Podcast
Questions and Answers
What is the primary role of the scrotum in the male reproductive system?
What is the primary role of the scrotum in the male reproductive system?
- To produce sperm cells.
- To secrete testosterone.
- To transport sperm to the urethra.
- To maintain optimal temperature for sperm production. (correct)
Which structure stores sperm cells as they mature?
Which structure stores sperm cells as they mature?
- Epididymis (correct)
- Seminal vesicles
- Prostate gland
- Vas deferens
What is the purpose of the fluid produced by the prostate gland?
What is the purpose of the fluid produced by the prostate gland?
- To provide energy for sperm cells.
- To transport sperm to the penis.
- To neutralize the acidity of the vagina. (correct)
- To lubricate the urethra.
Which part of the sperm cell contains enzymes needed to penetrate the egg?
Which part of the sperm cell contains enzymes needed to penetrate the egg?
Which of the following is NOT a function of testosterone in males?
Which of the following is NOT a function of testosterone in males?
What is the role of the seminal vesicles?
What is the role of the seminal vesicles?
Which structure in the female reproductive system is responsible for housing and protecting the fetus during pregnancy?
Which structure in the female reproductive system is responsible for housing and protecting the fetus during pregnancy?
Where does fertilization typically occur in the female reproductive system?
Where does fertilization typically occur in the female reproductive system?
What is the endometrium?
What is the endometrium?
Which hormone primarily stimulates male puberty?
Which hormone primarily stimulates male puberty?
What is the main hormonal driver of female puberty?
What is the main hormonal driver of female puberty?
What event signifies the beginning of fertility in females during puberty?
What event signifies the beginning of fertility in females during puberty?
Which hormone primarily influences spermatogenesis?
Which hormone primarily influences spermatogenesis?
What type of cell division is involved in gametogenesis?
What type of cell division is involved in gametogenesis?
How many chromosomes are present in a human spermatid?
How many chromosomes are present in a human spermatid?
What is the role of FSH in oogenesis?
What is the role of FSH in oogenesis?
During which days of a typical menstrual cycle does menstruation occur?
During which days of a typical menstrual cycle does menstruation occur?
What hormone is secreted by the corpus luteum?
What hormone is secreted by the corpus luteum?
Which hormone triggers ovulation?
Which hormone triggers ovulation?
What happens to the corpus luteum if fertilization does not occur?
What happens to the corpus luteum if fertilization does not occur?
Where does fertilization usually take place?
Where does fertilization usually take place?
What is the morula?
What is the morula?
Approximately how many days after fertilization does the blastocyst implant in the uterus?
Approximately how many days after fertilization does the blastocyst implant in the uterus?
What is the role of chorionic villi?
What is the role of chorionic villi?
When is the developing embryo referred to as a fetus?
When is the developing embryo referred to as a fetus?
On what day of the menstrual cycle does ovulation typically occur?
On what day of the menstrual cycle does ovulation typically occur?
Which blood vessels are found in the umbilical cord?
Which blood vessels are found in the umbilical cord?
What is the gestation period in humans?
What is the gestation period in humans?
What is the primary function of amniotic fluid?
What is the primary function of amniotic fluid?
Which structure directly facilitates the exchange of oxygen and nutrients between the maternal and fetal bloodstreams?
Which structure directly facilitates the exchange of oxygen and nutrients between the maternal and fetal bloodstreams?
A couple is having difficulty conceiving. Medical investigations reveal that the male partner's sperm count is significantly low, and the sperm exhibit poor motility. Which of the following accessory glands is MOST likely to be the source of this issue, considering its role in sperm viability and motility?
A couple is having difficulty conceiving. Medical investigations reveal that the male partner's sperm count is significantly low, and the sperm exhibit poor motility. Which of the following accessory glands is MOST likely to be the source of this issue, considering its role in sperm viability and motility?
A researcher is investigating the effects of a novel drug on spermatogenesis. They observe that the drug significantly reduces the number of mitochondria in the sperm's midpiece without affecting other cellular structures. What is the MOST likely impact of this drug on sperm function?
