Podcast
Questions and Answers
Which of the following is the MOST common initial symptom reported by patients with lumbosacral radiculopathy?
Which of the following is the MOST common initial symptom reported by patients with lumbosacral radiculopathy?
- Bowel and bladder dysfunction
- Radicular pain (correct)
- Progressive numbness in the affected dermatome
- Motor weakness in the lower extremities
A patient presents with lumbosacral radiculopathy. Which historical finding would be MOST concerning for an urgent underlying condition?
A patient presents with lumbosacral radiculopathy. Which historical finding would be MOST concerning for an urgent underlying condition?
- Intermittent low back pain for several years
- Numbness and tingling in the toes after exercise
- A history of significant trauma (correct)
- Reports of pain radiating down the leg with prolonged sitting
Which of the following is the MOST relevant detail to note about radicular pain?
Which of the following is the MOST relevant detail to note about radicular pain?
- It is characterized by patients as electrical shocks or shooting pain. (correct)
- It is localized to the lower back.
- It is constant and unremitting.
- It typically improves with activity.
Which of the following is LEAST likely to cause radicular symptoms?
Which of the following is LEAST likely to cause radicular symptoms?
A 60-year-old patient presents with low back pain and radicular symptoms. Which of the following 'red flag' symptoms warrants immediate investigation?
A 60-year-old patient presents with low back pain and radicular symptoms. Which of the following 'red flag' symptoms warrants immediate investigation?
During a physical exam for suspected lumbosacral radiculopathy, which finding would be MOST indicative of upper motor neuron involvement?
During a physical exam for suspected lumbosacral radiculopathy, which finding would be MOST indicative of upper motor neuron involvement?
A patient with suspected L5 radiculopathy is being examined. What specific finding related to reflexes would support this diagnosis?
A patient with suspected L5 radiculopathy is being examined. What specific finding related to reflexes would support this diagnosis?
A patient reports pain along the lateral aspect of their left foot. Which nerve root is MOST likely involved?
A patient reports pain along the lateral aspect of their left foot. Which nerve root is MOST likely involved?
During a straight leg raise test, a patient reports reproduction of their radicular pain at 45 degrees of hip flexion. This finding is MOST suggestive of nerve root involvement from which of the following spinal segments?
During a straight leg raise test, a patient reports reproduction of their radicular pain at 45 degrees of hip flexion. This finding is MOST suggestive of nerve root involvement from which of the following spinal segments?
The reverse straight leg raise (femoral nerve stretch test) primarily stretches which of the following nerves and nerve roots?
The reverse straight leg raise (femoral nerve stretch test) primarily stretches which of the following nerves and nerve roots?
After nonoperative measures fail, a patient is considered for surgical intervention for lumbar disc herniation. Which of the following is the MOST common initial surgical procedure?
After nonoperative measures fail, a patient is considered for surgical intervention for lumbar disc herniation. Which of the following is the MOST common initial surgical procedure?
Which of the following best describes the MOST common location for lumbar disc herniations?
Which of the following best describes the MOST common location for lumbar disc herniations?
In the lumbar spine, a posterolateral disc herniation at L4-L5 will MOST likely compress which nerve root?
In the lumbar spine, a posterolateral disc herniation at L4-L5 will MOST likely compress which nerve root?
Which of the following statements BEST describes the composition of the nucleus pulposus?
Which of the following statements BEST describes the composition of the nucleus pulposus?
Which of the following best describes the PRIMARY function of the annulus fibrosus in the intervertebral disc?
Which of the following best describes the PRIMARY function of the annulus fibrosus in the intervertebral disc?
What percentage of patients with lumbar disc herniation experience improvement with nonoperative care within approximately 3 months?
What percentage of patients with lumbar disc herniation experience improvement with nonoperative care within approximately 3 months?
Which of the following is a known risk factor for lumbar disc herniation?
Which of the following is a known risk factor for lumbar disc herniation?
Which of the following best describes a disc extrusion?
Which of the following best describes a disc extrusion?
A patient with lumbar radiculopathy is diagnosed with cauda equina syndrome. Which of the following symptoms would be MOST specific to this condition?
A patient with lumbar radiculopathy is diagnosed with cauda equina syndrome. Which of the following symptoms would be MOST specific to this condition?
