Podcast
Questions and Answers
Which of the following accurately describes the sequence of events in excitation-contraction coupling in skeletal muscle?
Which of the following accurately describes the sequence of events in excitation-contraction coupling in skeletal muscle?
- Acetylcholine release, action potential in the muscle cell membrane, tropomyosin binds to actin.
- Action potential in the muscle cell membrane, calcium release from sarcoplasmic reticulum, interaction of actin and myosin. (correct)
- Action potential in the muscle cell membrane, calcium release from T-tubules, interaction of actin and myosin.
- Acetylcholine binds to receptors, action potential in T-tubules, calcium reuptake into sarcoplasmic reticulum.
How does the somatic nervous system regulate skeletal muscle contraction?
How does the somatic nervous system regulate skeletal muscle contraction?
- By directly innervating multiple muscle fibers with multiple motor neurons.
- By indirectly controlling muscle fiber activity through the autonomic nervous system.
- By releasing hormones that stimulate muscle fiber contraction.
- By innervating muscle fibers with a single motor neuron as part of a motor unit. (correct)
What is the role of acetylcholinesterase at the neuromuscular junction (NMJ)?
What is the role of acetylcholinesterase at the neuromuscular junction (NMJ)?
- To stimulate the release of calcium from the sarcoplasmic reticulum.
- To activate the nicotinic acetylcholine receptor.
- To degrade acetylcholine, allowing for muscle relaxation. (correct)
- To propagate the action potential across the muscle cell membrane
During muscle contraction, what happens to the length of the A-band in a sarcomere?
During muscle contraction, what happens to the length of the A-band in a sarcomere?
What is the primary role of T-tubules in skeletal muscle function?
What is the primary role of T-tubules in skeletal muscle function?
What is the key difference between a muscle twitch and tetanus?
What is the key difference between a muscle twitch and tetanus?
Which characteristic is associated with Type I muscle fibers?
Which characteristic is associated with Type I muscle fibers?
Which of the following is a key component of the autonomic nervous system?
Which of the following is a key component of the autonomic nervous system?
How does the sympathetic nervous system affect heart rate?
How does the sympathetic nervous system affect heart rate?
What is the primary effect of thyroid hormones on metabolism?
What is the primary effect of thyroid hormones on metabolism?
Flashcards
Motor unit
Motor unit
A single motor neuron and all the muscle fibers it innervates.
Neuromuscular junction (NMJ)
Neuromuscular junction (NMJ)
Specialized synapse between a motor neuron and the skeletal muscle cell.
Excitation-contraction coupling
Excitation-contraction coupling
Transformation of an electrical signal into muscle contraction.
Myofibrils
Myofibrils
Signup and view all the flashcards
Z-discs
Z-discs
Signup and view all the flashcards
Concentric contraction
Concentric contraction
Signup and view all the flashcards
Eccentric contraction
Eccentric contraction
Signup and view all the flashcards
Parasympathetic
Parasympathetic
Signup and view all the flashcards
Sympathetic system
Sympathetic system
Signup and view all the flashcards
Endocrine system function
Endocrine system function
Signup and view all the flashcards
Study Notes
- Afferent information travels towards the CNS.
- Efferent information travels away from the CNS.
Muscle Physiology - Skeletal Muscle
- Skeletal muscle functions include movement, support (abdominal wall), posture, temperature regulation, and physical communication.
- Somatic nervous system regulates skeletal muscles, enabling voluntary movements.
- A motor unit comprises a single motor neuron and all muscle fibers it innervates.
- One muscle cell is innervated by a single motor neuron.
- A motor neuron innervates hundreds to thousands of muscle fibers.
Neuromuscular Junction (NMJ)
- NMJ is a specialized synapse between a somatic (alpha) motor neuron's nerve terminal and the motor end plate of the skeletal muscle cell.
- Action potential propagation usually results in an action potential across the muscle cell membrane.
- Excitation-contraction (E/C) coupling transforms an electrical signal into the contraction of sarcomeres, occurring in the sarcoplasmic triad.
- Acetylcholine (ACh) is utilized at all NMJs.
