Podcast
Questions and Answers
What type of protein is excessively produced in multiple myeloma?
What type of protein is excessively produced in multiple myeloma?
- Acute phase reactant
- Monoclonal immunoglobulin (correct)
- Polyclonal antibody
- Complement protein
Which of the following is a typical skeletal manifestation of multiple myeloma?
Which of the following is a typical skeletal manifestation of multiple myeloma?
- Extensive skeletal destruction (correct)
- Avascular necrosis
- Increased bone density
- Osteoblastoma
What is a common respiratory infection associated with multiple myeloma?
What is a common respiratory infection associated with multiple myeloma?
- Aspergillus
- Streptococcus pneumoniae (correct)
- Pneumocystis jirovecii
- Histoplasma capsulatum
Which of the following is a common general symptom observed in patients with multiple myeloma?
Which of the following is a common general symptom observed in patients with multiple myeloma?
Which radiological investigation is typically used to detect osteolytic lesions in multiple myeloma?
Which radiological investigation is typically used to detect osteolytic lesions in multiple myeloma?
The presence of Bence-Jones protein in the urine indicates which condition?
The presence of Bence-Jones protein in the urine indicates which condition?
What is the term for the increased level of calcium in the blood, often seen in multiple myeloma?
What is the term for the increased level of calcium in the blood, often seen in multiple myeloma?
Serum protein electrophoresis (SPEP) in multiple myeloma helps detect:
Serum protein electrophoresis (SPEP) in multiple myeloma helps detect:
What is the typical finding in bone marrow aspiration and biopsy in a patient with multiple myeloma?
What is the typical finding in bone marrow aspiration and biopsy in a patient with multiple myeloma?
Which of the following best describes the malignant cell type in multiple myeloma?
Which of the following best describes the malignant cell type in multiple myeloma?
Flashcards
Multiple Myeloma Definition
Multiple Myeloma Definition
Malignant proliferation of a single clone of plasma cells in the bone marrow.
Skeletal Destruction in MM
Skeletal Destruction in MM
Excessive skeletal destruction leading to osteolytic lesions, osteopenia and/or pathological fractures.
Key Features of MM
Key Features of MM
Bone pain, anemia, renal failure, hypercalcemia.
BM Plasmacytosis
BM Plasmacytosis
Signup and view all the flashcards
MM Classic triad
MM Classic triad
Signup and view all the flashcards
Multiple Myeloma Age
Multiple Myeloma Age
Signup and view all the flashcards
End-Organ Damage in MM
End-Organ Damage in MM
Signup and view all the flashcards
Immunotherapy for MM
Immunotherapy for MM
Signup and view all the flashcards
MM diagnostic criteria
MM diagnostic criteria
Signup and view all the flashcards
CRAB Criteria
CRAB Criteria
Signup and view all the flashcards
Study Notes
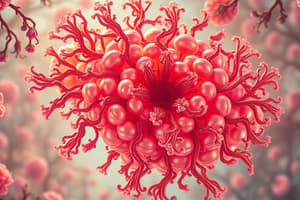
- Multiple myeloma is a malignant proliferation of a single clone of plasma cells in the bone marrow.
- This leads to excessive production of monoclonal immunoglobulin (M protein) and extensive skeletal destruction.
Clinical Picture
- The clinical picture of multiple myeloma can be remembered by the acronym "OLD AGE".
- Skeletal: Bone pains and pathological fractures are common.
- Renal: Acute kidney injury (AKI) and chronic kidney disease (CKD) can occur.
- Blood: Anemia and bleeding tendencies are present.
- Infections: Recurrent infections, especially with Streptococcus pneumoniae and gram-negative organisms.
- Neurological: Spinal cord compression leading to focal paraplegia can occur.
- General: Fatigue, generalized weakness, and weight loss are common symptoms.
- Hypercalcemia is often observed.
Investigations
- Skeletal: CT and X-ray show multiple osteolytic lesions, especially in the skull.
- Renal: Impaired renal function and Bence-Jones proteinuria (M protein) may be observed.
- Blood: Anemia and hypercalcemia are common.
- Electrophoresis and Immunofixation: Serum protein electrophoresis (SPEP) and urine protein electrophoresis (UPEP) detect M protein (Bence-Jones protein).
- Immunofixation identifies the immunoglobulin class of the M protein (commonly IgG, then IgA).
