Podcast
Questions and Answers
During skeletal muscle differentiation, what role do satellite cells play following a muscle injury?
During skeletal muscle differentiation, what role do satellite cells play following a muscle injury?
- They transform into myotubes, contributing to muscle fiber growth.
- They fuse with existing muscle fibers to repair them.
- They proliferate and produce new muscle fibers. (correct)
- They differentiate into connective tissue to support the damaged area.
If a muscle cell were unable to produce adequate amounts of ATP, which of the following processes would be most directly affected?
If a muscle cell were unable to produce adequate amounts of ATP, which of the following processes would be most directly affected?
- The release of calcium ions from the sarcoplasmic reticulum.
- The synthesis of actin and myosin filaments.
- The active transport of calcium ions back into the sarcoplasmic reticulum. (correct)
- The sliding of actin and myosin filaments during contraction.
Which structural feature is unique to cardiac muscle tissue and facilitates rapid communication between cells?
Which structural feature is unique to cardiac muscle tissue and facilitates rapid communication between cells?
- Myofibrils
- Intercalated discs (correct)
- Sarcoplasmic reticulum
- Transverse tubules
How does the arrangement of myofilaments differ between skeletal and smooth muscle tissue?
How does the arrangement of myofilaments differ between skeletal and smooth muscle tissue?
Following a stroke that damages the somatic motor cortex, a patient experiences difficulty voluntarily moving their right arm. Which type of neuron is most likely affected by this damage?
Following a stroke that damages the somatic motor cortex, a patient experiences difficulty voluntarily moving their right arm. Which type of neuron is most likely affected by this damage?
How do astrocytes contribute to neuronal function in the central nervous system?
How do astrocytes contribute to neuronal function in the central nervous system?
What is the primary function of oligodendrocytes in the central nervous system?
What is the primary function of oligodendrocytes in the central nervous system?
Which glial cell type is responsible for the immune defense in the central nervous system?
Which glial cell type is responsible for the immune defense in the central nervous system?
Which feature is characteristic of hyaline cartilage that contributes to its function in joints?
Which feature is characteristic of hyaline cartilage that contributes to its function in joints?
Unlike other types of cartilage, fibrocartilage lacks a perichondrium. How does this affect its ability to repair?
Unlike other types of cartilage, fibrocartilage lacks a perichondrium. How does this affect its ability to repair?
How does the presence of elastic fibers affect the functional properties of elastic cartilage compared to hyaline cartilage?
How does the presence of elastic fibers affect the functional properties of elastic cartilage compared to hyaline cartilage?
What is the role of lacunae in both cartilage and bone tissue?
What is the role of lacunae in both cartilage and bone tissue?
How does periosteum contribute to bone repair after a fracture?
How does periosteum contribute to bone repair after a fracture?
What is the key difference between intramembranous and endochondral ossification?
What is the key difference between intramembranous and endochondral ossification?
Which type of bone is characterized by interconnecting cavities and is typically found in the interior of bones?
Which type of bone is characterized by interconnecting cavities and is typically found in the interior of bones?
Which of the following is a key function of the endosteum?
Which of the following is a key function of the endosteum?
How do synarthroses differ from diarthroses?
How do synarthroses differ from diarthroses?
In diarthrotic joints, what is the function of the specialized type A synovial cells?
In diarthrotic joints, what is the function of the specialized type A synovial cells?
What is the primary role of type B synovial cells in diarthrotic joints?
What is the primary role of type B synovial cells in diarthrotic joints?
Which type of joint is characterized by bones joined by dense connective tissue, providing limited movement?
Which type of joint is characterized by bones joined by dense connective tissue, providing limited movement?
Flashcards
Muscle Tissue
Muscle Tissue
Derived from mesoderm, these tissues are composed of cells optimized for contractility. Key feature: sliding action of thick myosin and thin actin filaments.