A researcher is investigating the effects of a novel drug on spermatogenesis. They observe that the drug significantly reduces the number of mitochondria in the sperm's midpiece without affecting other cellular structures. What is the MOST likely impact of this drug on sperm function?
A woman is experiencing irregular menstrual cycles, and her doctor suspects a hormonal imbalance. Blood tests reveal consistently low levels of luteinizing hormone (LH) throughout her cycle. Which phase of the menstrual cycle would be MOST directly affected by this hormonal deficiency?
A woman is experiencing irregular menstrual cycles, and her doctor suspects a hormonal imbalance. Blood tests reveal consistently low levels of luteinizing hormone (LH) throughout her cycle. Which phase of the menstrual cycle would be MOST directly affected by this hormonal deficiency?
A fertility clinic is evaluating the developmental competence of embryos created through in vitro fertilization (IVF). During microscopic examination, they observe that several embryos reach the morula stage but fail to transition into blastocysts. Which of the following cellular processes or conditions is MOST likely responsible for this developmental arrest?
A fertility clinic is evaluating the developmental competence of embryos created through in vitro fertilization (IVF). During microscopic examination, they observe that several embryos reach the morula stage but fail to transition into blastocysts. Which of the following cellular processes or conditions is MOST likely responsible for this developmental arrest?
During an ultrasound at 20 weeks gestation, it’s discovered that the fetus has oligohydramnios (i.e. a deficiency in amniotic fluid). Considering the various functions of amniotic fluid, which of the following fetal complications is MOST likely to arise as a direct consequence of this condition?
During an ultrasound at 20 weeks gestation, it’s discovered that the fetus has oligohydramnios (i.e. a deficiency in amniotic fluid). Considering the various functions of amniotic fluid, which of the following fetal complications is MOST likely to arise as a direct consequence of this condition?
A researcher is studying a population with a high incidence of male infertility. They discover a genetic mutation that affects the production of inhibin by Sertoli cells in the testes. How would this mutation MOST likely impact male reproductive function?
A researcher is studying a population with a high incidence of male infertility. They discover a genetic mutation that affects the production of inhibin by Sertoli cells in the testes. How would this mutation MOST likely impact male reproductive function?
A scientist develops a drug that selectively blocks the action of acrosin, one of the key enzymes found in the acrosome of sperm cells. What specific step in fertilization would be MOST directly inhibited by this drug?
A scientist develops a drug that selectively blocks the action of acrosin, one of the key enzymes found in the acrosome of sperm cells. What specific step in fertilization would be MOST directly inhibited by this drug?
Which of the following structures is directly responsible for maintaining the testes at a temperature suitable for sperm production?
Which of the following structures is directly responsible for maintaining the testes at a temperature suitable for sperm production?
What is the primary function of the vas deferens?
What is the primary function of the vas deferens?
Which gland produces a mucus-like fluid that lubricates the urethra and neutralizes acidic urine?
Which gland produces a mucus-like fluid that lubricates the urethra and neutralizes acidic urine?
What is the role of the acrosome in a sperm cell?
What is the role of the acrosome in a sperm cell?
Which of the following components of sperm provides the energy required for its motility?
Which of the following components of sperm provides the energy required for its motility?
What is the primary function of the ovaries?
What is the primary function of the ovaries?
Which structure serves as the birth canal during childbirth?
Which structure serves as the birth canal during childbirth?
What type of cells line the fallopian tubes to aid in the movement of the egg towards the uterus?
What type of cells line the fallopian tubes to aid in the movement of the egg towards the uterus?
What is the function of the vulva?
What is the function of the vulva?
What hormonal change initiates the onset of male puberty?
What hormonal change initiates the onset of male puberty?
Which of the following secondary sexual characteristics is stimulated by testosterone in males?
Which of the following secondary sexual characteristics is stimulated by testosterone in males?
What event marks the beginning of fertility in females during puberty?
What event marks the beginning of fertility in females during puberty?
Which hormone primarily drives the physical changes associated with female puberty?
Which hormone primarily drives the physical changes associated with female puberty?
Where does spermatogenesis occur?
Where does spermatogenesis occur?
