Podcast
Questions and Answers
Which of the following is NOT a clinical manifestation associated with Helicobacter pylori?
Which of the following is NOT a clinical manifestation associated with Helicobacter pylori?
- Bacteremia (correct)
- GERD
- Gastritis
- Peptic ulcer disease
What is a component of the first-line quadruple therapy for Helicobacter pylori treatment?
What is a component of the first-line quadruple therapy for Helicobacter pylori treatment?
- Azithromycin
- Ciprofloxacin
- Doxycycline
- Clarithromycin (correct)
Which of the following characteristics is associated with Vibrio species?
Which of the following characteristics is associated with Vibrio species?
- Anaerobic growth only
- Gram-positive cocci
- Facultative anaerobes (correct)
- Lactose non-fermenting
What type of agar is used for the growth of Vibrio species?
What type of agar is used for the growth of Vibrio species?
What condition is associated with Vibrio vulnificus?
What condition is associated with Vibrio vulnificus?
What is the role of the tests used for identifying Enterobacteriaceae?
What is the role of the tests used for identifying Enterobacteriaceae?
Which of the following bacteria is a lactose non-fermenter present in the Enterobacteriaceae family?
Which of the following bacteria is a lactose non-fermenter present in the Enterobacteriaceae family?
What characteristic makes Enteroinvasive E. coli (EIEC) distinct among other E. coli pathotypes?
What characteristic makes Enteroinvasive E. coli (EIEC) distinct among other E. coli pathotypes?
Which of the following can be concluded about Escherichia coli regarding UTI?
Which of the following can be concluded about Escherichia coli regarding UTI?
What is the mechanism by which Enterotoxogenic E. coli (ETEC) causes diarrhea?
What is the mechanism by which Enterotoxogenic E. coli (ETEC) causes diarrhea?
What is the primary type of infection caused by typable Haemophilus influenzae (Hib)?
What is the primary type of infection caused by typable Haemophilus influenzae (Hib)?
Which of the following properties correctly describes Campylobacter jejuni?
Which of the following properties correctly describes Campylobacter jejuni?
What type of vaccine is used to prevent infections caused by Haemophilus influenzae type b?
What type of vaccine is used to prevent infections caused by Haemophilus influenzae type b?
Which test is NOT commonly used to diagnose Haemophilus influenzae infections?
Which test is NOT commonly used to diagnose Haemophilus influenzae infections?
What is the recommended dose schedule for the DTaP vaccine?
What is the recommended dose schedule for the DTaP vaccine?
What is the primary mechanism by which Neisseria meningitidis evades the immune system?
What is the primary mechanism by which Neisseria meningitidis evades the immune system?
Neisseria gonorrhoeae is most symptomatic in which percentage of males?
Neisseria gonorrhoeae is most symptomatic in which percentage of males?
Which feature is used to uniquely identify Neisseria meningitidis from Neisseria gonorrhoeae?
Which feature is used to uniquely identify Neisseria meningitidis from Neisseria gonorrhoeae?
What is the most common clinical sign of meningitis caused by Neisseria meningitidis?
What is the most common clinical sign of meningitis caused by Neisseria meningitidis?
Which of the following treatments is typically used for Neisseria gonorrhoeae infections?
Which of the following treatments is typically used for Neisseria gonorrhoeae infections?
What type of agar is used for culturing Neisseria meningitidis?
What type of agar is used for culturing Neisseria meningitidis?
Which of the following complications is associated with Neisseria meningitidis infections?
Which of the following complications is associated with Neisseria meningitidis infections?
What is a key characteristic of Neisseria gonorrhoeae in terms of its pathogenicity?
What is a key characteristic of Neisseria gonorrhoeae in terms of its pathogenicity?
Which serotype of Neisseria meningitidis is the most common and least immunogenic?
Which serotype of Neisseria meningitidis is the most common and least immunogenic?
How do respiratory droplets relate to the transmission of Neisseria meningitidis?
How do respiratory droplets relate to the transmission of Neisseria meningitidis?
Which organism is a major cause of neonatal meningitis?
Which organism is a major cause of neonatal meningitis?
What characteristic is associated with Klebsiella pneumoniae?
What characteristic is associated with Klebsiella pneumoniae?
Which pathogen is particularly associated with nosocomial UTIs and catheter septicemia?
Which pathogen is particularly associated with nosocomial UTIs and catheter septicemia?
What is a key virulence factor of Proteus spp.?
