Podcast
Questions and Answers
What is the primary characteristic of serous inflammation?
What is the primary characteristic of serous inflammation?
- Formation of an ulcer on the surface of an organ or tissue
- Outpouring of a thin fluid derived from plasma or mesothelial cells (correct)
- Deposition of fibrin in the extracellular spaces
- Accumulation of pus in the affected area
What is the term for the accumulation of fluid in serous cavities?
What is the term for the accumulation of fluid in serous cavities?
- Effusion (correct)
- Exudate
- Transudate
- Infiltrate
What is the main component of fibrinous exudate in fibrinous inflammation?
What is the main component of fibrinous exudate in fibrinous inflammation?
- Fibrin (correct)
- Lymphocytes
- Eosinophils
- Neutrophils
What is the primary cause of suppurative inflammation?
What is the primary cause of suppurative inflammation?
What is the term for a localized collection of purulent inflammatory exudate?
What is the term for a localized collection of purulent inflammatory exudate?
What is the characteristic of an ulcer?
What is the characteristic of an ulcer?
Which of the following is a common site for ulcer formation?
Which of the following is a common site for ulcer formation?
What is the term for the shedding of inflammatory necrotic tissue?
What is the term for the shedding of inflammatory necrotic tissue?
What is the primary difference between serous and fibrinous inflammation?
What is the primary difference between serous and fibrinous inflammation?
What is the term for the inflammatory response characterized by the production of large amounts of pus?
What is the term for the inflammatory response characterized by the production of large amounts of pus?
What is the most common cause of chronic inflammation?
What is the most common cause of chronic inflammation?
What is the characteristic feature of chronic inflammation in the lung?
What is the characteristic feature of chronic inflammation in the lung?
What is the function of CD4+ T lymphocytes in inflammation?
What is the function of CD4+ T lymphocytes in inflammation?
What is the outcome of acute inflammation that leads to tissue destruction?
What is the outcome of acute inflammation that leads to tissue destruction?
What type of cells are commonly seen in chronic inflammation?
What type of cells are commonly seen in chronic inflammation?
What is the role of B lymphocytes in the adaptive immune response?
What is the role of B lymphocytes in the adaptive immune response?
What is the name of the macrophages found in the liver?
What is the name of the macrophages found in the liver?
What is the definition of chronic inflammation?
What is the definition of chronic inflammation?
What is the outcome of acute inflammation that leads to the formation of a cavity?
What is the outcome of acute inflammation that leads to the formation of a cavity?
What is the name of the process by which new blood vessels are formed in chronic inflammation?
What is the name of the process by which new blood vessels are formed in chronic inflammation?
Flashcards are hidden until you start studying
Study Notes
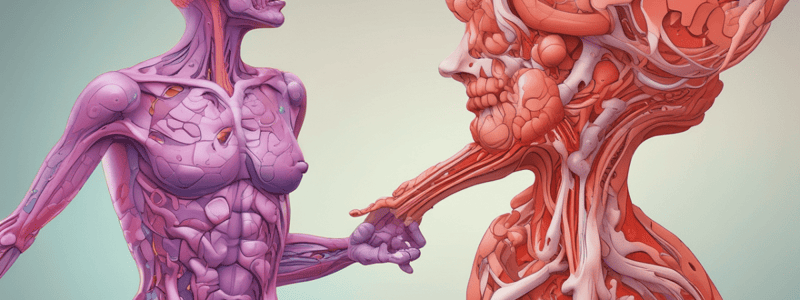
Morphological Patterns of Acute Inflammation
- Serous inflammation: characterized by outpouring of thin fluid derived from plasma or mesothelial cells lining serous cavities, leading to accumulation of fluid in these cavities (effusion), e.g., skin blisters.
Types of Acute Inflammation
- Fibrinous inflammation: characterized by deposition of fibrin in extracellular spaces, often occurring in cases of severe injuries with high vascular permeability, e.g., fibrinous exudate in meninges, pericardium, and pleura.
- Purulent inflammation: characterized by production of large amounts of pus (purulent exudate), consisting of neutrophils, liquefactive necrosis, and edema fluid, often caused by pyogenic bacteria, leading to abscess formation.
- Ulcer: a local defect or excavation of the surface of an organ or tissue produced by sloughing of inflammatory necrotic tissue, often occurring at sites of mucosa, skin, and subcutaneous tissues.
Outcome of Acute Inflammation
- Complete resolution with regeneration of native cells and restoration of the site to normal.
- Abscess formation, often in infections with pyogenic organisms.
- Healing by connective tissue replacement (fibrosis) and scarring, occurring after substantial tissue destruction or when inflammation occurs in tissues that do not regenerate.
- Progression to chronic inflammation.
Chronic Inflammation
- Definition: inflammation of prolonged duration (weeks to years), characterized by simultaneous inflammation, tissue injury, and healing, often by fibrosis.
- Causes: persistent infection, prolonged exposure to toxic agents, hypersensitivity diseases, immune-mediated inflammatory diseases, and chronic inflammation following acute inflammation.
- Morphologic features: infiltration with mononuclear cells, tissue destruction or necrosis, and attempts at healing by connective tissue replacement.
Cells in Chronic Inflammation
- Macrophages: play a crucial role in chronic inflammation, can be activated and differentiated into various forms, e.g., Kupffer cells (liver), microglial cells (CNS), alveolar macrophages (lung).
- Lymphocytes: major drivers of inflammation in autoimmune and chronic inflammatory diseases, activation of B and T lymphocytes is part of the adaptive immune response, and subsets of CD4+ T lymphocytes (TH1, TH2, TH17) secrete different cytokines and elicit different types of inflammation.
- Interaction between lymphocytes and macrophages in chronic inflammation is bidirectional and reciprocal, with both cells having a unique relationship.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.