What is the end result of meiosis during spermatogenesis?
What is the end result of meiosis during spermatogenesis?
Which part of the sperm cell contains 22 autosomes and one sex chromosome?
Which part of the sperm cell contains 22 autosomes and one sex chromosome?
How many functional ova typically result from one oogenesis event?
How many functional ova typically result from one oogenesis event?
What structure provides support and protection to the egg during the early stages after fertilization?
What structure provides support and protection to the egg during the early stages after fertilization?
During which phase of the ovarian cycle does the Graafian follicle develop?
During which phase of the ovarian cycle does the Graafian follicle develop?
What hormone is secreted by the developing follicles in the ovaries during days 1-7 of the menstrual cycle?
What hormone is secreted by the developing follicles in the ovaries during days 1-7 of the menstrual cycle?
How does oestrogen affect the endometrium during the follicular phase of the menstrual cycle?
How does oestrogen affect the endometrium during the follicular phase of the menstrual cycle?
Which hormone is primarily responsible for preparing the endometrium for implantation during the luteal phase?
Which hormone is primarily responsible for preparing the endometrium for implantation during the luteal phase?
What event results directly from a peak in luteinizing hormone (LH) levels?
What event results directly from a peak in luteinizing hormone (LH) levels?
What happens to progesterone levels if fertilization does not occur?
What happens to progesterone levels if fertilization does not occur?
Through which structure does the sperm travel after passing through the cervix?
Through which structure does the sperm travel after passing through the cervix?
Mitotic division of the zygote results in the formation of which structure?
Mitotic division of the zygote results in the formation of which structure?
What is the role of enzymes secreted by the blastocyst during implantation?
What is the role of enzymes secreted by the blastocyst during implantation?
What is the main function of the chorionic villi?
What is the main function of the chorionic villi?
At what point in development is the term 'fetus' used?
At what point in development is the term 'fetus' used?
Which of the following is a function of the placenta?
Which of the following is a function of the placenta?
Which structure facilitates the exchange of oxygen and nutrients between the maternal and fetal bloodstreams?
Which structure facilitates the exchange of oxygen and nutrients between the maternal and fetal bloodstreams?
What developmental stage is characterized by the development of the amnion and chorion?
What developmental stage is characterized by the development of the amnion and chorion?
If fertilization does not occur, what event is triggered by the reduction of progesterone levels?
If fertilization does not occur, what event is triggered by the reduction of progesterone levels?
Which of the following is NOT derived from the outer cells of the blastocyst?
Which of the following is NOT derived from the outer cells of the blastocyst?
Which event occurs immediately after ovulation?
Which event occurs immediately after ovulation?
What is the main function of the umbilical vein?
What is the main function of the umbilical vein?
What process occurs approximately on day 14 of the menstrual cycle?
What process occurs approximately on day 14 of the menstrual cycle?
Which of the following correctly matches the structure with its origin?
Which of the following correctly matches the structure with its origin?
Which of the following events is LEAST likely to be directly affected by a significant decrease in progesterone levels during early pregnancy?
Which of the following events is LEAST likely to be directly affected by a significant decrease in progesterone levels during early pregnancy?
Which of the following is an accurate description of the roles and timing of hormonal action during the menstrual cycle?
Which of the following is an accurate description of the roles and timing of hormonal action during the menstrual cycle?
Which of the following is the primary function of the scrotum in the male reproductive system?
Which of the following is the primary function of the scrotum in the male reproductive system?
Where in the male reproductive system are sperm cells stored and allowed to mature?
Where in the male reproductive system are sperm cells stored and allowed to mature?
What is the role of the alkaline fluid produced by the prostate gland?
What is the role of the alkaline fluid produced by the prostate gland?
Which part of a sperm cell contains the genetic material?
Which part of a sperm cell contains the genetic material?
What is the primary function of the seminal vesicles?
What is the primary function of the seminal vesicles?
Which structure in the female reproductive system is the site of fertilization?
Which structure in the female reproductive system is the site of fertilization?
Which hormone primarily stimulates the development of male secondary sexual characteristics during puberty?
Which hormone primarily stimulates the development of male secondary sexual characteristics during puberty?
