Podcast
Questions and Answers
Which assessment finding is most indicative of achalasia?
Which assessment finding is most indicative of achalasia?
- Regurgitation of undigested food. (correct)
- Severe abdominal cramping relieved by defecation.
- Frequent, large-volume diarrhea.
- Increased appetite and weight gain.
A patient reports experiencing chest pains and is diagnosed with esophageal spasms. Which medication would be MOST appropriate for managing this condition?
A patient reports experiencing chest pains and is diagnosed with esophageal spasms. Which medication would be MOST appropriate for managing this condition?
- Antacids
- Isosorbide Dinitrate (correct)
- H2 receptor antagonists
- Proton pump inhibitors
A patient with a hiatal hernia is experiencing nighttime heartburn. What instruction should the nurse give?
A patient with a hiatal hernia is experiencing nighttime heartburn. What instruction should the nurse give?
- Elevate the head of the bed to reduce acid reflux. (correct)
- Eat a large meal right before bed to prevent acid reflux.
- Lie flat immediately after eating to aid digestion.
- Take antacids with warm water before bed.
A patient is diagnosed with GERD. What dietary modification is MOST important for the nurse communicate?
A patient is diagnosed with GERD. What dietary modification is MOST important for the nurse communicate?
Which assessment finding would differentiate a gastric ulcer from a duodenal ulcer?
Which assessment finding would differentiate a gastric ulcer from a duodenal ulcer?
A patient with a peptic ulcer is prescribed antibiotics, a proton pump inhibitor, and antacids. What is the most important teaching point for the nurse emphasize?
A patient with a peptic ulcer is prescribed antibiotics, a proton pump inhibitor, and antacids. What is the most important teaching point for the nurse emphasize?
What dietary modifications should patients with Celiac disease adhere to?
What dietary modifications should patients with Celiac disease adhere to?
A patient with Celiac disease reports experiencing fatigue, depression, and migraine headaches. What does the nurse recognize with these manifestations?
A patient with Celiac disease reports experiencing fatigue, depression, and migraine headaches. What does the nurse recognize with these manifestations?
A patient is diagnosed with a mechanical bowel obstruction. Which finding is MOST indicative of this condition?
A patient is diagnosed with a mechanical bowel obstruction. Which finding is MOST indicative of this condition?
A patient with Crohn's disease is scheduled for a barium study of the upper GI tract. The nurse explains that the test is used to detect:
A patient with Crohn's disease is scheduled for a barium study of the upper GI tract. The nurse explains that the test is used to detect:
Flashcards
Dysphagia
Dysphagia
Difficulty swallowing; hallmark sign of disturbances in ingestion.
Achalasia
Achalasia
A rare esophageal disorder causing absent or ineffective peristalsis in the distal esophagus, preventing proper swallowing.
Hiatal Hernia
Hiatal Hernia
The upper part of the stomach pushes through an opening in the diaphragm, and up into the chest
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD)
Signup and view all the flashcards
Gastritis
Gastritis
Signup and view all the flashcards
Peptic Ulcer Disease (PUD)
Peptic Ulcer Disease (PUD)
Signup and view all the flashcards
Celiac Disease
Celiac Disease
Signup and view all the flashcards
Intestinal Obstruction
Intestinal Obstruction
Signup and view all the flashcards
Crohn's Disease
Crohn's Disease
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Study Notes
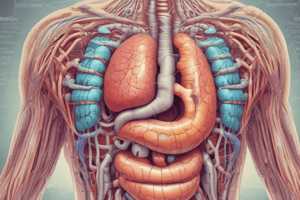
- The provided material contains study notes on medical surgical nursing, focusing on gastrointestinal disorders.
- It's transcribed by Guillergan, M.H.
Module 1 Contents:
- Disturbances in ingestion: achalasia, esophageal spasm, hiatal hernia, diverticulum, gastroesophageal reflux.
- Disturbances in digestion: gastritis, peptic ulcer disease.
- Disturbances in absorption and elimination: celiac disease, intestinal obstruction, Crohn's disease, ulcerative colitis.
Main Functions of GI System
- The main functions of the GI system are ingestion, digestion, absorption, and excretion.
Disturbances in Ingestion: Achalasia
- A rare disorder that may progress slowly.
- It involves a malfunction of the nerves controlling food movement through the esophagus.
- There is absent or ineffective peristalsis in the distal esophagus and failure of the esophageal sphincter to relax during swallowing.