During a physical examination, which of the following findings would be MOST indicative of L5 radiculopathy?
During a physical examination, which of the following findings would be MOST indicative of L5 radiculopathy?
During a physical exam for lower back pain, the clinician elicits pain during the straight leg raise test that is relieved by dorsiflexion of the ankle. This suggests the patient is suffering primarily from which condition?
During a physical exam for lower back pain, the clinician elicits pain during the straight leg raise test that is relieved by dorsiflexion of the ankle. This suggests the patient is suffering primarily from which condition?
Which imaging modality is generally considered the 'gold standard' for evaluating lumbar disc herniation and nerve root compression?
Which imaging modality is generally considered the 'gold standard' for evaluating lumbar disc herniation and nerve root compression?
A patient with chronic low back pain and suspected lumbar disc herniation has a plain X-ray performed. Which of the following findings would be suggestive of degenerative changes?
A patient with chronic low back pain and suspected lumbar disc herniation has a plain X-ray performed. Which of the following findings would be suggestive of degenerative changes?
Which of the following is NOT typically included in non-operative treatment for lumbar disc herniation?
Which of the following is NOT typically included in non-operative treatment for lumbar disc herniation?
A patient has failed conservative treatment for lumbar disc herniation. Which of the following is generally considered a surgical option?
A patient has failed conservative treatment for lumbar disc herniation. Which of the following is generally considered a surgical option?
After undergoing a lumbar discectomy, a patient develops a dural tear. What is the MOST likely immediate consequence of this complication?
After undergoing a lumbar discectomy, a patient develops a dural tear. What is the MOST likely immediate consequence of this complication?
What is the MOST likely outcome of lumbar discectomy?
What is the MOST likely outcome of lumbar discectomy?
Which of the following is MOST characteristic of neurogenic claudication secondary to lumbar canal stenosis?
Which of the following is MOST characteristic of neurogenic claudication secondary to lumbar canal stenosis?
What is the PRIMARY difference between spondylosis and spondylolisthesis?
What is the PRIMARY difference between spondylosis and spondylolisthesis?
A patient presents with progressive lower extremity weakness and bowel/bladder dysfunction. MRI reveals a large central disc herniation compressing the cauda equina. What is the appropriate next step in management?
A patient presents with progressive lower extremity weakness and bowel/bladder dysfunction. MRI reveals a large central disc herniation compressing the cauda equina. What is the appropriate next step in management?
A patient presents with lower back pain radiating down the leg, and paresthesia. Which of the following is the MOST likely underlying mechanism causing these symptoms?
A patient presents with lower back pain radiating down the leg, and paresthesia. Which of the following is the MOST likely underlying mechanism causing these symptoms?
A patient is diagnosed with lumbosacral radiculopathy. Which of the following findings would suggest a condition beyond a typical disc herniation?
A patient is diagnosed with lumbosacral radiculopathy. Which of the following findings would suggest a condition beyond a typical disc herniation?
During an examination for lumbosacral radiculopathy, a patient reports numbness in the lateral aspect of the foot and diminished ankle plantarflexion strength. Which nerve root is MOST likely affected?
During an examination for lumbosacral radiculopathy, a patient reports numbness in the lateral aspect of the foot and diminished ankle plantarflexion strength. Which nerve root is MOST likely affected?
A patient experiencing radicular pain performs a straight leg raise. At what range of hip flexion is reproduction of radicular pain considered a positive sign, suggestive of nerve root involvement?
A patient experiencing radicular pain performs a straight leg raise. At what range of hip flexion is reproduction of radicular pain considered a positive sign, suggestive of nerve root involvement?
A patient reports anterior thigh pain. Which nerve is MOST likely being stretched during a femoral nerve stretch test?
A patient reports anterior thigh pain. Which nerve is MOST likely being stretched during a femoral nerve stretch test?
A patient is being evaluated for lumbar disc herniation. Which of the following MOST accurately reflects the anatomical relationship relevant to nerve root compression in the lumbar spine?
A patient is being evaluated for lumbar disc herniation. Which of the following MOST accurately reflects the anatomical relationship relevant to nerve root compression in the lumbar spine?
What is the MOST significant difference between cervical and lumbar spine nerve root anatomy that influences how disc herniations affect nerve roots?
What is the MOST significant difference between cervical and lumbar spine nerve root anatomy that influences how disc herniations affect nerve roots?
