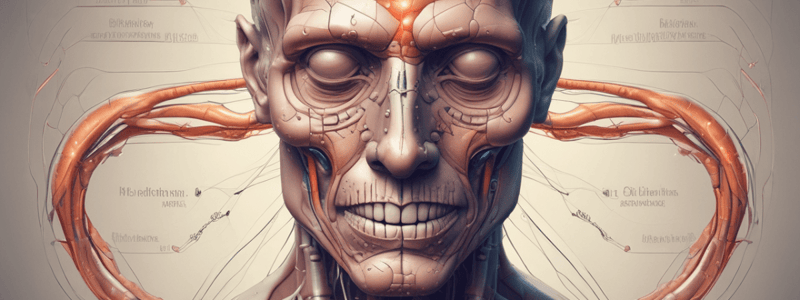
Pain Classification and Physiology
- Pain can be classified based on longevity (acute vs. chronic) and underlying pathophysiology (nociceptive or non-nociceptive)
- Nociceptive pain is associated with stimulation of specific nociceptors and can be either somatic or visceral
- Somatic pain has an identifiable locus and is well localized, sharp, and hurts at the point/area of stimulus
- Visceral pain is often associated with distension of organ capsules or obstruction of hollow viscus, and is diffuse, dull, cramping, squeezing, or vague in nature
- Non-nociceptive pain is caused by damage to peripheral or central neural structures, resulting in abnormal processing of painful stimuli
- Inflammatory pain results from sensitization of the nociceptive pathway from mediators released at the site of tissue inflammation without neural injury
Somatic Nociceptive Pain Pathway
- Transduction: transformation of noxious stimuli into an action potential
- Peripheral nociceptors are categorized according to morphology:
- Myelinated Aδ elicit fast-sharp pain
- Nonmyelinated C fibers elicit slow-dull, burning, throbbing, and aching pain
- Biochemical events take place, including:
- Release of chemical mediators from inflammatory response and neurotransmitters from nociceptive nerve endings
- Substance P release from peripheral afferent nociceptor C fibers, involved in slow, chronic pain
- Glutamate release from Aδ and C primary afferent fibers, causing initial, fast, sharp pain
- Bradykinin release during inflammatory process, directly stimulating peripheral nociceptors
- Histamine release from mast cells, basophils, and platelets, acting on various histamine receptors
- Serotonin release from platelets, acting on multiple receptors and nociceptors
- Prostaglandins synthesized from COX-1 and COX-2, sensitizing peripheral nociceptors
- Cytokines released in response to tissue injury, leading to increased PG production
- Calcitonin gene-related peptide release from peripheral afferent nociceptor C fibers, producing local cutaneous vasodilation and plasma extravasation
Transmission and Modulation
- Transmission: action potential conducted from periphery to CNS
- Primary afferent neurons Aδ and C fibers cell bodies located in dorsal root ganglia of spinal cord
- 2 types of 2nd-order neurons:
- Nociceptive neurons receive input from Aδ and C fibers
- Wide-dynamic-range (WDR) neurons receive input from Aδ, C, and Aβ fibers
- Modulation: involves altering neural afferent activity along the pain pathway
- Suppression occurs through local inhibitory interneurons and descending efferent pathways
- Descending axons from cerebral cortex, hypothalamus, thalamus, periaqueductal gray area, nucleus raphe magnus, and locus coeruleus synapse with and suppress pain transmission to brainstem and spinal cord dorsal horn
Perception
- Occurs once the signal is recognized by various areas of the brain, including amygdala, somatosensory areas of cortex, hypothalamus, and anterior cingulate cortex
Physiologic Consequences
- Acute pain is responsive to pharmacotherapy and treatment of the precipitating cause
- Poorly controlled acute pain may lead to chronic pain states
- Contraindications for certain medications, such as recent MI, prolonged QTi, cardiac dysrhythmias, and unstable CHF
Pharmacological Management
- SNRIs (duloxetine, venlafaxine) lack affinity for cholinergic, histaminergic, and adrenergic receptors
- SSRIs primarily used for treatment of depression, with relatively weak analgesic effects
- Corticosteroids used as adjuncts for management of acute onset and chronic pain syndromes
- Methadone: a synthetic opioid with a racemic mixture of two enantiomers, D-isomer (S-methadone) and L-isomer (R-methadone)
- Intraoperative management: opioids may need to be increased by 30-100% compared to opioid-naïve patients
- Postoperative management: consider IV PCA if unable to do RA/CPNB
Special Populations
- Elderly: alterations in pain processing and perception, with decreased nociceptive processing and neurotransmitters in CNS
- Pediatric: nociceptive pathways are well developed in premature and full-term infants, but maturation of descending pathway precedes ascending neural pathway
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.