- ACh activates nicotinic acetylcholine receptors, causing an EPSP/depolarization.
Sarcolemma and Sarcoplasmic Reticulum
- T-tubules invaginate the myofibrils and are continuous with the sarcolemma.
- Terminal cisternae are closely opposed to T-tubules.
- The sarcoplasmic reticulum surrounds myofibrils as a network of interconnected "sacrotubles," where E/C coupling occurs.
- A single muscle cell contains many myofibrils.
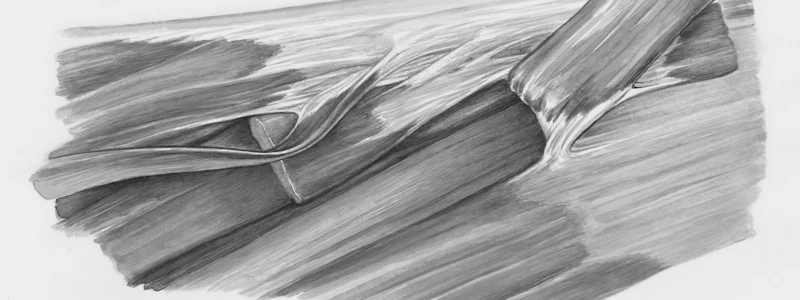
Myofibrils and Sarcomeres
- Myofibrils are serial-repeating sarcomeres, which are the smallest contractile units of a muscle cell.
- Thin filaments: actin
- Thick filaments: myosin
- Sarcomeres shorten during contraction as thick and thin filaments slide past one another.
- The length of filaments remains constant during sarcomere shortening via the sliding of thin filaments toward M-lines.
Sarcomere Components
- Z-discs: borders between neighboring sarcomeres
- A-band: length of the thick filament
- M-line: the center of the sarcomere
- I-band: region with thin filaments, without overlapping thick filaments
- H-zone: region with thick filaments, without overlapping thin filaments
Muscle Contraction and Relaxation
- Muscle contraction occurs when:
- ACh binds to skeletal muscle fibers.
- Action potential moves into T-tubules.
- Calcium is released by the sarcoplasmic reticulum.
- Calcium binds to troponin, enabling active cross-bridge cycling.
- A myosin ATPase is involved in the contraction.
- Muscle relaxation occurs when:
- Acetylcholinesterase degrades ACh.
- Calcium is pumped into the ECF and sarcoplasmic reticulum.
- Tropomyosin blocks cross-bridge formation.
- Skeletal muscle contraction is prevented.
Cross-Bridge Cycle and Muscle Contraction Types
- Calcium concentration is low, tropomyosin blocks actin filament binding sites.
- Calcium release allows binding, and cross-bridge attachment occurs.
- A power stroke then takes place.
- ATP binding to myosin causes cross-bridge detachment.
- Eccentric contraction involves muscle lengthening.
- Isometric contraction involves no change in muscle length.
- Concentric contraction involves muscle shortening.
Muscle Twitch and Tetanus
- Twitch is caused by a single action potential.
- Infused tetanus involves a lower stimulation rate, allowing partial muscle relaxation between stimuli.
- Fused tetanus involves a high stimulation rate, with no muscle relaxation between stimuli.
- Whole muscle movements are smooth and sustained due to multiple motor unit activation.
- Contraction strength increases with more motor units, frequency of stimulation, and increases in myofibers thickness.
Muscle Fiber Types
- Type I fibers have slow contraction speeds and low strength, but high fatigue resistance.
- Type IIA fibers have fast contraction speeds, intermediate strength, and intermediate fatigue resistance.
- Type IIX fibers have fast contraction speeds and high strength, but low fatigue resistance.
- Asynchronous contraction of motor units allows for smooth movement.
Autonomic Nervous System
- The autonomic nervous system controls involuntary functions by regulating smooth muscles, cardiac cells, glands, and other tissues and is sometimes called the visceral motor system.
- The somatic motor system controls skeletal muscles allowing voluntary movement.
- The autonomic nervous system has includes two neurons per target cell.
- The ganglion is where the preganglionic neuron and postganglionic neuron meet.