Which hormone primarily stimulates spermatogenesis?
Which hormone primarily stimulates spermatogenesis?
Where does fertilization usually take place in the female reproductive tract?
Where does fertilization usually take place in the female reproductive tract?
Approximately how many days after fertilization does the blastocyst typically implant in the uterus?
Approximately how many days after fertilization does the blastocyst typically implant in the uterus?
What is the approximate gestation period in humans?
What is the approximate gestation period in humans?
Which cells within the testes are responsible for producing testosterone?
Which cells within the testes are responsible for producing testosterone?
What is the primary role of ciliated columnar epithelium in the fallopian tubes?
What is the primary role of ciliated columnar epithelium in the fallopian tubes?
In spermatogenesis, what is the immediate precursor cell to a mature sperm cell?
In spermatogenesis, what is the immediate precursor cell to a mature sperm cell?
Which phase of the ovarian cycle is characterized by the development of the corpus luteum?
Which phase of the ovarian cycle is characterized by the development of the corpus luteum?
What is the role of the acrosome in sperm function during fertilization?
What is the role of the acrosome in sperm function during fertilization?
Which of the following correctly describes the path sperm take to fertilize an egg?
Which of the following correctly describes the path sperm take to fertilize an egg?
What is the primary function of the vulva?
What is the primary function of the vulva?
Which of the following hormones has a negative feedback effect on FSH secretion during the follicular phase of the menstrual cycle?
Which of the following hormones has a negative feedback effect on FSH secretion during the follicular phase of the menstrual cycle?
A drug that inhibits the action of mitochondria would most directly affect which part of the sperm cell and its function?
A drug that inhibits the action of mitochondria would most directly affect which part of the sperm cell and its function?
If a woman has a consistently short luteal phase in her menstrual cycle, which hormone supplement would be MOST likely prescribed to help maintain a pregnancy?
If a woman has a consistently short luteal phase in her menstrual cycle, which hormone supplement would be MOST likely prescribed to help maintain a pregnancy?
Which of the following events is LEAST directly dependent on the presence of luteinizing hormone (LH)?
Which of the following events is LEAST directly dependent on the presence of luteinizing hormone (LH)?
Consider a scenario where the Cowper's glands are non-functional. Which aspect of male reproductive function would be MOST directly compromised?
Consider a scenario where the Cowper's glands are non-functional. Which aspect of male reproductive function would be MOST directly compromised?
During which stage of development does the process of gastrulation occur, establishing the three primary germ layers?
During which stage of development does the process of gastrulation occur, establishing the three primary germ layers?
If a mutation caused the Sertoli cells to lose their ability to support and nourish developing sperm cells, but Leydig cell function remained normal, what would be the MOST likely outcome?
If a mutation caused the Sertoli cells to lose their ability to support and nourish developing sperm cells, but Leydig cell function remained normal, what would be the MOST likely outcome?
A researcher is studying the impact of a new environmental toxin on reproductive health. They observe that exposure to this toxin leads to a significant decrease in the number of mitochondria in developing spermatids. What is the MOST direct consequence of this mitochondrial damage on sperm function?
A researcher is studying the impact of a new environmental toxin on reproductive health. They observe that exposure to this toxin leads to a significant decrease in the number of mitochondria in developing spermatids. What is the MOST direct consequence of this mitochondrial damage on sperm function?
Flashcards
Testes
Testes
Primary male reproductive organs that produce sperm cells and testosterone.
Scrotum
Scrotum
Skin sac that holds the testes and regulates their temperature.
Epididymis
Epididymis
Coiled tube where sperm mature and are stored.