Skeletal Muscle
Skeletal Muscle
Voluntary muscles mostly attached to bone
Cardiac Muscle
Cardiac Muscle
Involuntary muscles found in the heart
Smooth Muscle
Smooth Muscle
Signup and view all the flashcards
Endomysium
Endomysium
Signup and view all the flashcards
Perimysium
Perimysium
Signup and view all the flashcards
Epimysium
Epimysium
Signup and view all the flashcards
Sarcoplasmic Reticulum
Sarcoplasmic Reticulum
Signup and view all the flashcards
Transverse Tubules
Transverse Tubules
Signup and view all the flashcards
Striations (Muscle)
Striations (Muscle)
Signup and view all the flashcards
Sarcomere
Sarcomere
Signup and view all the flashcards
Synapse
Synapse
Signup and view all the flashcards
Dendrites
Dendrites
Signup and view all the flashcards
Glial Cells
Glial Cells
Signup and view all the flashcards
Oligodendrocytes
Oligodendrocytes
Signup and view all the flashcards
Microglia
Microglia
Signup and view all the flashcards
Bone
Bone
Signup and view all the flashcards
Endosteum
Endosteum
Signup and view all the flashcards
Periosteum
Periosteum
Signup and view all the flashcards
Osteoblasts
Osteoblasts
Signup and view all the flashcards
Study Notes
Muscle Tissue
- Derived from mesoderm
- Composed of cells optimized for contractility
Muscle Contractility
- Optimized by the sliding action of thick myosin filaments along thin actin filaments
Muscle Organelles
- Specialized organelles are referred to with the prefix sarco
Muscle Types
- Skeletal muscle consists of voluntary muscles mostly attached to bone
- Cardiac muscle consists of involuntary muscles found in the heart
- Smooth muscle consists of involuntary muscles found in visceral organs and soft tissues
Skeletal Muscle Properties
- Made of muscle fibers
- Long, cylindrical, and multinucleated contractile cells
- Possess elongated nuclei, located peripherally under the sarcolemma
- Organized by thin layers of collagenous supporting tissue
Skeletal Muscle Connective Tissue
- Endomysium surrounds the muscle fiber, consisting of loose (areolar) connective tissue
- Perimysium surrounds the muscle fascicle, consisting of dense irregular connective tissue
- Epimysium surrounds the whole muscle, consisting of dense irregular connective tissue
- Deep fascia overlies the epimysium and is continuous with joint connective tissue
Muscle Fiber Organization
- Skeletal muscle exhibits striations, alternating light and dark bands
- Dark bands are A bands
- Light bands are I bands
- The Z disc bisects each I band
Sarcomere Structure
- Sarcomere is the repetitive functional unit of the muscle contractile apparatus
- Sarcomeres extend from Z disc to Z disc
- They are arranged end-to-end from myofibrils
- A bands contain thick myosin filaments
- I bands contain thin actin filaments
Sarcoplasmic Reticulum
- It is a membranous smooth ER found in skeletal muscle fibers
- Sequesters Ca2+ during muscle contraction
- Terminal cisterns are expanded structures near T tubules
Transverse (T) Tubules
- Are invaginations of the cell sarcolemma
- It encircles each myofibril
- Located near the aligned A and I bands
Skeletal Muscle Fiber Types
- Slow oxidative fibers are for slow contractions over long periods
- They have many mitochondria and depend on oxidative metabolism
- They are dark red in color due to high myoglobin and surrounding capillaries
- Postural muscles of the back are an example
- Fast glycolytic fibers are for rapid, short-term contractions
- They have few mitochondria and depend on anaerobic metabolism
- They are white in color due to less myoglobin & surrounding capillaries
- Major muscles of the legs are an example
- Fast oxidative-glycolytic fibers have physiological and histological features that are intermediate between the other two types
- Extraocular muscles are an example
Cardiac Muscle
- Striated, similarly arranged to skeletal muscle tissue
- Fibers arranged in series are joined at interdigitating regions called intercalated discs
- Contains long, uninucleated, branching contractile cells
- Possess centrally-located nuclei
- Sparser, less well-organized myofibrils
- With fibroblast activity
Intercalated Discs
- Consist of many junctional complexes
- Transverse sections contain desmosomes and fascia adherens
- Longitudinal sections contain gap junctions
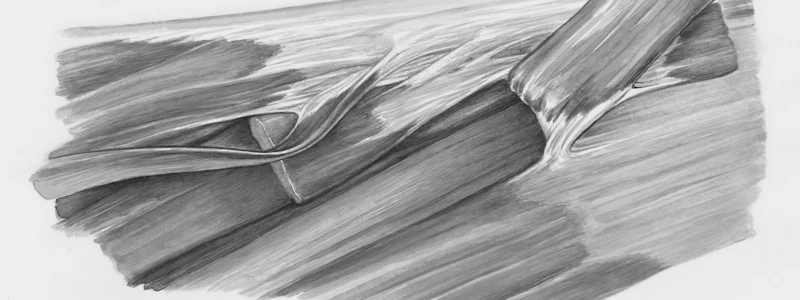
Smooth Muscle
- Possesses a rudimentary sarcoplasmic reticulum
- Lacks T tubules, contains caveolae
- Not arranged in sarcomeres (unstriated)
- Bundles of thick and thin myofilaments crisscross the sarcoplasm obliquely
- Actin filaments insert into dense bodies
- Lacks troponin and tropomyosin, uses calmodulin & MLCK
- Stimulation from the autonomic nervous system is propagated via gap junctions, allowing synchronized contraction
Skeletal Muscle Control
- It's under the influence of the autonomic nervous system and various hormones
