Podcast
Questions and Answers
How do pulmonary arteries contribute to the perfusion of the lungs?
How do pulmonary arteries contribute to the perfusion of the lungs?
- By directly feeding oxygen to the alveolar capillaries.
- By delivering systemic venous blood from the heart to the lungs for oxygenation. (correct)
- By providing high-pressure, low-volume blood directly to the alveoli.
- By carrying oxygenated blood from the lungs to the heart.
Why is the low-pressure, high-volume system of the pulmonary veins important for respiratory function?
Why is the low-pressure, high-volume system of the pulmonary veins important for respiratory function?
- It ensures the rapid delivery of oxygenated blood to the systemic circulation.
- It helps maintain a consistent blood pressure throughout the respiratory cycle.
- It facilitates efficient gas exchange by maximizing the contact time between blood and alveolar air. (correct)
- It minimizes the risk of pulmonary edema by preventing high hydrostatic pressure in the lungs.
What role does angiotensin-converting enzyme (ACE) play within the lung capillary endothelium?
What role does angiotensin-converting enzyme (ACE) play within the lung capillary endothelium?
- It stimulates the production of surfactant to reduce alveolar surface tension.
- It helps regulate blood pressure by converting angiotensin I to angiotensin II. (correct)
- It breaks down blood clots to maintain pulmonary blood flow.
- It directly facilitates oxygen transport across the alveolar membrane.
How does Boyle's Law explain the mechanics of pulmonary ventilation?
How does Boyle's Law explain the mechanics of pulmonary ventilation?
Atmospheric pressure is critical in ventilation. What is true regarding atmospheric pressure?
Atmospheric pressure is critical in ventilation. What is true regarding atmospheric pressure?
During pulmonary ventilation, what happens to intrapulmonary pressure during inspiration and expiration?
During pulmonary ventilation, what happens to intrapulmonary pressure during inspiration and expiration?
Why is it important to maintain a minimal amount of fluid in the intrapleural space?
Why is it important to maintain a minimal amount of fluid in the intrapleural space?
The lungs' natural tendency to recoil and the surface tension of alveolar fluid both promote what?
The lungs' natural tendency to recoil and the surface tension of alveolar fluid both promote what?
How is negative intrapleural pressure ($P_{ip}$) affected by the opposing forces within the thoracic cavity?
How is negative intrapleural pressure ($P_{ip}$) affected by the opposing forces within the thoracic cavity?
If the intrapleural pressure ($P_{ip}$) becomes equal to intrapulmonary pressure ($P_{pul}$), what is the most likely result?
If the intrapleural pressure ($P_{ip}$) becomes equal to intrapulmonary pressure ($P_{pul}$), what is the most likely result?
What correctly describes the order in which pressure changes occur during inspiration?
What correctly describes the order in which pressure changes occur during inspiration?
How does surfactant prevent atelectasis?
How does surfactant prevent atelectasis?
According to the provided information, what is a major nonelastic source of resistance to gas flow in the airways?
According to the provided information, what is a major nonelastic source of resistance to gas flow in the airways?
How is the relationship between flow (F), pressure ($\Delta P$), and resistance (R) best described in the context of pulmonary ventilation?
How is the relationship between flow (F), pressure ($\Delta P$), and resistance (R) best described in the context of pulmonary ventilation?
Why is airway resistance the greatest when considering the respiratory tract?
Why is airway resistance the greatest when considering the respiratory tract?
How would decreased lung compliance affect pulmonary ventilation?
How would decreased lung compliance affect pulmonary ventilation?
Mathematically, the equation $C_L = \Delta V_L / \Delta (P_{pul} - P_{ip})$ represents what?
Mathematically, the equation $C_L = \Delta V_L / \Delta (P_{pul} - P_{ip})$ represents what?
What does external respiration primarily involve?
What does external respiration primarily involve?
How does an increased thickness of the respiratory membrane affect external respiration?
How does an increased thickness of the respiratory membrane affect external respiration?
After blood passes the alveoli in the lungs what is approximate PO2 and PCO2?
After blood passes the alveoli in the lungs what is approximate PO2 and PCO2?
Why is ventilation-perfusion coupling essential for efficient gas exchange?