Vas Deferens (Sperm Duct)
Vas Deferens (Sperm Duct)
Signup and view all the flashcards
Urethra
Urethra
Signup and view all the flashcards
Seminal Vesicles
Seminal Vesicles
Signup and view all the flashcards
Prostate Gland
Prostate Gland
Signup and view all the flashcards
Cowper’s Gland (Bulbourethral Gland)
Cowper’s Gland (Bulbourethral Gland)
Signup and view all the flashcards
Penis
Penis
Signup and view all the flashcards
Testosterone
Testosterone
Signup and view all the flashcards
Acrosome
Acrosome
Signup and view all the flashcards
Ovaries
Ovaries
Signup and view all the flashcards
Fallopian Tubes
Fallopian Tubes
Signup and view all the flashcards
Uterus
Uterus
Signup and view all the flashcards
Endometrium
Endometrium
Signup and view all the flashcards
Cervix
Cervix
Signup and view all the flashcards
Vagina
Vagina
Signup and view all the flashcards
Vulva
Vulva
Signup and view all the flashcards
Oestrogen
Oestrogen
Signup and view all the flashcards
Spermatogenesis
Spermatogenesis
Signup and view all the flashcards
Oogenesis
Oogenesis
Signup and view all the flashcards
FSH (Follicle-Stimulating Hormone)
FSH (Follicle-Stimulating Hormone)
Signup and view all the flashcards
LH (Luteinizing Hormone)
LH (Luteinizing Hormone)
Signup and view all the flashcards
Fertilization
Fertilization
Signup and view all the flashcards
Zygote
Zygote
Signup and view all the flashcards
Morula
Morula
Signup and view all the flashcards
Blastocyst
Blastocyst
Signup and view all the flashcards
Implantation
Implantation
Signup and view all the flashcards
Gestation Period
Gestation Period
Signup and view all the flashcards
Placenta
Placenta
Signup and view all the flashcards
Umbilical Cord
Umbilical Cord
Signup and view all the flashcards
Amnion
Amnion
Signup and view all the flashcards
Testosterone's role in male puberty
Testosterone's role in male puberty
Signup and view all the flashcards
Sexual organ growth (male)
Sexual organ growth (male)
Signup and view all the flashcards
Sperm production initiation
Sperm production initiation
Signup and view all the flashcards
Body hair emergence (male)
Body hair emergence (male)
Signup and view all the flashcards
Muscular and vocal development (male)
Muscular and vocal development (male)
Signup and view all the flashcards
Oestrogen's role in female puberty
Oestrogen's role in female puberty
Signup and view all the flashcards
Sexual organ growth (female)
Sexual organ growth (female)
Signup and view all the flashcards
Menstrual cycle initiation
Menstrual cycle initiation
Signup and view all the flashcards
Pubic hair emergence (female)
Pubic hair emergence (female)
Signup and view all the flashcards
Breasts and hips development
Breasts and hips development
Signup and view all the flashcards
Spermatogenesis location
Spermatogenesis location
Signup and view all the flashcards
Meiosis in spermatogenesis
Meiosis in spermatogenesis
Signup and view all the flashcards
Sperm cell structure
Sperm cell structure
Signup and view all the flashcards
Acrosome function
Acrosome function
Signup and view all the flashcards
Mitochondria in sperm
Mitochondria in sperm
Signup and view all the flashcards
Sperm tail function
Sperm tail function
Signup and view all the flashcards
Oogenesis location
Oogenesis location
Signup and view all the flashcards
Mitosis in oogenesis
Mitosis in oogenesis
Signup and view all the flashcards
FSH function
FSH function
Signup and view all the flashcards
Follicle cells
Follicle cells
Signup and view all the flashcards
Ovum jelly layer function
Ovum jelly layer function
Signup and view all the flashcards
Ovum cytoplasm function
Ovum cytoplasm function
Signup and view all the flashcards
Ovum nucleus content
Ovum nucleus content
Signup and view all the flashcards
Menstrual Cycle Overview
Menstrual Cycle Overview
Signup and view all the flashcards
Days 1-7 (Menstruation) of cycle
Days 1-7 (Menstruation) of cycle
Signup and view all the flashcards
Endometrium Breakdown
Endometrium Breakdown
Signup and view all the flashcards
Days 8-13 (Follicular Phase) of cycle
Days 8-13 (Follicular Phase) of cycle
Signup and view all the flashcards
Endometrium Thickening
Endometrium Thickening
Signup and view all the flashcards
Day 14 (Ovulation)