Why is lumbar disc herniation more likely to be unilateral?
Why is lumbar disc herniation more likely to be unilateral?
Which of the following is the MOST accurate description of the nucleus pulposus?
Which of the following is the MOST accurate description of the nucleus pulposus?
A patient's MRI report indicates a lumbar disc 'extrusion.' Which statement BEST describes this finding?
A patient's MRI report indicates a lumbar disc 'extrusion.' Which statement BEST describes this finding?
A patient with suspected lumbar radiculopathy reports that their leg pain worsens with sitting, coughing, and sneezing, but improves with standing. Which of the following is the MOST likely explanation for these symptoms?
A patient with suspected lumbar radiculopathy reports that their leg pain worsens with sitting, coughing, and sneezing, but improves with standing. Which of the following is the MOST likely explanation for these symptoms?
A patient experiencing symptoms of lumbar radiculopathy undergoes electrodiagnostic testing (EMG/NCV). What is the PRIMARY purpose of this?
A patient experiencing symptoms of lumbar radiculopathy undergoes electrodiagnostic testing (EMG/NCV). What is the PRIMARY purpose of this?
What is the rationale for bed rest in the non-operative treatment of lumbar disc herniation?
What is the rationale for bed rest in the non-operative treatment of lumbar disc herniation?
Selective nerve root corticosteroid injections (SNRB) may be considered in the treatment of lumbar disc herniation when:
Selective nerve root corticosteroid injections (SNRB) may be considered in the treatment of lumbar disc herniation when:
What is the PRIMARY goal when performing a surgical laminectomy and discectomy for lumbar disc herniation?
What is the PRIMARY goal when performing a surgical laminectomy and discectomy for lumbar disc herniation?
Why might fusion and instrumentation be added to a lumbar discectomy?
Why might fusion and instrumentation be added to a lumbar discectomy?
A patient who underwent a lumbar discectomy now presents with increased lower back pain, decreased range of motion, and signs of nerve root irritation. What complication is MOST likely?
A patient who underwent a lumbar discectomy now presents with increased lower back pain, decreased range of motion, and signs of nerve root irritation. What complication is MOST likely?
What is the PRIMARY objective of lumbar canal stenosis treatment?
What is the PRIMARY objective of lumbar canal stenosis treatment?
How does spondylolisthesis lead to radiculopathy?
How does spondylolisthesis lead to radiculopathy?
What is the rationale for using dynamic and oblique views when obtaining plain x-rays for patients with lower back pain?
What is the rationale for using dynamic and oblique views when obtaining plain x-rays for patients with lower back pain?
When is an MRI with gadolinium ESPECIALLY useful in the context of lumbar disc disease?
When is an MRI with gadolinium ESPECIALLY useful in the context of lumbar disc disease?
Which of these is NOT a typical finding on plain X-ray suggestive of degenerative changes in the lumbar spine?
Which of these is NOT a typical finding on plain X-ray suggestive of degenerative changes in the lumbar spine?
Which of the following is the MOST common location for lumbar disc herniations?
Which of the following is the MOST common location for lumbar disc herniations?
Which lumbar level is likely affected by weakness in ankle dorsiflexion and decreased patellar reflex?
Which lumbar level is likely affected by weakness in ankle dorsiflexion and decreased patellar reflex?
What does the FABER test primarily assess?
What does the FABER test primarily assess?
Which type of herniation is most commonly associated with cauda equina syndrome?
Which type of herniation is most commonly associated with cauda equina syndrome?
Why might someone with weakness in hip abduction have issues with the Trendelenburg sign/test?
Why might someone with weakness in hip abduction have issues with the Trendelenburg sign/test?
Arteriovenous malformations (AVM) are in what general category of causes for lumbosacral radiculopathy?
Arteriovenous malformations (AVM) are in what general category of causes for lumbosacral radiculopathy?
Which of the following is not one of the 'Herniation zones'?
Which of the following is not one of the 'Herniation zones'?
Flashcards
Lumbosacral Radiculopathy Definition
Lumbosacral Radiculopathy Definition
A disorder of the spinal nerve roots from L1-S4.
Causes of Lumbosacral Radiculopathy
Causes of Lumbosacral Radiculopathy
Compression, irritation, or stretching of the nerve roots exiting the spine.