What is a key virulence factor of Proteus spp.?
Which statement is true regarding Serratia marcescens?
Which statement is true regarding Serratia marcescens?
Which condition is NOT commonly associated with Klebsiella pneumoniae?
Which condition is NOT commonly associated with Klebsiella pneumoniae?
What type of infections is Proteus vulgaris most commonly associated with?
What type of infections is Proteus vulgaris most commonly associated with?
Which characteristic differentiates P. mirabilis from P. vulgaris?
Which characteristic differentiates P. mirabilis from P. vulgaris?
What type of toxin does Vibrio cholerae produce that leads to watery diarrhea?
What type of toxin does Vibrio cholerae produce that leads to watery diarrhea?
Which serotypes of Vibrio cholerae are primarily associated with epidemics?
Which serotypes of Vibrio cholerae are primarily associated with epidemics?
What clinical manifestation is characteristic of cholera?
What clinical manifestation is characteristic of cholera?
Which of the following statements about the Enterobacteriaceae family is true?
Which of the following statements about the Enterobacteriaceae family is true?
What is the primary treatment for cholera infection?
What is the primary treatment for cholera infection?
What is the shape of bacteria belonging to the Enterobacteriaceae family?
What is the shape of bacteria belonging to the Enterobacteriaceae family?
What indicates a significant loss of potassium in a cholera patient?
What indicates a significant loss of potassium in a cholera patient?
Which of the following bacteria within the Enterobacteriaceae family is known to be non-motile?
Which of the following bacteria within the Enterobacteriaceae family is known to be non-motile?
What does the Vi antigen refer to in Salmonella enterica?
What does the Vi antigen refer to in Salmonella enterica?
What does the Enteropluri® Tube specifically identify?
What does the Enteropluri® Tube specifically identify?
Flashcards
Helicobacter pylori
Helicobacter pylori
A type of bacteria that causes gastritis and peptic ulcers, not associated with bacteremia.
Quadruple Therapy
Quadruple Therapy
A common treatment for Helicobacter pylori infection, consisting of a proton pump inhibitor, an antibiotic (Clarithromycin or Amoxicillin), a bismuth compound, and sometimes Tetracycline and Metronidazole if resistance is present.
Vibrionaceae
Vibrionaceae
A group of bacteria that includes Vibrio cholerae, Vibrio vulnificus, and Vibrio parahaemolyticus.
Vibrio vulnificus
Vibrio vulnificus
Signup and view all the flashcards
Vibrio parahaemolyticus
Vibrio parahaemolyticus
Signup and view all the flashcards
Neisseria meningitidis
Neisseria meningitidis
Signup and view all the flashcards
Meningitis
Meningitis
Signup and view all the flashcards
Capsule
Capsule
Signup and view all the flashcards
Antiphagocytic
Antiphagocytic
Signup and view all the flashcards
Capnophillic
Capnophillic
Signup and view all the flashcards
Metabolism
Metabolism
Signup and view all the flashcards
Pili
Pili
Signup and view all the flashcards
IgA protease
IgA protease
Signup and view all the flashcards
Neisseria gonorrhoeae
Neisseria gonorrhoeae
Signup and view all the flashcards
Urethritis (Males) / Endocervicities (Females)
Urethritis (Males) / Endocervicities (Females)
Signup and view all the flashcards
What is DTaP?
What is DTaP?
Signup and view all the flashcards
What is Hib?
What is Hib?
Signup and view all the flashcards
How does Hib infect the body?
How does Hib infect the body?
Signup and view all the flashcards
What are the characteristics of Hib's survival?
What are the characteristics of Hib's survival?
Signup and view all the flashcards
What is Campylobacter jejuni?
What is Campylobacter jejuni?