Clinical Manifestations of Achalasia
- Dysphagia (difficulty swallowing) is a hallmark sign.
- Other manifestations are regurgitation, chest discomfort, weight loss, and pyrosis (heartburn).
- The cause is currently unknown.
- Decreased or absent peristalsis occurs in the distal portion of the esophagus.
- The normal swallowing pattern is disrupted.
- The lower esophageal sphincter muscle doesn't relax properly, preventing food passage.
- Diagnostic findings involve endoscopy and esophageal manometry, which is a definitive diagnostic method.
- X-ray studies (esophagram) show esophageal dilation above the lower gastroesophageal sphincter, known as a bird's beak deformity.
- Management is focused on instructing the patient to eat slowly and drink fluids with meals, preferring warm water for vasoconstriction.
- Patients should chew food thoroughly, stay upright while eating, and remain upright for at least one hour after meals.
- Drinking a full glass of water with pills is advised.
- Pharmacological interventions include Isosorbide Dinitrate or Calcium Channel Blockers.
- Isosorbide Dinitrate is an anti-anginal drug used for chest pain (angina) in coronary artery disease patients to relax smooth muscles of esophagus and reduce spasms.
Types of Esophageal Spasm
- Jackhammer esophagus involves hypercontractile esophagus.
- Diffuse esophageal spasm has spasms with normal amplitude.
- Type III achalasia is characterized by lower esophageal sphincter (LES) obstruction.
- Calcium channel blockers (like nifedipine) relax smooth muscles.
- In achalasia, calcium channel blockers reduce pressure in the LES, easing food passage and reducing dysphagia and chest pain.
- They act more as muscle relaxants compared to Isosorbide.
- Botulinum Toxin Injection (Botox) blocks acetylcholine, administered via endoscopy.
- Pneumatic Balloon Dilation stretches the narrowed area of the esophagus, has a high success rate, and requires analgesics or tranquilizers for pain management.
- Surgical option is Laparoscopic Heller Myotomy followed by fundoplication.
Hiatal Hernia
- The upper part of the stomach pushes through a diaphragm opening and into the chest.
- This involves protrusion of the upper part of the stomach.
Types of Hiatal Hernia
- Sliding hiatal hernia (Type 1) involves the junction between the stomach and esophagus sliding up during increased abdominal pressure, returning to normal when pressure is relieved.
- Paraesophageal hiatal hernia involves a portion of the stomach remaining stuck in the chest cavity with no sliding up and down.
- In hiatal hernia, the esophageal hiatus in the diaphragm has a larger opening than normal.
- A portion of the upper stomach slips up or passes through the hiatus and enters into the chest.
- Causes include heavy lifting, hard coughing/sneezing, pregnancy, vomiting, constipation, and obesity.
- Common clinical manifestations include heartburn, regurgitation, dysphagia, and a sense of fullness post-eating.
- Many patients are asymptomatic, with symptoms worsening after meals.
- Assessment and diagnostic findings involve Chest X-ray, Barium Swallow/X-ray, and Upper endoscopy for visualization.
- Management includes frequent, small feedings, advising patients to avoid reclining for 1 hour after eating, and elevating the head of the bed.
- Pharmacologic options include PPIs (taken after meals) and antacids (taken before meals).
- Surgical intervention involves Nissen Fundoplication.
Diverticulum
- Diverticulum is an out-pouching of mucosa and submucosa protruding through a weak portion of the esophagus musculature.
Gastroesophageal Reflux Disease (GERD)
- A common disorder marked by backflow of gastric or duodenal contents into the esophagus, causing troublesome symptoms or mucosal injury.
- It's due to a weak or damaged lower esophageal sphincter (LES).
- Physiologic GERD is postprandial, short-lived, and asymptomatic without nocturnal symptoms, while Pathologic GERD includes symptoms, mucosal injury, and nocturnal symptoms.
- The primary cause involves an incompetent lower esophageal sphincter (LES), as well as aging, and consumption of certain substances.
Clinical Manifestations of GERD
- This includes pyrosis (heartburn), regurgitation, dyspepsia (indigestion), dysphagia or odynophagia, hypersalivation, and dry cough.
- Diagnostic findings include patient history, barium swallow, endoscopy, pH monitoring, and esophageal manometry.
- Management involves educating the patient to avoid situations that cause esophageal irritation through lifestyle modifications, such as diet, limiting alcohol, and avoiding certain foods.
- Elevating the head of the bed and avoiding eating before bed are also helpful.