Manifestations of Nerve Damage
Manifestations of Nerve Damage
Radiating pain, tingling, numbness, and/or Motor weakness
Radiculopathy
Radiculopathy
Signup and view all the flashcards
Radicular Pain
Radicular Pain
Signup and view all the flashcards
Common Causes of Lumbosacral Radiculopathy
Common Causes of Lumbosacral Radiculopathy
Signup and view all the flashcards
Degenerative Conditions of the Spine
Degenerative Conditions of the Spine
Signup and view all the flashcards
Traumatic Causes
Traumatic Causes
Signup and view all the flashcards
Benign or Malignant Tumors
Benign or Malignant Tumors
Signup and view all the flashcards
Inflammatory Causes
Inflammatory Causes
Signup and view all the flashcards
Vascular Conditions
Vascular Conditions
Signup and view all the flashcards
Radicular Pain
Radicular Pain
Signup and view all the flashcards
Red Flag Symptoms
Red Flag Symptoms
Signup and view all the flashcards
Neurological Examination
Neurological Examination
Signup and view all the flashcards
L3,L4 Myotomal areas
L3,L4 Myotomal areas
Signup and view all the flashcards
Sciatic Nerve Stretch Test
Sciatic Nerve Stretch Test
Signup and view all the flashcards
Reverse straight leg test
Reverse straight leg test
Signup and view all the flashcards
Investigations
Investigations
Signup and view all the flashcards
Surgical treatment
Surgical treatment
Signup and view all the flashcards
Lumbar Disc Herniation
Lumbar Disc Herniation
Signup and view all the flashcards
Lumbar Spine Considerations
Lumbar Spine Considerations
Signup and view all the flashcards
Cervical spine Root Mismatch
Cervical spine Root Mismatch
Signup and view all the flashcards
Findings by X-Ray
Findings by X-Ray
Signup and view all the flashcards
Nonoperative Treatment
Nonoperative Treatment
Signup and view all the flashcards
Rest
Rest
Signup and view all the flashcards
Operative Treatment
Operative Treatment
Signup and view all the flashcards
Spinal Instability Symptoms
Spinal Instability Symptoms
Signup and view all the flashcards
L1 & L2 Myotomal area
L1 & L2 Myotomal area
Signup and view all the flashcards
Lasègue' Sign
Lasègue' Sign
Signup and view all the flashcards
Causes of Radiculopathy
Causes of Radiculopathy
Signup and view all the flashcards
Diagnostic tools
Diagnostic tools
Signup and view all the flashcards
Herniation Treatment
Herniation Treatment
Signup and view all the flashcards
Disc Herniation Location
Disc Herniation Location
Signup and view all the flashcards
Surgical intervention
Surgical intervention
Signup and view all the flashcards
Lumbar spine
Lumbar spine
Signup and view all the flashcards
Canal Narrowing
Canal Narrowing
Signup and view all the flashcards
Spontaneous Resolution
Spontaneous Resolution
Signup and view all the flashcards
Cauda Equina Syndrome
Cauda Equina Syndrome
Signup and view all the flashcards
Lumbar Spondylolisthesis
Lumbar Spondylolisthesis
Signup and view all the flashcards
Study Notes
- Surgery covers lumbar disc diseases, lumbosacral radiculopathy, including: definition, causes, symptoms, and treatments; costing 10 LE at Level 4.