Signup and view all the flashcards
Vibrio cholerae
Vibrio cholerae
Signup and view all the flashcards
Cholera toxin
Cholera toxin
Signup and view all the flashcards
Cholera
Cholera
Signup and view all the flashcards
Cholera pathogenesis
Cholera pathogenesis
Signup and view all the flashcards
Enterobacteriaceae
Enterobacteriaceae
Signup and view all the flashcards
Facultative anaerobes
Facultative anaerobes
Signup and view all the flashcards
Oxidase test
Oxidase test
Signup and view all the flashcards
Vi antigen
Vi antigen
Signup and view all the flashcards
Enteropluri ® Tube
Enteropluri ® Tube
Signup and view all the flashcards
O antigen
O antigen
Signup and view all the flashcards
Enterotube Test
Enterotube Test
Signup and view all the flashcards
MacConkey Agar
MacConkey Agar
Signup and view all the flashcards
Escherichia coli
Escherichia coli
Signup and view all the flashcards
Enterotoxogenic E. coli (ETEC)
Enterotoxogenic E. coli (ETEC)
Signup and view all the flashcards
Enteroinvasive E. coli (EIEC)
Enteroinvasive E. coli (EIEC)
Signup and view all the flashcards
Neonatal Meningitis: E. coli
Neonatal Meningitis: E. coli
Signup and view all the flashcards
Klebsiella pneumoniae: Key Features
Klebsiella pneumoniae: Key Features
Signup and view all the flashcards
Klebsiella Pneumonia: Clinical Manifestations
Klebsiella Pneumonia: Clinical Manifestations
Signup and view all the flashcards
Serratia marcescens: Identification & Infections
Serratia marcescens: Identification & Infections
Signup and view all the flashcards
Proteus spp.: General Properties
Proteus spp.: General Properties
Signup and view all the flashcards
Proteus spp.: Indole Production
Proteus spp.: Indole Production
Signup and view all the flashcards
Proteus mirabilis: Common Infection
Proteus mirabilis: Common Infection
Signup and view all the flashcards
Proteus spp.: Clinical Significance
Proteus spp.: Clinical Significance
Signup and view all the flashcards
Study Notes
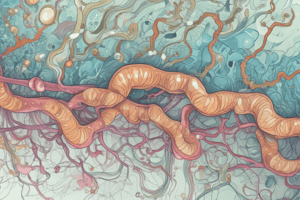
Medically Important Gram-Negative Bacteria
- These bacteria are a diverse group, crucial in various medical contexts.
- Learning objectives focus on key characteristics, diseases, and virulence factors.
- Neisseria spp. and Moraxella spp. exhibit distinct morphologies, features, and common diseases, also outlining their key virulence factors.
- Enterobacteriaceae family members are noted for their differing oxidase and lactose fermentation tests, distinguishing opportunistic from primary pathogens and serological classification (O, H, and K antigens).
- Gram-negative organisms like Pseudomonas aeruginosa, Burkholderia cepacia, Acinetobacter baumannii, Vibrio spp., Campylobacter spp., Helicobacter pylori, Haemophilus spp., and Bordetella pertussis each possess specific morphologies, virulence factors, and related illnesses.
- These organisms' features and classifications are covered in Murray's Medical Microbiology (9th edition), specifically chapters 23 through 29.
Gram (+ve) and Gram (-ve) Bacteria
- Gram-positive bacteria have a thick peptidoglycan layer, while gram-negative bacteria have a thin peptidoglycan layer.
- Their contrasting structures affect how antibiotics affect them, leading to differential susceptibility.
- Gram-positive cell walls contain lipoteichoic acid and are sensitive to certain antibiotics.
- Gram-negative cell walls contain lipopolysaccharides (endotoxins), endotoxins are released when the bacteria die, leading to inflammation and possible shock.
Neisseria species
- Bean-shaped gram-negative diplococci (pairs).
- Non-spore-forming, intracellular pathogens.
- Aerobic, requiring carbon dioxide for optimal growth.
- Most are oxidase and catalase positive.
- All metabolize glucose, but only N. meningitidis metabolizes specifically maltose.
- Neisseria species grow on modified Thayer Martin Agar.
Neisseria meningitidis
- Second most common cause of community-acquired meningitis.
- Transmitted via respiratory droplets.
- Encapsulated, capnophilic (5% CO2).
- Metabolizes glucose and maltose.
- A significant percentage of humans carry it in their nasopharynx.
- Key virulence factors include a polysaccharide capsule and pili for attachment.
Virulence and Pathogenesis of N. meningitidis
- Polysaccharide capsule: Antiphagocytic, protecting the bacteria from attack.
- Various serotypes (A, C, W-135, Y, B). Serotype B is most common and least immunogenic.
- Pili: Attachment to respiratory epithelium.
- IgA protease: Colonization of mucosal membranes.
- Lipooligosaccharide (LOS) endotoxin: Fever, shock.
- Complement deficiency (C6-C9): Increased risk of Nisseria infections.
Clinical Signs and Manifestations of N. meningitidis
- Meningitis: Fever, headache, and stiff neck ("nuchal rigidity").