Why is ventilation-perfusion coupling essential for efficient gas exchange?
What describes how local autoregulatory mechanisms respond when ventilation is greater for alveolar perfusion.
What describes how local autoregulatory mechanisms respond when ventilation is greater for alveolar perfusion.
What is a potential consequence of an imbalance in ventilation-perfusion coupling in the lungs?
What is a potential consequence of an imbalance in ventilation-perfusion coupling in the lungs?
How does regional positioning of the blood in the lungs effect pulmonary arterial pressure?
How does regional positioning of the blood in the lungs effect pulmonary arterial pressure?
The parasympathetic motor fibers have what impact on pulmonary ventilation?
The parasympathetic motor fibers have what impact on pulmonary ventilation?
How does the body accommodate an increased need for oxygen during exercise given the limited transit time in pulmonary capillaries (~0.75 seconds)?
How does the body accommodate an increased need for oxygen during exercise given the limited transit time in pulmonary capillaries (~0.75 seconds)?
Why does carbon dioxide (CO2) still diffuse in equal amounts to oxygen (O2) despite having a partial pressure gradient that is not as steep?
Why does carbon dioxide (CO2) still diffuse in equal amounts to oxygen (O2) despite having a partial pressure gradient that is not as steep?
How is atelectasis described?
How is atelectasis described?
According to the material what is not true of the fluid surrounding the lungs?
According to the material what is not true of the fluid surrounding the lungs?
What is the equation most closely related to Boyle's Law?
What is the equation most closely related to Boyle's Law?
What is true of bronchial arteries?
What is true of bronchial arteries?
What is the correct order of the flow of air in and out of the lungs?
What is the correct order of the flow of air in and out of the lungs?
How does the body ensure enough oxygen can get into the blood to reach the tissues when exercising?
How does the body ensure enough oxygen can get into the blood to reach the tissues when exercising?
What is the effect of having the arteries about 12 cm above or below the hilum has?
What is the effect of having the arteries about 12 cm above or below the hilum has?
How does positive Pip form in the lungs?
How does positive Pip form in the lungs?
What are the three typical types of Atelectasis?
What are the three typical types of Atelectasis?
What is the effect of histamine on the lungs when considering external respiration?
What is the effect of histamine on the lungs when considering external respiration?
Flashcards
Lung perfusion:
Lung perfusion:
Blood supply to the lungs from two circulations; pulmonary and bronchial.
Pulmonary arteries:
Pulmonary arteries:
Vessels delivering systemic venous blood from heart to lungs.
Pulmonary veins:
Pulmonary veins:
Vessels carrying oxygenated blood from respiratory zones back to the heart.
Pulmonary circulation:
Pulmonary circulation:
Signup and view all the flashcards
Bronchial arteries:
Bronchial arteries:
Signup and view all the flashcards
Pulmonary ventilation:
Pulmonary ventilation:
Signup and view all the flashcards
Atmospheric Pressure (Patm):
Atmospheric Pressure (Patm):
Signup and view all the flashcards
Intrapulmonary Pressure (Ppul):
Intrapulmonary Pressure (Ppul):
Signup and view all the flashcards
Intrapleural Pressure (Pip):
Intrapleural Pressure (Pip):
Signup and view all the flashcards
Transpulmonary Pressure:
Transpulmonary Pressure:
Signup and view all the flashcards
Lung collapse (inward force):
Lung collapse (inward force):
Signup and view all the flashcards
Lung expansion (outward force):
Lung expansion (outward force):
Signup and view all the flashcards
Negative Pip maintenance:
Negative Pip maintenance:
Signup and view all the flashcards
Pneumothorax:
Pneumothorax:
Signup and view all the flashcards
Atelectasis:
Atelectasis:
Signup and view all the flashcards
Boyle's Law:
Boyle's Law:
Signup and view all the flashcards
Pulmonary Ventilation mechanism:
Pulmonary Ventilation mechanism:
Signup and view all the flashcards
Pneumothorax cause:
Pneumothorax cause:
Signup and view all the flashcards
Definition of Atelectasis:
Definition of Atelectasis:
Signup and view all the flashcards
Surface tension:
Surface tension:
Signup and view all the flashcards
Surfactant:
Surfactant:
Signup and view all the flashcards
Airway resistance:
Airway resistance:
Signup and view all the flashcards
Lung compliance:
Lung compliance:
Signup and view all the flashcards
External Respiration:
External Respiration:
Signup and view all the flashcards
Internal Respiration:
Internal Respiration:
Signup and view all the flashcards
Partial pressure gradients:
Partial pressure gradients:
Signup and view all the flashcards
Resistance Site:
Resistance Site:
Signup and view all the flashcards
Nerve control of the lungs:
Nerve control of the lungs:
Signup and view all the flashcards
Balance between bronchoconstriction and bronchodilation:
Balance between bronchoconstriction and bronchodilation:
Signup and view all the flashcards
Influence of local PO2 on perfusion
Influence of local PO2 on perfusion
Signup and view all the flashcards
balanciing
balanciing
Signup and view all the flashcards
Study Notes
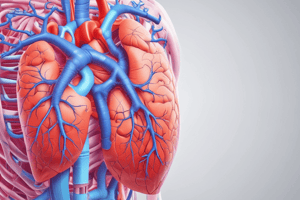
- Lungs are perfused by two circulations: the pulmonary circulation and the bronchial circulation.