Lumbosacral Radiculopathy
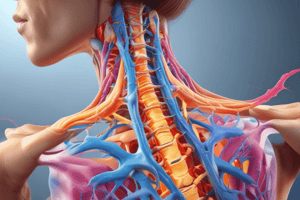
- A disorder of the spinal nerve roots from L1-S4
- Caused by compression, irritation, or stretching of the nerve roots which exit the spine
- Can result in radiating pain, tingling, numbness, paraesthesia, occasional shooting pain, motor weakness, and reflex changes
- Radiculopathy is a complex of symptoms from nerve root pathology, including pain, anesthesia, paresthesia, hypoesthesia, motor, and/or reflex changes
- Radicular pain can arise from one or more spinal nerve roots
Common Causes of Lumbosacral Radiculopathy
- Lesions of the intervertebral discs
- Degenerative disease of the spine
Causes of Radicular Symptoms
- Any process that irritates, compresses, or stretches the spinal nerves
Degenerative Conditions of the Spine
- Spondylosis
- Spondylolisthesis
- Spinal canal stenosis
- Lumbar disc herniation
Trauma
- Motor vehicle accident
- Falling from a height
- Pathological fracture
- Osteoporosis
Tumors
- Benign or malignant tumors (primary spinal tumors like Schwannoma, Neurofibroma, Lymphoma, Osteoblastoma, Meningioma)
- Secondary metastatic tumors are more common
Inflammatory Conditions
- Spondylodiscitis
- Epidural abscess
- Fungal infections
- Tuberculosis (TB)
Vascular Conditions
- Arteriovenous malformations (AVM)
History and Symptoms
- History and physical exams are crucial in diagnosing lumbosacral radiculopathy
- Pain is the most common symptom
- Radicular pain presents as electrical shocks or shooting pains that radiate from the buttock to the foot
- Numbness or weakness along the distribution supplied by the respective nerve root(s) are often noted
Red Flag Symptoms
- Could indicate an urgent clinical condition
- Age over 55 years
- Fever or unexplained weight loss and night sweats
- History of significant trauma
- Bowel or bladder dysfunction and saddle anesthesia
- Malignancy (previous surgeries, chemo or radiation therapy, or a history of metastatic disease)
- Significant medical comorbidities
- Progressive neurologic deficit on serial exam
Physical Examination
- General examination includes vital signs, color signs, red flag signs, and other system exams
- Neurological examination includes sensory, motor, and gait exam with assessment for upper motor neuron findings (Babinski sign, Clonus, Spasticity)
Nerve Root Examination
- L1 affects the inguinal region and hip flexors
- L2 affects the anterior mid-thigh and hip flexors
- L3 affects the distal anterior thigh, impacts hip flexors and knee extensors
- L4 affects the medial lower leg and foot, knee extensors, ankle dorsiflexors and patellar reflex
- L5 affects the lateral leg and foot, hallux extension, ankle plantar flexors and Achilles reflex, and diminished or absent Achilles reflex
- S1 affects the lateral side of the foot, ankle plantar flexors, evertors and Achilles reflex
Nerve Root Stretch Signs
- Sciatic nerve stretch test, (Lasègue test/straight leg raising test) where passively raising one leg increases tension on the sciatic nerve between 30 to 60 degrees
- Reproduction of symptoms between 30°-60° suggests lower lumbar nerve root involvement between L4 to S1
- Femoral nerve stretch test, reverse straight leg or Ely test–Slump test is where extending the hip and flexing the knee with patient prone reproduces pain by stretching the femoral nerve and the L2-L4 nerve roots.
- Slump test can reproduce radicular symptoms by placing the patient seated with neck in full flexion and knees in full extension
Investigations
- Lumbosacral Plain X-ray
- CAT scan lumbosacral
- Lumbosacral MRI
- Dexa Bone scan isotopes bone scan
- Laboratory tests in red flag signs
- EMG & NCV (nerve conduction velocity)
Surgical Treatment
- In refractory cases, surgical decompression of the nerve root from offending pathology
- Fusion and instrumentation can be used if there are signs of instability
Surgical Treatments for Specific Conditions
- Lumbar disc herniation is treated with lumbar discectomy
- Lumbar canal stenosis is treated with decompressive laminectomy
- Lumbar spondylolisthesis is treated with lumbar fixation
- Spinal tumors and metastasis are treated with tumor excision
- Spondylodiscitis is treated with evacuation of abscess and debridement
Lumbar Disc Herniation
- Displacement of the nucleus pulposus of the intervertebral disc, which may compress traversing nerve roots or exiting nerve roots within the spinal canal
Anatomical Considerations
- Vertical anatomy of the lumbar nerve root where paracentral and foraminal disc issues will affect different nerve roots, unlike horizontal anatomy of the cervical nerve root