- At the autonomic ganglion, the presynaptic cell is the preganglionic neuron, and the postsynaptic cell is the postganglionic neuron. The target tissue is the post synaptic cell.
Parasympathetic Nervous System
- The parasympathetic nervous system involves rest and digest functions.
- It has four cranial nerves (including vagus) that innervate all major internal organs.
- Most visceral organs are innervated by both sympathetic and parasympathetic systems, showing antagonistic effects on the same target cell.
- Both pre- and postganglionic neurons use acetylcholine (ACh).
- Nicotinic ACh receptors are at the ganglion, muscarinic receptors at the target cells.
- It decreases heart rate, which happens through cholinergic innervation via the vagus nerve, activation involving of M2 muscarinic receptors, indirectly opening K+ channels, and hyperpolarization.
- Stimulation of circular muscles via muscarinic receptors leads to muscle contraction and a decrease in pupil diameter.
- Preganglionic fibers originate in the brain stem, with terminal ganglia.
Sympathetic Nervous System
- Sympathetic nervous system functions involve fight or flight responses, including a short-term stress response.
- The sympathetic nervous system causes branching of preganglionic.
- The collateral (prevertebral) ganglia exists in the sympathetic nervous system.
- The adrenal medulla is part of the sympathetic nervous system.
- Some efferent fibers are both somatic and sympathetic.
- Some efferent fibers innervate blood vessels and sweat glands.
- Only sympathetically-innervated organs are the adrenal medulla, arrest or police muscles, sweat glands, and blood vessels.
- Preganglionic neurons release acetylcholine.
- Postganglionic neurons release norepinephrine (NE).
- Activation of Alpha 1 adrenergic receptors leads to vasoconstriction and pupil dilation.
- Activation of Beta 1 adrenergic receptors increases heart rate and contractility:
- Beta 1 receptors indirectly open calcium channels, leading to depolarization.
- Beta 2 adrenergic receptors cause dilation of bronchioles in the lung.
- Radial muscles, stimulated via alpha one receptors, lead to muscle contraction and pupil diameter increases.
- Preganglionic fibers originate in the spinal cord.
- Paravertebral ganglia run parallel to the spinal cord.
- Prevertebral ganglia are in front of the spinal cord.
Endocrine System and Metabolism
- Endocrine signals are blood-borne, relying on hormone diffusion into nearby capillaries.
- Endocrine glands are ductless by nature. Target cells have specific receptors that recognize and bind hormones.
- Functionally, the endocrine system regulates body metabolism, growth, and reproduction.
- Hormones use G protein-coupled receptors, enzyme-linked receptors, and intracellular receptors, but not ligand-gated cell receptors.
- Hydrophilic hormones interact with cell-surface receptors at target tissues being all peptide and protein hormones as well as epinephrine and norepinephrine.
- Hydrophobic hormones interact with intracellular receptors at target tissues including steroid and thyroid hormones.
- Metabolism includes all physical/chemical processes converting/using energy.
- Metabolic rate: amount of heat produced/minute (amount of O2 used/minute).
- Basal metabolic rate (BMR): rate of O2 consumption when awake + relaxed.
- Hyperthyroidism leads to high BMR, and hypothyroidism leads to low BMR.
- Transition between anabolism and catabolism occurs at rest.
- Absorptive states increase insulin secretion from pancreas, which lead to increased anabolism.
- Post-absorptive states increase glucagon secretion from pancreas which lead to increased catabolism.
- Insulin and glucagon are antagonistic.
- Adrenal hormones mediate stress, thyroid hormones control BMR and growth, and growth hormone drives growth and maintenance.
Homeostasis and Signaling
- Regulated variables in are ions, body temperature, and arterial pO2/pCO2.
- Variables not regulated are heart rate and hormone levels.
- The adrenal medulla is the only organ with single neuron innervation.
- For parasympathetic responses, receptors are muscarinic.
- Dorsal and ventral root ganglia are not involved in the autonomic nervous system.
- M2 muscarinic receptors control heart rate.
- Exocrine signaling involves cellular communication with the secretion of substances through ducts.
- The pituitary connects to the hypothalamus via the infundibulum with its anterior lobe exerting hormonal control while the posterior lobe exerts neural control.