- Vomiting is a common symptom.
- Complications: Septicemia (Waterhouse-Friderichsen syndrome), Adrenal insufficiency, and Intravascular coagulation.
- Diagnosis using Gram stain and culture, or possibly rapid PCR of CSF.
Neisseria gonorrhoeae
- Gram-negative diplococci
- Intracellular pathogen
- Does not metabolize maltose
- Fastidious
- Symptomatic in 90% of males and 50% of females.
- More prevalent in southern U.S. states.
- Infections are frequently underreported.
- Key virulence factors are pili for attachment and IgA protease to degrade the immune response.
Virulence and Pathogenesis of N. gonorrhoeae
- Pili: Attachment, antigenic variation.
- Outer membrane proteins: Antigenic variation.
- Lipo-oligosaccharide (LOS): Modified endotoxin.
- IgA protease: Hydrolyzes secretory IgA.
- Invades mucosal surfaces.
Clinical Signs and Manifestations of N. gonorrhoeae
- Males: Urethritis with dysuria (painful urination) and purulent discharge.
- Females: Endocervicitis, salpingitis, and possible rectal infections in homosexual males.
- Some patients with conjunctivitis.
- Diagnosis: NAAT (Nucleic Acid Amplification Test) and culture.
- Treatment: Ceftriaxone (IM) and Azithromycin (oral).
Gram-Negative Bacilli
- Diverse group of gram-negative rod-shaped bacteria.
- Key classifications: non-enteric and enteric.
- Pseudomonas aeruginosa, Burkholderia cepacia, and Bordetella pertussis are significant non-enteric varieties.
- Haemophilus influenzae and Yersinia pestis are facultative anaerobes, important non-enteric bacilli. Specific pathogens are noted as aerobic and facultative anaerobes respectively.
Pseudomonas aeruginosa
- Ubiquitous, water-inhabiting gram-negative rod with a flagellum.
- Frequent in hospital environments.
- Strict aerobe, opportunistic.
- Common in cystic fibrosis (CF) patients, leading to pneumonia.
- Resistant to multiple antibiotics.
- Some factors leading to tissue damage (phospholipase C and Exotoxin A) are discussed.
Acinetobacter baumannii
- Gram-negative, aerobic rods.
- Common environmental organisms (soil, water, skin), commonly isolated from patients in hospitals.
- Rarely causes disease in healthy individuals, but strains in hospital settings are highly drug-resistant.
- Can cause multiple infections (Respiratory tract infections, Urinary tract infections, Wound infections, Septicemia)
Burkholderia cepacia
- Gram-negative rod.
- Can be found in water, soil, and hospital environments.
- Opportunistic organism, frequently associated with respiratory infections, particularly in individuals with cystic fibrosis.
- Can spread via person-to-person contact, contact with contaminated surfaces, or exposure to Burkholderia in the environment.
- Many strains are antibiotic-resistant, posing clinical challenges.
Bordetella pertussis
- Human-specific pathogen.
- Highly contagious (person-to-person).
- Non-motile, encapsulated gram-negative coccobacillus.
- Fastidious, requiring specialized media (Bordet-Gengou or Regan-Lowe agar) for growth.
- Associated with lymphocytosis – increased levels of white blood cells, and toxins (Adenylate cyclase toxin and Pertussis toxin).
Virulence and Pathogenesis of Bordetella pertussis
- Polysaccharide capsule: Antiphagocytic.
- Adenylate cyclase toxin: Inhibits phagocytosis.
- Tracheal cytotoxin: Destroys ciliated epithelial cells, and induces apoptosis and potentially dermonecrotic lesions.
- Pertussis toxin (PT): Increases cAMP levels.
- Filamentous hemagglutinins (FHA): Bacterial attachment.
Clinical Signs and Manifestations of Bordetella pertussis
- Whooping cough, a specific paroxysmal cough, with periods of intense coughing.
- Other symptoms include fever, headache, sneezing, and anorexia.
Management of Bordetella pertussis
- Vaccination is the primary method of prevention.
- Diphtheria, tetanus, and pertussis vaccines (DTaP) are given in childhood.
- Tdap vaccines are recommended for adolescents and adults.
Haemophilus influenzae
- Gram-negative, pleomorphic (varying shape) coccobacilli
- Strict human pathogen, typically found in the nasopharynx.
- Facultative anaerobe
Campylobacter jejuni
- Gram-negative curved, rodshaped organism.