- Bone Marrow Aspiration and Biopsy: Shows BM plasmacytosis with sheets or clusters of plasma cells (>10% infiltration).
Treatment
- Chemotherapy: Melphalan, thalidomide, and prednisone are used.
- Immunotherapy: Monoclonal antibodies like elotuzumab and daratumumab are employed.
- New therapy: Selinexor, a nuclear export inhibitor, inhibits the transport of oncogenic proteins.
- Radiotherapy and bone marrow transplantation (BMT) are also treatment options.
- Multiple myeloma should be considered if an older patient develops a pathological fracture.
- An older patient with bone pain, anemia, renal failure, and hypercalcemia should be evaluated for multiple myeloma.
- The classic diagnostic triad for multiple myeloma consists of bone marrow plasmacytosis (>10% infiltration), osteolytic bone lesions, and M proteins in blood or urine.
Introduction to Multiple Myeloma
- Multiple myeloma is a clonal plasma cell proliferative disorder.
- It is characterized by an abnormal increase of monoclonal paraprotein.
- This increase leads to specific end-organ damage.
Epidemiology
- It is most frequently diagnosed in 65-74 year olds.
- African Americans are twice as likely to be diagnosed with multiple myeloma.
- Men are 1.5 times more likely to be diagnosed with multiple myeloma.
Pathogenesis
- Myeloma cells lead to the production of monoclonal protein causing hyperviscosity and neuropathy and coagulation defects due to amyloid deposition.
- Myeloma cells also cause decreased immunoglobulins and neutropenia leading to infections.
- They can cause bone marrow infiltration and subsequent bone destruction.
- This leads to hypercalcemia, renal failure, and anemia.
Disease Characteristics
- As plasma cell clones become more aggressive, the number of BM plasma cells and circulating myeloma protein increase.
- This leads to end-organ damage, such as anemia, renal insufficiency, hypercalcemia, and increased risk of infections.
- Bone lesions are osteolytic and can be seen on skeletal radiography.
- Extramedullary disease involves other organs like the skin and liver.
Clinical Presentation
- Anemia is due to bone marrow infiltration and renal failure (decreased EPO level).
- Bone pain results from increased osteoclast activity causing lytic bone lesions and pathological fractures.
- Plasmacytoma (collection of plasma cells outside the bone marrow) contributes to bone pain.
- Hypercalcemia is due to increased bone destruction.
- Renal failure is due to hypercalcemia, drug-induced causes (NSAIDs), and plasma cell infiltration in the kidney.
- Spinal cord compression can be due to plasmacytoma or pathological fractures.
- Recurrent infections are due to hypogammaglobulinemia.
- Hyperviscosity occurs due to high levels of plasma cells.
Alternate Diagnosis
- Hypercalcemia can be caused by hyperparathyroidism, thyrotoxicosis, or drugs.
- Renal failure can be caused by diabetic nephropathy or hypertension.
- Anemia can be caused by anemia of chronic illness or nutritional deficiency.
- Bone pain can be caused by osteoporosis or primary bone cancer.
Clinical Features
- Hypercalcemia is present in 13% at diagnosis.
- Increased osteoclastic bone resorption and increased renal tubular calcium reabsorption are the causes.
- Renal failure is present in 19% at diagnosis.
- Light chain cast nephropathy, hypercalcemia, monoclonal immunoglobulin deposition disease, plasma cell infiltration of the kidneys, concurrent amyloidosis, and drug-induced causes are renal failure etiologies.
- Anemia is present in 35% at diagnosis.
- Bone marrow infiltration by plasma cells, cytokine-mediated suppression of erythropoiesis, and renal failure contribute to anemia.
- Bone pain is present in 58% at diagnosis.
- Increased osteoclast activity causing lytic bone lesions, osteoporosis, and pathological fractures are causes of bone pain.
- Plasmacytomas affecting the bone also contribute to bone pain.
Other Features
- Spinal cord compression occurs in 5% of patients due to plasmacytomas or pathological fractures.
- Recurrent infections are due to hypogammaglobulinemia and leukopenia.
- Hyperviscosity symptoms are due to high levels of circulating paraprotein.
How to Diagnose
- Complete blood count shows normocytic normochromic anemia.
- Blood chemistry includes renal and liver function tests, ESR, LDH, and serum calcium.
- Quantitative immunoglobulin assay measures Ig G, Ig A, Ig M levels.