- In the lumbar spine, nerve roots exit below the corresponding pedicle
- A posterolateral lumbar disc herniation (L4-L5) compresses the traversing nerve root (L5)
- Foraminal lumbar disc prolapse (L4-5) compresses (L4)
Key Difference Between Cervical and Lumbar Spine Nerve Root
- Cervical spine C6 nerve root travels under C5 pedicle (mismatch)
- Lumbar spine L5 nerve root travels under L5 pedicle (match)
- C8 nerve root (NO C8 pedicle) allows transition
Horizontal (Cervical) vs. Vertical (Lumbar) Anatomy of Nerve Roots
- Vertical anatomy of lumbar nerve root where a paracentral and foraminal disc will affect different nerve roots
- Because of horizontal anatomy of cervical nerve root where central and foraminal discs will affect the same nerve root
- Exception: Lumbarized or sacralized vertebrae, conjoined lumbar nerve roots, far lateral disc herniation
Intervertebral disc
- Consists of 1) inner nucleus pulposus (NP), 2) outer annulus fibrosus (AF) which maintains the NP within the center of the disc, and 3) cartilaginous endplate
The Central NP
- A site of collagen secretion
- Contains numerous proteoglycans (PG), which facilitate water retention, creating hydrostatic pressure to resist axial compression of the spine
- Primarily composed of type II collagen, which accounts for 20% of its overall dry weight
Epidemiology
- Lumbar Disc Herniation is a very common cause of low back pain and radicular leg pain,
- Incidence rate of 80% of the population sustaining an episode of low back pain (LBP) once during their lifetime
- 80% will improve in short period without cost of imaging or surgery
- Lifetime prevalence of 10%
Age and Sex
- Peak incidence is 4th and 5th decades with a 3:1 male to female ratio
Level
- Commonly affects the L4-L5 & L5-S1 levels
Pathophysiology of Disc Herniation
- Changes in the biology of the intervertebral disc are thought to contribute
- Involves recurrent torsional strain and tears of the outer annulus, leading to herniation of the nucleus pulposus
- Includes reduced water retention in the NP and increased percent of type I collagen within the NP & inner AF
- Herniation is usually unilateral due to the lack of support by the posterior longitudinal ligament
Herniation Zones
- Central prolapse
- Paracentral
- Foraminal
- Extraforaminal
Classification
- Location: central prolapse, paracentral, foraminal, extraforaminal
- Anatomic: protrusion, extrusion, sequestered fragment (free)
- Onset: acute disc herniation, chronic disc herniation
Location Classification Details
- Central prolapse involves back pain and cauda equina syndrome
- Posterolateral (paracentral) is most common, where PLL is weakest, affecting the traversing/descending/lower nerve root, specifically L4/5 affects L5 nerve root
- Foraminal location affects the exiting nerve root
- Extraforaminal is less common (5-10%), where L4/5 affects L4 nerve root and herniated disc material directly compresses dorsal root ganglion
- Axillary which may affect both exiting and descending nerves
Anatomic Classification Details
- Protrusion is eccentric bulging with an intact annulus
- Extrusion is disc material herniates through annulus but remains continuous with disc space
- Sequestered fragment (free) herniates through annulus and is not continuous with disc space
Symptoms of Injury in the Clinical Picture
- Axial back pain (low back pain) may be discogenic or mechanical in nature
- Radicular pain (buttock and leg pain) symptoms worsen with sitting, coughing, Valsalva, sneezing, and improve with standing
- Weakness in the affected myotomes may occur
- Cauda equina syndrome (present in 1-10%)
- Bilateral leg pain, LE weakness, saddle anesthesia, bowel and bladder symptoms are emergent
Cauda Equina Syndrome
- Dysfunction of multiple lumbar & sacral nerve roots within the lumbar canal due to massive lumbar disc herniation, infection tumor or trauma
- Its an urgent neurological condition
- Low back pain and severe sciatica are usually bilateral
- Urine retention or incontinence, saddle anesthesia, significant motor weakness, and sexual dysfunction
Physical Examination for Radiculopathy
- L2 radiculopathy is associated with hip flexor weakness
- L3 radiculopathy is associated with hip adduction and knee extension weakness
- L4 radiculopathy involves ankle dorsiflexion weakness where L4 is greater than L5, and decreased patellar reflex
- L5 radiculopathy involves EHL weakness and manual testing ankle dorsiflexion weakness; test patient by having them walk on heels ankle inversion weakness