Day 14 (Ovulation)
Signup and view all the flashcards
Days 15-22 (Luteal Phase) of cycle
Days 15-22 (Luteal Phase) of cycle
Signup and view all the flashcards
Endometrium Development
Endometrium Development
Signup and view all the flashcards
Days 23-28 of the cycle
Days 23-28 of the cycle
Signup and view all the flashcards
FSH function
FSH function
Signup and view all the flashcards
LH surge
LH surge
Signup and view all the flashcards
Oestrogen's endometrium role
Oestrogen's endometrium role
Signup and view all the flashcards
Progesterone's role
Progesterone's role
Signup and view all the flashcards
Copulation and Ejaculation
Copulation and Ejaculation
Signup and view all the flashcards
Sperm Journey
Sperm Journey
Signup and view all the flashcards
Fertilization result
Fertilization result
Signup and view all the flashcards
Zygote Division
Zygote Division
Signup and view all the flashcards
Epididymis function
Epididymis function
Signup and view all the flashcards
Vas Deferens function
Vas Deferens function
Signup and view all the flashcards
Prostate Gland function
Prostate Gland function
Signup and view all the flashcards
Fallopian Tubes function
Fallopian Tubes function
Signup and view all the flashcards
Uterus function
Uterus function
Signup and view all the flashcards
Vagina function
Vagina function
Signup and view all the flashcards
Sexual organ growth (male puberty)
Sexual organ growth (male puberty)
Signup and view all the flashcards
Sperm Production puberty
Sperm Production puberty
Signup and view all the flashcards
Spermatogenesis basics
Spermatogenesis basics
Signup and view all the flashcards
Oogenesis basics
Oogenesis basics
Signup and view all the flashcards
Follicle Cells role
Follicle Cells role
Signup and view all the flashcards
Union of gametes
Union of gametes
Signup and view all the flashcards
Study Notes
Male Reproductive System
- Composed of distinct parts, each with specific functions crucial for reproduction.
- Testes are primary male reproductive organs, responsible for producing sperm cells and testosterone.
- Testes are oval-shaped glands suspended in the scrotum.
- Scrotum maintains sperm at a temperature slightly lower than the body's core temperature.
- Sperm production occurs at about 2°C lower than the body's standard temperature.
- Epididymis is a coiled tube located on the outside of the testes within the scrotum.
- Epididymis is where sperm cells mature and are stored after production in the testes.
- Vas Deferens (Sperm Duct) is a muscular tube that transports sperm from the epididymis to the urethra.
- Urethra runs through the penis and expels semen (during ejaculation) and urine (during urination).
- Seminal Vesicles are glands attached to the vas deferens near the base of the bladder.
- Seminal Vesicles produce a nutrient-rich fluid that provides energy for sperm cells' mobility and survival.
- Prostate Gland produces an alkaline fluid that is part of semen.
- The alkalinity of the prostate fluid neutralizes the acidic environment of the vagina, protecting the sperm.
- Cowper’s Gland (Bulbourethral Gland) produces a mucus-like fluid released before ejaculation.
- The Cowper's Gland fluid lubricates the urethra and neutralizes traces of acidic urine.
- Penis is the external organ through which the urethra runs.
- The penis delivers sperm into the female reproductive tract during sexual intercourse.
- Testosterone, produced by the testes, plays crucial roles in the male reproductive system.
- Testosterone aids in the development of male secondary sexual characteristics.
- Secondary sexual characteristics include facial hair, deep voice, and muscle mass.
- Testosterone stimulates the maturation of sperm cells.
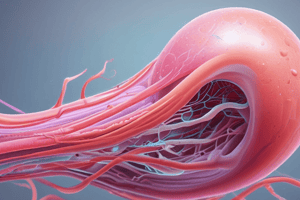
- A sperm cell's structure delivers the male's genetic material to the female's egg.
- The sperm cell head contains the nucleus with 23 chromosomes and is capped by the acrosome.
- The acrosome contains enzymes essential for penetrating the egg cell during fertilization.
- The sperm cell middle section houses mitochondria, providing energy required for movement.
- The sperm cell tail is used for swimming, propelling the sperm towards the egg for potential fertilization.