- A component of visceral organs and blood vessels
- Specialized for slow, steady contractions
- Smooth muscle fibers are elongated, fusiform in shape, unstriated with a central nucleus
- Linked by numerous gap junctions
- Enclosed by an external lamina and a network of collagen fibers (Types I & III)
- Cells shorten and broaden on contraction
Nervous Tissue Derivation
- Derived from Ectoderm
Nervous Tissue Cells
- Parenchyma: Neurons
- Stroma: Glial cells
Nervous System Function
- Distributed throughout the body as an integrated communications network
Nervous System Divisions
- Central Nervous System includes the brain and spinal cord
- Peripheral Nervous System includes cranial, spinal, and peripheral nerves and ganglia
Neuron Definition
- Functional unit of both the CNS and PNS
- Responds to environmental stimuli by reversing the ionic gradient across the plasma membrane of the cell
Nerve Impulse
- Also known as the Action Potential/Depolarization Wave
- Consists of the reversal of the ionic gradient starting at the place where the stimulus is received
- Propagated across the cell's entire plasma membrane, traveling along the neuron's processes
- Signal is eventually transmitted to other neurons, muscles, and glands
Neuron Dendrites
- Numerous elongated processes extending from the cell body
- Receives stimuli from other neurons at unique sites called synapses
Neuron Cell Body
- Also known as Soma/Perikaryon
- Contains the nucleus and organelles
- Synthetic center for the entire neuron
Neuron Axon
- Single long process extending from the cell body
- Specialized to generate and conduct nerve impulses to other cells
Neuron Cytoplasm
- Contains Nissl bodies, regions with numerous ribosomes and highly developed RER
- Abundant cytoskeleton, including microtubules, actin filaments, and intermediate filaments
Neuron Classification
- Sensory/Afferent neurons receive stimuli from receptors
- Motor/Efferent neurons send impulses to effector organs such as muscle fibers and glands
- Somatic motor neurons: voluntary; innervate skeletal muscle
- Autonomic motor neurons: involuntary; innervate glands, cardiac muscle, and smooth muscle
- Interneurons establish relationships among other neurons, usually multipolar or anaxonic
Neuron Cell Body Components
- Contains the nucleus and cytoplasm
- Excludes the cell processes
- Nucleus is large and euchromatic
Dendrite Properties
- Highly branched, tapering processes emerging off the cell body
- Principal signal reception and processing site on neurons
- End in either specialized sensory receptors or form synapses with neighboring neurons
- Dendritic spines are intial processing sites for synaptic signals
Axon Features
- Usually singular
- Long cylindrical process with less branching
- Originates from the axon hillock which is a pyramid-shaped region of the perikaryon
- Ends in terminal boutons that terminate at other neurons or effector organs
- Contains a myelin sheath for insulation
- Axoplasm contains mostly mitochondria, microtubules, neurofilaments, and vesicles
Synapse Characteristics
- Sites where nerve impulses are transmitted from one neuron to the next cell, muscle, or gland
- Converts an electrical signal into a chemical signal
- Contains a presynaptic axon terminal (terminal bouton), synaptic cleft, and postsynaptic cell membrane
Glial Cells
- Support neuronal survival and fosters an optimal environment for neuronal activity
- Estimated to be 10x more abundant than neurons
CNS Glial Cells
- Oligodendrocytes form and maintain the myelin sheath
- Astrocytes provide physical and metabolic support
- Microglia are phagocytic cells
- Ependymal cells line the ventricles for the formation of CSF
PNS Glial Cells
- Satellite cells maintain the environment around the neuronal body in a ganglion
- Schwann cells form and maintain the myelin sheath
Cartilage
- Tough, durable form of connective tissue
- ECM characterized by large amounts of GAGs and proteoglycans
Cartilage Functions
- Cushioning/Shock absorption: able to bear stress without distortion due to firm but resilient ECM
- Lubrication: smooth surface allows sliding and facilitates bone movement
- Guides development of long bones
Cartilage Cells
- Parenchyma consists of Chondrocytes which synthesize & maintain ECM located in matrix cavities called lacunae
Cartilage Vessels
- Lacks vascular supply, receives nutrients by diffusion from capillaries in surrounding connective tissue
Perichondrium
- Sheath of dense CT that surrounds cartilage
- Harbors the blood supply and neural component
- Lacks nerve supply
Cartilage matrix
- Variation in composition dictates the type of cartilage
- Components include Type II Collagen fibrils, Hyaluronan, Proteoglycans, and Water
Hyaline Cartilage Properties
- Hyalos is Greek for glass (homogeneous, semitransparent in fresh state)