Pulmonary Circulation
- Pulmonary arteries deliver systemic venous blood from the heart to the lungs for oxygenation.
- Pulmonary arteries branch profusely and feed into pulmonary capillary networks.
- Pulmonary veins carry oxygenated blood from the respiratory zones back to the heart.
- The pulmonary circulation is a low-pressure, high-volume system.
- Lung capillary endothelium contains enzymes to act on substances in blood.
- Angiotensin-converting enzyme activates blood pressure hormone in the lungs.
Bronchial Circulation
- Bronchial arteries provide oxygenated blood to the lungs and lung tissue.
- Bronchial arteries arise from the aorta and enter the lungs at the hilum.
- It is part of systemic circulation, and is a high pressure, low volume system.
- Bronchial arteries supply all lung tissue except the alveoli.
- Bronchial veins anastomose with pulmonary veins.
- Pulmonary veins carry most venous blood back to the heart.
Respiratory Physiology
- Pulmonary ventilation consists of two phases: inspiration and expiration.
- Inspiration is when gases flow into the lungs.
- Expiration is when gases exit the lungs.
Pressure Relationships in the Thoracic Cavity
- Atmospheric pressure (Patm) is the pressure exerted by the air surrounding the body
- 760 mm Hg at sea level = 1 atmosphere
- Respiratory pressures are described relative to atmospheric pressure, e.g., a respiratory pressure of -5 mmHg means the pressure is lower than Patm by 5 mm Hg.
Intrapulmonary Pressure
- Intrapulmonary pressure (Ppul) is the pressure in the alveoli.
- It is also called intra-alveolar pressure
- It fluctuates with breathing.
- It always eventually equalizes with atmospheric pressure (Patm).
Intrapleural Pressure
- Intrapleural pressure (Pip) is pressure in the pleural cavity.
- Intrapleural pressure fluctuates with breathing
- It is always a negative pressure (<Patm and <Ppul).
- Pip is usually 4 mm Hg less than Ppul.
- Fluid level must be kept at a minimum to keep lungs inflated.
- Excess fluid is pumped out by the lymphatic system to maintain appropriate functioning.
- Positive Pip pressure causes the lung to collapse.
Additional Notes on Intrapleural pressure (Pip)
- Its pressure is created by two opposing elastic forces: a collapsing force and an expanding force.
- Two inward forces promote lung collapse.
- Lungs' natural tendency to recoil because of elasticity, causing the lungs to try to assume the smallest size.
- Surface tension of alveolar fluid: surface tension pulls on alveoli to try to reduce alveolar size.
- One outward force promotes lung expansion.
- The elasticity of the chest wall pulls the thorax outward.
- The negative Pip is affected by these opposing forces but is maintained by a strong adhesive force between the parietal and visceral pleurae.
- The chest wall pulls outward into the intrapleural space due to forces created by recoil and surface tension.
- The lungs pull inward, tending to separate the visceral and parietal pleurae.