Female Reproductive System
- Ovaries found as a pair on either side of the uterus, surrounded by germinal epithelium.
- Ovaries produce egg cells and secrete the hormones progesterone and estrogen.
- Fallopian Tubes connect the ovaries to the uterus and are lined with ciliated columnar epithelium.
- The ciliated columnar epithelium helps move the egg cells.
- Fallopian Tubes transport egg cells from the ovary to the uterus.
- The Fallopian Tubes are also the site of fertilization.
- The Uterus is a hollow, pear-shaped organ.
- The Uterus houses and protects the embryo and fetus during pregnancy.
- The Endometrium is the inner lining of the uterus.
- The Endometrium is the site of implantation and where the placenta forms.
- The Cervix is the lower, narrow opening of the uterus.
- The Cervix stretches and opens to allow the baby through during childbirth.
- The Vagina is a muscular tube that runs from the cervix to the exterior.
- The Vagina receives the penis and semen during sexual intercourse.
- The vagina serves as the birth canal and the passage for menstrual blood.
- Vulva - The opening to the vagina is covered by two labia.
- The Vulva protects the entrance to the vagina.
Puberty
- Male puberty is primarily stimulated by the hormone testosterone.
- There is an increase in size and function of male sex organs.
- Initiation of sperm cell production marks sexual maturation.
- There is the emergence of pubic, facial, and body hair.
- Muscles develop more prominently, and the voice deepens.
- Female puberty is driven by the hormone oestrogen.
- There is growth in the female sex organs.
- The start of the menstrual cycle and the production of ova indicate fertility.
- Pubic hair begins to grow.
- There's noticeable growth and development of breasts.
- The widening of hips marks physical maturity.
Gametogenesis
- Spermatogenesis refers to the process of male gamete (sperm cell) production in the testes.
- Spermatogenesis takes place in the seminiferous tubules' germinal epithelium.
- Spermatogenesis is driven by testosterone.
- Diploid germinal epithelial cells (with 46 chromosomes) divide through meiosis.
- Haploid sperm cells contain 23 chromosomes each.
- Sperm cells may carry either an X or a Y chromosome, contributing to offspring's sex determination.
- Under testosterone's influence, diploid germinal epithelial cells undergo meiosis.
- The meiotic division results in four haploid spermatids.
- Spermatids mature into fully-fledged sperm cells.
- The sperm cell head consists of the nucleus, housing 22 autosomes and one sex chromosome (X or Y).
- The sperm cell head also contains the acrosome, filled with enzymes for penetrating the egg's outer layers.
- The middle portion of the sperm is packed with mitochondria, supplying the energy for motility.
- The tail enables the sperm to swim through fluid, propelling the cell forward for fertilization.
- Oogenesis produces female gametes (ova or egg cells) in the ovaries.
- It begins in the diploid germinal epithelium, which divides through mitosis to form multiple follicles.
- Events are cyclical and occur approximately every 28 days, regulated by FSH.
- Mitosis of diploid germinal epithelium cells produces numerous follicles.
- FSH stimulates one of these follicles each cycle, leading to the enlargement of one cell.
- This meiotic process results in four haploid cells, but only one survives to become a mature ovum; the remaining three degenerate.
- Follicle cells surround the egg, offering support and protection.
- A layer of jelly safeguards the egg, particularly during the early developmental stages post-fertilization.
- The cytoplasm provides essential nutrients for the developing egg.
- A haploid nucleus containing 22 autosomes and one X chromosome merges with a sperm's genetic material.
Menstrual Cycle
- It involves changes in the ovaries (ovarian cycle) and the uterus (uterine cycle).
- The average cycle is 28 days, though this can vary.
- Days 1–7 (Menstruation): New follicles in the ovaries develop and secrete oestrogen.
- The endometrium breaks down and is shed during menstruation.
- Days 8–13 (Follicular Phase): A mature Graafian follicle develops in the ovaries.
- The Graafian follicle moves to the edge of the ovary and secretes oestrogen.
- Oestrogen leads to the thickening of the endometrium and the development of more blood vessels and glands.