- Motile (polar flagellum), microaerophilic (needs a lower oxygen concentration).
- Common cause of bacterial diarrhea.
- Often associated with undercooked poultry.
- Virulence factors include adherence factors (that contribute to mucosal attachment), some O-antigens can cross react and result in demyelination.
Helicobacter pylori
- Gram-negative, microaerophilic, spiral-shaped bacterium.
- Motile (flagella)
- Lactose non-fermenter.
- Urease positive
- Common cause of gastritis and peptic ulcers.
- Can potentially lead to chronic/life-long infection if untreated.
- Key virulence factors include urease, vacA, and type IV secretion system which neutralize gastric acid and facilitate mucosal colonization & attachment.
Clinical Signs and Manifestations of Helicobacter pylori
- H. pylori is associated with various digestive problems.
- These include gastritis (inflammation of the stomach lining), peptic ulcers, and potentially gastric adenocarcinoma.
Vibrio cholerae
- Gram-negative, curved rods.
- Facultative anaerobes.
- Single polar flagellum.
- Oxidase positive
- Human reservoir (colon)
- Outbreaks associated with contaminated water.
- 6 serotypes; only 01 & 0139 related to epidemics.
Virulence and Pathogenesis of Vibrio cholerae
- Heat-labile enterotoxin (composed of 6 subunits): ADP-ribosylation of G proteins, leading to increased cAMP levels, resulting in loss of water and electrolytes.
Escherichia coli
- Gram-negative, facultative enteric rods.
- Most common cause of UTIs and normal intestinal flora.
- Motile (some strains).
- Doesn't produce H2S, urease -, citrate - and indole + and lactose+. -Numerous pathotypes exist, including enteropathogenic E. coli (EPEC), enterotoxigenic E. coli (ETEC), enterohemorrhagic E. coli (EHEC), and uropathogenic E. coli (UPEC).
- Different types are associated with certain diseases (like EHEC causing hemorrhagic colitis and UPEC related to urinary tract infections).
Klebsiella pneumoniae
- Gram-negative encapsulated, non-motile rods.
- Lactose fermenter.
- Common GIT pathogen.
- Frequent nosocomial infection (hospital acquired infection).
- Patients with medical devices and/or underlying illnesses have a higher risk of infection.
- Significant antibiotic resistance (extended-spectrum beta-lactamases, fluoroquinolones, and aminoglycosides, and carbapenems).
Serratia marcescens
- Gram-negative, motile rods.
- Opportunistic pathogen.
- Lactose fermenter; produces red pigments, (such as prodigiosin).
- Associated with nosocomial infections, catheter-related septicemia, and burn infections.
- Drug resistance is increasing; antibiotic treatment success is decreasing.
Proteus spp.
- Gram-negative rods.
- Urease positive, lactose non fermenters.
- Produce hydrogen sulfide (H₂S).
- Important in Struvite stone formation.
- Commonly found as normal microbiota in the human GI tract.
- P. mirabilis is most common; P. vulgaris are less common, but may be more associated with hospital settings.
Salmonella
- Gram-negative motile rods.
- Lactose nonfermentative.
- H2S production.
- Classification of species and varieties is significant (2500 serotypes).
- Can cause enteritis, typhoid.
- Some serotypes are more commonly associated with gastroenteritis from the consumption of contaminated meals.
Shigella
- Gram-negative, non-motile rods.
- Lactose nonfermenters
- Does not produce H2S.
- Humans are the only reservoir, commonly transmitted via the fecal-oral route.
- Mainly a disease of infants and young children/school aged children.
- Key virulence factors for invasion are the types of toxin and their associated mechanism of action; specifically Shiga toxin and its mechanism of action.
Yersinia enterocolitica
- Gram-negative facultative rods.
- Motile at 25°C, non-motile at 37°C
- Urease +, but does not ferment lactose.
- Usually found in colder climates or contaminated meat, milk.
- Can cause enterocolitis and post-infectious arthritis.
Yersinia pestis
- Gram-negative coccobacilli.
- Non motile
- Facultative intracellular.
- Important zoonotic pathogen (transmitted via fleas.
- Plague is a disease that can occur in bubonic, pneumonic, and septicemic forms.
- Different cycles of infection are detailed, in both wild and domestic situations.
Enterobacteriaceae Identification
- Key tests for identifying members of the Enterobacteriacea family are lactose fermentation, H2S production, motility, and Voges-Proskauer.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.