- A negative intrapleural pressure is created that opposes the separation and outward recoil forces of the chest wall and inward recoil forces of the lungs.
- Fluid accumulation in the pleural cavity causes positive Pip.
Pulmonary Ventilation
- It consists of inspiration and expiration.
- It is a mechanical process that depends on volume changes in the thoracic cavity.
- Volume changes lead to pressure changes and are facilitated by muscles.
- Pressure changes lead to the flow of gases to equalize pressure.
- It is determined by Boyle's law.
Boyle's Law
- Boyle's law describes the relationship between pressure and volume of a gas.
- Gases always fill the container they are in.
- If the amount of gas is the same and the container size is reduced, pressure will increase.
- Pressure (P) varies inversely with volume (V) and can be expressed mathematically as P1V1 = P2V2.
Intrapulmonary Pressure
- It is dependent on Boyle's Law.
Clinical Imbalance: Atelectasis
- Atelectasis: lung collapse due to plugged bronchioles, which cause collapse of alveoli, or pneumothorax which introduces air in the pleural cavity.
- Pneumothorax can occur from a wound in the parietal pleura, or rupture of the visceral pleura.
- It is treated by removing air with chest tubes.
- The lungs reinflate when the pleurae heal.
- It is not a pathology, but a condition that describes an incomplete expansion of the lung, or collapse of a previously inflated lung.
- It can occur as a consequence of several respiratory pathologies.
3 main types of atelectasis found in adults:
- Resorption occurs due to incomplete airway obstruction.
- Compression occurs due to the accumulation of transudate, exudate, blood, or air (pneumothorax) in the pleural cavity.
- Contraction is caused by fibrosis that prevents the lungs from fully expanding (attenuated compliance).
Pulmonary Ventilation (At the start of a breath)
- Pressures inside and outside the thorax are identical, so there's no air movement.
- The expanding thoracic cavity expands the lungs.
- Parietal pleura is attached to the thoracic wall, and the visceral pleura is attached to the lungs.
- Pleural fluid forms a slick but tight bond between the two layers
- If injury allows air into the pleural cavity, the bond is broken, the lung collapses (atelectasis).
Pulmonary Ventilation (During exhalation)
- Thoracic cavity decreases in volume.
- Decreased volume causes increased pressure (Poutside < Pinside).
- Air is forced out from an area of high pressure to low pressure.
Physical Factors Influencing Pulmonary Resistance
Airway Resistance:
- Friction is the major nonelastic source of resistance to gas flow and occurs in airways.
- Flow (F) is equal to the pressure differential divided by resistance (R): F = ΔP / R
- The pressure gradient between the atmosphere and alveoli is only 2 mm Hg or less during normal quiet breathing.
- A 2 mm Hg difference is sufficient to move 500 ml of air.
- Airway resistance is greatest in the bronchioles.
- Gas flow changes inversely with resistance.
- Resistance in the respiratory tree is usually insignificant, due to large airway diameters in the first part of the conducting zone.
- Progressive branching of airways (getting smaller) also increases total cross-sectional area.
- Resistance usually occurs in medium-sized bronchi.
- In terminal bronchioles, resistance is negligible because diffusion drives gas movement.
Alveolar Surface Tension:
- Surface tension is the attraction of liquid molecules to one another at a gas-liquid interface.
- It draws liquid molecules closer together and reduces contact with dissimilar gas molecules.
- Surface tension resists any force that tends to increase the surface area of a liquid.
- Water, which has very high surface tension, coats alveolar walls in a thin film and tends to cause alveoli to shrink to the smallest size (i.e., collapse).
- Surfactant reduces surface tension.
- A surfactant is the body's detergent-like lipid and protein complex that helps to reduce surface tension of alveolar fluid.
- It prevents alveolar collapse.
- A surfactant is produced by type II alveolar cells.
Lung Compliance
- Lung compliance is the measure of change in lung volume that occurs with a given change in transpulmonary pressure.
- Measure of how much lung stretches and is normally high because lungs are distensible, and there is surfactant, which decreases alveolar surface tension.
- Higher lung compliance means it is easier to expand the lungs.
- The formula for lung compliance is written mathematically as: CL = ΔV / Δ(Ppul - Pip), with Cl equal to compliance, ΔV₁ equal to the change in lung volume, and D(Ppul-Pip) equal to the change in transpulmonary pressure.