- Posterior pituitary secretes ADH for high blood osmolality and oxytocin for lactation.
- The adrenal cortex uses steroid hormones for long-term stress response, while the adrenal medulla uses epinephrine and norepinephrine for short-term stress response.
- Alpha cells in the pancreas secrete glucagon, and beta cells secrete insulin.
- Insulin binds to receptor tyrosine kinase, which leads to dimerization of r and activation of rtk PhoSphorylates substrates.
Pancreas and Glucose Regulation
- The pancreas is a ductal gland producing and recreating pancreatic into the small intestine.
- Clusters of endocrine cells are scattered throughout the islets of Langerhans.
- Alpha cells produce glucagon, while beta cells produce insulin.
- Changes in blood glucose levels influence secretion of insulin and glucagon.
- Pancreatic hormones regulate blood glucose levels and influence cellular metabolism.
Insulin Receptor and Action
- The insulin receptor is a receptor tyrosine kinase.
- Insulin R phosphorylates itself and other proteins.
- Insulin binding leads to dimerization which leads to activation
- Activated RTK phosphorylates substrates.
- Activated insulin R leads to downstream signaling cascade in target cells like increased glucose uptake and anabolic effects.
- High blood glucose levels lead to increased insulin secretion, leading to increased glucose uptake from blood.
Glucose Uptake and Anabolic Effects
- GLUT4 recruitment to cell membranes helps to insulin enter cells via GLUT4.
- Insulin cells can't have glucose levels above 170 mg/dl.
- These can lead to increased glycogen synthesis (glucose-glycogen) in the liver and muscle and increased lipogenesis of glucose into triglycerides in adipocytes.
- Beta cells detect changes in blood glucose via GLUT2.
Hypothalamic-Pituitary Axis (HPA) and Adrenal Glands
- Corticotropin-releasing hormone stimulates the secretion of adrenocorticotropic hormone (ACTH) and the adrenal cortex - gluco-corticoids
- Thyrotropin-releasing hormone (TRH) stimulates thyroid and thyroid hormones.
- Adrenal glands has an Adrenal cortex that secretes steroid hormones and androgens that is Controlled by HPA.
- Adrenal medulla secretes epinephrine and norepinephrine into the blood that is Controlled by sympathetic division of the ANS
Stress Responses and Intracellular Receptors
- A shorter-term "fight-or-flight" response is present.
- There is also a longer-term stress response.
- Neural activity combines with hormones in the bloodstream to constitute fight-or-flight response.
- Steroid receptors are located in the cytosol with Hydrophobic hormones are transported with transport protein and Hydrophilic hormones are transported freely in the blood
- Hormone binding leads to receptor activation leading to changes in gene transcription leading to the physiological response of the target tissue
Thyroid and Metabolism
- Nearly all cells in the body are targets.
- In the liver, glucose metabolism and gluconeogenesis are promoted
- All other major normal growth and development are promoted
- For T4 it impacts BMR, affects calorigenic effects and increases metabolic heat and cold adaption.
- Protein synthesis, growth of skeleton occurs
- This is Critical for proper growth and development of CNS
Thyroid Imbalance
- Hyperthyroidism: high BMR, weight loss, nervousness, irritability, higher body temp, and intolerance to heat
- Hypothyroidism: low BMR, weight gain, lethargy, increased sleep, lower body temp, coarse skin, and slow pulse and repression
The Knee-Jerk Reflex
- First: patellar ligament or tendon is tapped leading to it stretching the tendon and quads
- Second: the Muscle stretch lead to activate and stretches the muscle spindle apparatus
- Third: afferent fibers carry sensory information to spinal cord through dorsal horns
- Fourth: In the spinal cord, afferent fibers fire action potentials onto alpha and gamma motor neurons
- Fifth: Motor neurons carry efferent information back to the thigh via ventral horns
- Sixth: Alpha motor neurons synapse onto the extra fusal fibers on quads- causing contraction
- Lastly: Gamma motor neuron synapses onto the intrafusal fibers of the quads causing muscle spindle apparatus to contract and reset
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.