- Serum protein electrophoresis detects paraproteins (M proteins) in the blood.
- Serum free light chain assay and serum B2 microglobulin are performed.
- A urine test is conducted.
- Bone marrow evaluation is required at diagnosis, to evaluate response, and at the time of relapse.
- Radiology with X-rays, PET, MRI, CT scans, which may not be performed in all cases, can help to detect complications associated with multiple myeloma and determine if cancer has spread.
Diagnostic Criteria for MM
- ≥ 10% BM plasma cells or biopsy-proven bony or extramedullary plasmacytoma and ≥ 1 MDE (CRAB or biomarkers of malignancy)
- Biomarkers of malignancy include >1 focal lesion (25 mm in size), ≥60% plasma cells on BM examination and Serum involved/uninvolved FLC ratio ≥100 (involved FLC must be ≥100 mg/L)
CRAB Criteria
- Hypercalcemia: Serum calcium >0.25 mmol/L higher than the upper limits of normal, or >2.75 mmol/L
- Renal Insufficiency: Serum creatinine >177 µmol/L or <0.67 mL/s creatinine clearance
- Anemia: Hemoglobin <100 g/L or hemoglobin >20 g/L below the lower limit of normal
- Bone lesions: ≥1 osteolytic lesion on skeletal radiography, CT, or PET-CT
- Factors affecting treatment options include age, cost, comorbidities, disease complications (renal failure) and risk stratification.
Treatment of Multiple Myeloma
- Supportive care includes hydration and diuretics for hypercalcemia.
- Blood transfusion and erythropoietin are done for symptomatic anemia and adequate hydration, and treating hypercalcemia and avoid nephrotoxic drugs are done for renal impairment.
- Bisphosphonates for bone lytic lesions, analgesia for bone pain, antibiotics for infections, and plasmapheresis for hyperviscosity are done.
- Specific treatment includes chemotherapy (alkylating agents), targeted therapy (immunomodulatory drugs), monoclonal antibodies (anti-CD38), and autologous stem cell transplantation.
Lecture Notes - Epidemiology
- Elderly (mean age 65-70 years).
- Men > Women.
- Family History = 4-fold increased risk.
Prognostic Investigations
- Serum albumin: hypoalbuminaemia correlates with poor prognosis.
- LDH: tumor burden (prognostic).
- B2 microglobulin: tumor burden.
- C-reactive protein (CRP): tumor aggression.
Staging
- Criteria are based on Sr B2-M and Sr albumin levels.
Poor Prognostic Factors
- Age > 60 years.
- Anemia.
- Low serum albumin.
- High B2 microglobulin.
- Raised LDH.
- Poor general condition.
- Poor cytogenetics.
- Poor response to therapy.
Treatment - Supportive
- Bone pain: Analgesics and Stabilization by surgical fixation.
- Pathological fracture: Radiotherapy and Bisphosphonate.
- Anemia: Packed RBC's transfusion, Erythropoietin, and Supportive care.
Treatment
- Infection: IVIG, Antibiotics and antifungal.
- Hypercalcemia: Adequate hydration, Calcitonin, Corticosteroids, Bisphosphonate.
- Renal impairment: Adequate hydration & avoid nephrotoxic drugs. Treatment of hypercalcemia, hyperuricemia and infections.
- Hyper viscosity: Plasmapheresis + chemotherapy.
Treatment - Specific
- Melphalan /steroid: for elderly patients unfit for chemotherapy.
- Immunomodulators: Thalidomide.
- Proteasome inhibitors: Bortezomib.
- Monoclonal antibodies: anti CD38 (daratumumab).
- Auto stem cell transplant.
- VAD is no longer the gold-standard induction regimen.
Multiple Myeloma Diagnostic Criteria
- Clonal bone marrow plasma cells or plasmacytoma.
- Presence of serum and/or urinary monoclonal protein (except in patients with true non-secretory multiple myeloma).
- Evidence of end-organ damage attributed to the plasma cell disorder.
CRAB
- Hypercalcemia: ≥ 11 mg/L or upper limit of normal
- Renal Insufficiency: creatinine (> 2 mg/dl)
- Anemia: with Hb value of > 2 g/dl below the lower limit of normal or Hb value <10 g/dl.
- Bone lesions: lytic lesions, severe osteopenia or pathologic fractures.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.