- For nausea and vomiting, ice chips and antiemetic medications like ondansetron are used.
- Ptyalism is addressed by chewing sugarless gum or hard candy and thorough toothbrushing.
- Dysphagia is managed by flexing the neck, using thickened liquids, and feeding slowly.
- Pharmacologic interventions include antacids, H2 receptor antagonists, and proton pump inhibitors.
- Surgical intervention involves Nissen Fundoplication.
Gastritis
- Gastritis is an inflammation of the gastric mucosa, which can be acute or chronic.
- Acute gastritis, which can be erosive or nonerosive, is commonly caused by local irritants or infection
Clinical Manifestations of Gastritis
- Clinical manifestations: epigastric pain, dyspepsia, anorexia, melena, hematochezia, pyrosis, anemia, and nutrient deficiencies.
- Diagnostic procedures include barium swallow and endoscopy
- Gastric mucosa is capable of repairing itself.
- Medical management includes supportive therapy, but some cases may require emergency surgey
Nursing Management for Gastritis:
- Reducing anxiety
- Promoting optimal nutrition through IV therapy to correct electrolyte imbalances
- Discouraging smoking and caffeinated beverages
- Providing pain relief
Peptic Ulcer Disease (PUD)
- involves excavation in the stomach mucosa that can be caused by H. Pylori infection, NSAID use, smoking, alcohol, or genetics
- Clinical manifestations of peptic ulcers include pain (gastric or duodenal), weight loss, emesis, and dark stool
- diagnostic procedures includes upper endoscopy and a physical examination that finds pain in the epigastric area.
- Medical management consists of PPIs, lifestyle changes, or H2 blockers.
- Nursing considerations for patients with PUDs involved dietary modifications and assessing bowel movements.
- Possible complications are hypovolemic shock and perforation
Celiac Disease
- It results in loss of ability to absorb macro and micronutrients, causing systemic nutritional deficits
- The cause stems from an autoimmune response to products that contain the protein gluten.
- Clinical manifestations are diarrhea or steatorrhea (hallmark sign), abdominal pain and distention, flatulence, weight loss, and non-GI symptoms like fatigue.
- Diagnostic findings are IGA and Anti-Tissue Transglutaminase, as well as upper endoscopy with biopsies from the proximal small intestine.
- Definitive diagnosis is based upon a series of serologic tests and endoscopic biopsy.
- Chronic, non-curable, lifelong disease.
Treatment for Celiac Disease revolves around refraining from gluten
- Focus should be on foods like fresh fruits/vegetables, meat/poultry, fish, dairy, beans/legumes, and rice.
- Foods like rye, bulgar, etc (found in pastries, cakes, pizza etc) caramel colored foods,
- Other manifestations of celiac disease may require specific, targeted treatment.
- Other manifestations of celiac disease may require specific, targeted treatment.
- Anemia can be treated by folate, cobalamin, or iron supplements, while osteopenia treatment is recommended to treat osteoporosis.
- Nursing management : gluten-free foods, promoting optimal nutrition, and relieving pain
Intestinal Obstruction
- Occurs when blockage prevents the normal flow of intestinal contents through the tract, and the obstruction can be partial or complete.
- Severity depends on the region of bowel affected, the degree to which the lumen is occluded, and especially the degree to which the vascular supply to the bowel wall is disturbed.
- Mechanical obstruction happens inside the intestinal lumen
- Functional obstruction is where they intestinal musculature cannot propel
Inflammatory Bowel Disease
- A group of chronic disorders, specifically Crohn's Disease and Ulcerative Colitis
- Causes depend on familial risk, smoking, and altered immune system.
Crohn's Disease
- A subacute and chronic inflammation, there are histopathologic changes characterized by remission and exacerbation
- Develops into small, focal ulcers that are separated by edematous patches
- Interference Of Intestinal Peristalsis Because Of A Constricted Lumen
- Clinical manifestations include RLO pain and diarrhea, anorexia, weight loss, and nutritional deficiencies
Ulcerative Colitis
- of the mucosal and submucosal layers of rectum and colon has an unknown cause
- Characterized by unpredictable periods of remission and exacerbation with bouts of abdominal cramps and bloody or purulent diarrhea
- diagnostic findings include abnormal a-ray, colonoscopy, or albumin levels
- Clinical manifestations include bloody diarrhea (hallmark sign) and intermittent tenesmus
- Has a complication of toxic megacolon.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.