- Day 14 (Ovulation): The Graafian follicle bursts to release an egg cell.
- Days 15–22 (Luteal Phase): The ruptured Graafian follicle transforms into the corpus luteum.
- The corpus luteum secretes progesterone.
- Progesterone further stimulates the endometrium to thicken and develop more blood vessels and glands.
- Days 23–28: If fertilisation does not occur, the corpus luteum shrinks and stops producing progesterone.
- The breakdown of the endometrium occurs, causing menstruation.
- If fertilisation does occur, the corpus luteum remains active and continues to secrete progesterone.
- Progesterone prevents menstruation and supports pregnancy.
- FSH (Follicle-Stimulating Hormone) is produced by the pituitary gland.
- FSH stimulates the development of the follicle in the ovaries.
- LH (Luteinizing Hormone) is also produced by the pituitary gland.
- LH levels peak around day 14, triggering ovulation and the formation of the corpus luteum.
- Oestrogen levels increase as the follicle develops, leading to the thickening of the endometrium.
- After ovulation, oestrogen levels initially decrease as the Graafian follicle ceases functioning.
- Progesterone is produced by the corpus luteum post-ovulation.
- Progesterone levels increase to prepare the endometrium for pregnancy.
- If fertilisation does not occur, progesterone levels fall, leading to the shedding of the endometrial lining.
Fertilization and Development of Zygote to Blastocyst
- During copulation, the penis is inserted into the vagina, and sperm cells are released close to the cervix.
- Sperm swim through the cervix, into the uterus, and up through the fallopian tubes.
- If a haploid ovum (released during ovulation) is present in the fallopian tubes, one sperm cell may penetrate its jelly layer, leading to fertilization.
- The union results in a diploid zygote, where the nuclei of the ovum and sperm cell fuse.
- Post-fertilization, the zygote undergoes mitosis while moving down the fallopian tube toward the uterus.
- This continuous mitotic division forms a solid ball of cells known as the morula.
- As division continues, the morula develops into a hollow, fluid-filled ball of cells termed the blastocyst.
- The blastocyst typically occurs around five days after fertilization.
- The blastocyst travels from the fallopian tube to the uterus, where it embeds itself into the endometrium, a process known as implantation.
- The outer cells of the blastocyst secrete enzymes that soften a portion of the uterine wall, allowing the blastocyst to embed.
- Following implantation, the outer layers of the blastocyst develop into extra-embryonic membranes—the amnion and the chorion.
- The chorion forms the chorionic villi that extend into the endometrium and contribute to placenta formation, which in turn secretes progesterone.
- At this stage, the blastocyst is referred to as the embryo.
- The embryo will develop throughout the gestation period, lasting about 40 weeks or 280 days, until birth.
- After 12 weeks of gestation, the embryo is then referred to as a fetus.
Implantation, Gestation, and the Role of the Placenta
- Ovulation occurs usually on day 14 of the menstrual cycle.
- A mature Graafian follicle in the ovary bursts and releases an egg cell.
- Fertilization happens high up in the fallopian tube.
- The egg cell (23 chromosomes) and the sperm cell (23 chromosomes) fuse to form a zygote (46 chromosomes).
- After fertilization, the zygote divides by mitosis, forming first a morula, then a blastocyst, and finally an embryo.
- The embryo is as it moves down the fallopian tube towards the uterus.
- The embryo reaches the uterus in about 5 to 7 days and embeds itself into the endometrium, known as implantation.
- Post-implantation the embryo develops many finger-like structures called villi from its outer membrane, that grow into the uterine tissue to form the placenta.
- The placenta connects to the embryo via the umbilical cord.
- The umbilical cord contains two umbilical arteries carrying deoxygenated blood from the embryo to the placenta, and one umbilical vein that carries oxygenated blood from the placenta to the embryo.
- The embryo is encased in a fluid-filled sac called the amnion.
- The fluid inside the amnion is referred to as amniotic fluid.
- After approximately eight weeks, the embryo develops into a fetus.
- Structures such as limbs and all necessary body organs have formed.
- Gestation is the time from fertilization to birth, typically lasts for about 9 months or 39–40 weeks.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.