- Most common type of cartilage
Hyaline Cartilage Location
- Articular surface of movable joints
- Walls of larger respiratory passages
- Ventral ends of ribs (costal cartilages)
- Epiphyseal ribs of long bones for longitudinal bone growth
- Temporary skeleton in the embryo
Cartilage composition
- Collagen Type II is present
- Aggrecan binds to water
- Chondronectin enables adherence of chondrocytes to ECM
Perichondrium Structure
- Sheath covering hyaline cartilage made of dense irregular CT
- Outer fibrous layer contains type I collagen, fibroblasts, and blood vessels
- Inner cellular layer contains chondroblasts
Chondrocytes Properties
- Small, round nuclei appear shrunken
- Pale-staining cytoplasm
- Arranged in isogenous groups (clusters)
Types of cartilaginous matrix
- Territorial matrix--matrix that surrounds each chondrocyte or isogenous group
- Interterritorial matrix--matrix that fills the space between isogenous groups and chondrocytes
Elastic Cartilage features
- Similar to hyaline cartilage but abundant in elastic fibers & chondrocytes
- Yellowish in color
- Flexible support for tissues that need stretch
- Has a surrounding perichondrium
- Chondroblasts are responsible for oppositional growth of the matrix
Elastic cartilaginous matrix
- Contains elastic fibers to gives a rough appearance to the matrix
- Also contains Type II Collagen
Elastic Cartilage Locations
- Epiglottis
- Auditory canal / tube
- Larynx
- Pinna/auricle
Fibrocartilage characteristics
- Provides cushioning, firm support, and tensile strength
- Lacks perichondrium
Fibrocartilage locations
- Pubic symphysis
- Intervertebral disk
- Insertion of tendons/ligaments
Chondroyctes Properties
- Chondrocytes are smaller and fewer, arranged in lacunae in small groups in parallel rows or columns
ECM composition
- Type I collagen gives matrix a dense and coarse appearance
- Type II Collagen is also present
Bone definition
- Hard and strong connective tissue
- ECM is hard and calcified
Bone functions
- Protection & Support
- Calcium reserve
- Blood cell production
- Movement
Bone Structures
- Lined by endosteum (internal surface surrounding the marrow cavity)
- Periosteum is the external surface of the bone
Bone matrix properties
- 50% of dry weight is inorganic material
- Contains Calcium hydroxyapatite as the most abundant part of the matrix
- Also contains Bicarbonate, Citrate, Magnesium, Potassium, Sodium, and Calcium phosphate
Bone organic material
- Type I Collagen
- Proteoglycans and glycoproteins
Types of Bone Cells
- Osteocytes are small cells with cytoplasmic processes that extend into canaliculi
- They deposit matrix around themselves
- Occupies a space in the matrix called a lacuna
Osteoblasts
- Synthesize and secrete organic matrix components
- Can differentiate as osteocytes and become entrapped in lacunae or flatten to cover the matrix surface as bone lining cells – cuboidal or low columnar in shape
Osteoclasts
- Function in bone remodeling & resorption of calcified bone matrix
- They are large, multinucleated cells derived from monocytes
Periosteum vs Endosteum
- Periosteum: outer fibrous layer of dense connective tissue, Type I collagen, fibroblasts, blood vessels
- Endosteum: covers trabeculae of bony matrix
Types and Organization of Bone
- Compact bone: dense bone beneath the periosteum
- Spongy/Cancellous bone: deep area of the bone consisting of interconnecting cavities
- Woven bone: immature bone formed in osteogenesis or repair
- Lamellar bone: lamellae concentrically organized around small central canals
Osteogenesis
-
Intramembranous ossification: flat bone formation; mesenchymal cells differentiate into osteoblasts and deposit osteoid - unmineralized prebone that later becomes calcified
-
Endochondral ossification: long bone formation; hyaline cartilage serves a cartilage model; cartilage proliferates then calcifies, eventually replaced by bone
Joints Definition
- Regions where adjacent bones are capped and held together by CT
Types of Joints
- Synarthroses limited or no movement; can be fibrous or cartilaginous
- Synostoses essentially no movement – skull sutures
- Syndesmoses bones joined by dense CT – interosseous ligament of inferior tibiofibular joint, posterior sacroiliac joints
- Symphyses thick pad of fibrocartilage between thin articular cartilage – pubic symphysis, intervertebral disks
- Diarthroses free bone movement – elbow, knee; ligaments and capsule of dense CT maintain alignment
Specialized Joint Cells
- Type A cells / Macrophage-like synovial cells are derived from blood monocytes, remove wear and tear debris from synovial fluid, and regulate inflammatory events in diarthrotic joints
- Type B cells / Fibroblastic synovial cells produce abundant hyaluronan and smaller amounts of proteoglycans
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.