- S1 radiculopathy is associated with ankle plantar flexion weakness and decreased Achilles tendon reflex
Provocative Tests- Straight Leg Raise (SLR)
- Tension sign for L5 and S1 nerve root
- Technique can be performed sitting or supine while hip flexion is the identifying factor
- Contralateral SLR is less sensitive but more specific
- Lasègue' sign and SLR aggravated by forced ankle dorsiflexion
- Bow string sign and SLR aggravated by compression on popliteal fossa
- Kernig test involves pain reproduced with neck flexion, hip flexion, and leg extension
- Naffziger test involves pain reproduced by coughing
- Milgram Test involves pain reproduced with straight leg elevation for 30 seconds
- Trendelenburg Test which involves gluteus Medius weakness
- FABER test is Flexion, Abduction, external rotation that is markedly positive in presence of hip joint disease, trochanteric bursitis, and Sacroiliitis
Investigation
- Radiographs of A-P, Lateral, Dynamic and Oblique
- Findings: loss of normal lumbar lordosis (spasm), loss of disc height, lumbar spondylosis (degenerative changes), Lumbar spondylolisthesis
- Lumbosacral CAT scan provides more details about bony anatomy
Indications
- Plain x-ray lumbar sacral spine and pain lasting over a month
- Pain not responding to nonoperative management
- Red flag signs are present
- Highly sensitive and specific and helpful for preoperative planning
- MRI with gadolinium: Useful for revision surgery that allows to distinguish between post- surgical fibrosus (enhances with gadolinium) vs. recurrent herniated disc (does not enhance with gadolinium)
Nonoperative Treatment
- First line of treatment for most patients with disc lumbar herniation
- 80% improve in symptoms within 3 months with nonoperative care
- Size of herniation decreases over time and will reabsorbed sequestered disc herniations show the greatest degree of spontaneous reabsorption.
Non Operative Treament Elements
- Bedrest: Bedrest followed by progressive activity as tolerated
- Medication: Includes NSAIDs, muscle relaxants, Steroidal anti-inflammatory medications, Opioid analgesics
- Physical therapy: Involves Traction & extension exercises extremely beneficial
- Intervention procedures: Involves Steroid injection or Radiofrequency
Selective Nerve Root Corticosteroid Injections
- Second line of treatment if medications fail, use epidural, selective nerve block which leads to long lasting improvement in ~ 50% (compared to ~90% with surgery)
Operative Treatment
- Indicated for Progressive disabling pain that has failed nonoperative management, Progressive neurological deficits, or Cauda equina syndrome
Surgical Options
- Open Lumbar Laminectomy and discectomy
- Lumbar Microdiscectomy, fenestration and foraminotomy
- Lumbar Endoscopic discectomy
- Lumbar Discectomy with fusion and instrumentations
- Lumbar Far lateral microdiscectomy
- Lumbar Disc replacement surgery
- Varied depending on what causes the lumbar radiculopathy
- The treatments involve either decompressing the nerve or stabilizing the spine
Techniques of Lumbar Discectomy
- Varied elements
- Position: Prone position under general or spinal anesthesia
- Incision of the skin, lumbar fascia & separation of paravertebral muscles
Outcome
- 70%-90% Success rate
- Depends on degenerative factors, stenotic factors and instability factors
Complication of Lumbar Discectomy
- Dural tear (1%)
- Nerve root injury
- Incomplete decompression & residual HLD
- Missed level
- Discitis (1%)
- Lumbar instability
- Chronic low back pain & arachnoiditis
- Vascular catastrophe: injury to the vena cava, iliac arteries or aorta
- Endoscopic Lumbar Discectomy
Lumbar Spine Fusion & Instrumentation Types
- Posterior Lumbar Interbody Fusion (PLIF)
- Transforaminal Lumbar Interbody Fusion (TLIF)
- Anterior lumbar interbody fusion (ALIF), involves pedicle screws and Lumbar Cage Implantation
Lumbar Canal Stenosis
- Narrowing of the lumbar canal diameter
- Compression of lumbar nerve roots, resulting in nerve root ischemia.
- Clinical presentation with Neurogenic claudication pain and Decompressive laminectomy with or without fusion and instrumentations as a type of Treatment
Lumbar Spondylolisthesis
- Forward displacement of one vertebra over the other.
- Causes include degenerative spondylosis, spinal trauma, congenital defects, spondylodiscitis, and iatrogenic (previous lumbar laminectomy)
- Causes Instability of the spinal segment which leads to chronic Low back pain and radiculopathy
- Treated with surgical fixation & fusion of the spine
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.