- Compliance can be diminished by: nonelastic scar tissue (fibrosis), reduced production of surfactant, and decreased flexibility of the thoracic cage.
Respiration
- External respiration: pulmonary gas exchange between alveoli and pulmonary capillaries
- Internal respiration: capillary gas exchange between blood capillaries and body tissues
External Respiration
- External respiration (pulmonary gas exchange) involves the exchange of O2 and CO2 across respiratory membranes.
- Exchange is influenced by: partial pressure gradients, and gas solubilities, thickness and surface area of respiratory membrane, and ventilation-perfusion coupling
- View the videos for additional understanding of the pleural space and pleural effusions.
Partial pressure gradients and gas solubilities in external respiration
- A steep partial pressure gradient for O2 exists between blood and lungs.
- Venous blood Po₂ = 40 mm Hg
- Alveolar Po₂ = 104 mm Hg
- Drives oxygen flow into blood
- Equilibrium is reached across the respiratory membrane in ~0.25 seconds, but it takes red blood cells ~0.75 seconds to travel from start to end of the pulmonary capillary.
- The partial pressure gradient for CO2 is less steep.
- Venous blood Pco₂ = 45 mm Hg
- Alveolar Pco₂ = 40 mm Hg
- Though the gradient is not as steep, CO2 still diffuses in equal amounts with oxygen. CO2 is 20x more soluble in plasma and alveolar fluid than oxygen.
Thickness of respiratory membrane in external respiration
- In addition to a steep partial pressure gradient, the respiratory membrane contributes to efficient gas exchange.
- Respiratory membranes are very thin, between 0.5 to 1 µm thick.
- The large total surface area of the alveoli is 40x the surface area of the skin.
Local PO2 and PCO2 levels on perfusion:
- Changes in PO2 in alveoli cause changes in diameters of arterioles.
- Where alveolar O2 is high, arterioles dilate to increase blood flow to those alveoli.
- Where alveolar O2 is low, arterioles constrict, directing blood to alveoli where oxygen is high, so that blood can pick up more oxygen
- This mechanism is opposite than seen in the systemic arterioles that dilate when oxygen is low and constrict when oxygen is high.
- Changes in PCO2 in alveoli cause changes in diameters of bronchioles.
- Where alveolar CO2 is high, bronchioles dilate, and this allows the elimination of CO2 more rapidly.
- Where alveolar CO2 is low, bronchioles constrict.
Balancing Ventilation and Perfusion
- Changing diameters of local arterioles and bronchioles synchronizes ventilation-perfusion.
- Ventilation-perfusion is never balanced for all alveoli because:
- Regional variations may be present, due to the effect of gravity on blood and air flow through lungs.
- Occasionally, alveolar ducts plugged with mucus create unventilated areas in the lungs.
- Ventilation and Q/Q are controlled by autoregulatory mechanisms that sense PO2 and PCO2
- V stands for Ventilation
- Q stands for the Perfusion rate
Distributions of Pulmonary Blood Flow
- Blood flow in the lungs is distributed differently because of the effect of gravity and creates three zones in the lungs
- Zone 1 is at the apex
- Zone 2 is midway
- Zone 3 is above the base
- Blood enters the hilum via the pulmonary artery and exerts an average pulmonary arterial pressure
- Arteries in Zone 1 are about 12 cm above hilum - gravity reduces pulmonary arterial pressure
- Arteries in Zone 3 are about 12 cm below the hilum - gravity increases pulmonary arterial pressure
Innervation of the lungs
- Lungs are innervated by parasympathetic and sympathetic motor fibers, as well as visceral sensory fibers.
- Nerves enter through the pulmonary plexus on the lung root (hilum) then run along bronchial tubes and blood vessels
- Parasympathetic motor fibers cause bronchoconstriction of airways and mucous production
- Autonomic excitatory cholinergic nerves secrete acetylcholine into bronchial smooth muscle cells and submucosal glands
- Sympathetic motor fibers regulate bronchodilation of airways
- Inhibitory nonadrenergic and noncholinergic nerves cause airway bronchodilation
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.