Podcast
Questions and Answers
What is the primary mechanism of action of lidocaine as a local anesthetic?
What is the primary mechanism of action of lidocaine as a local anesthetic?
- Acetylcholine receptor antagonist
- Ca2+ channel blocker
- K+ channel blocker
- Na+ channel blocker (correct)
Which of the following is a common side effect of local anesthetics like lidocaine?
Which of the following is a common side effect of local anesthetics like lidocaine?
- Seizures (correct)
- Headaches
- Coughing
- Nausea and vomiting
Which regional anesthesia technique involves injecting anesthetic into the epidural space?
Which regional anesthesia technique involves injecting anesthetic into the epidural space?
- Peripheral nerve block
- Spinal block
- TAP block
- Epidural block (correct)
What is one advantage of using an epidural for anesthesia?
What is one advantage of using an epidural for anesthesia?
Which local anesthetic is often used in dental procedures?
Which local anesthetic is often used in dental procedures?
In which scenario would you typically consider using peripheral nerve blocks?
In which scenario would you typically consider using peripheral nerve blocks?
What type of anesthetic approach allows for patient-controlled analgesia?
What type of anesthetic approach allows for patient-controlled analgesia?
Which local anesthetic is known for a longer duration of action and is often used in surgery?
Which local anesthetic is known for a longer duration of action and is often used in surgery?
What is the primary mechanism by which general anesthesia achieves its effects?
What is the primary mechanism by which general anesthesia achieves its effects?
Which neurotransmitter is classified as an excitatory neurotransmitter involved in general anesthesia?
Which neurotransmitter is classified as an excitatory neurotransmitter involved in general anesthesia?
In the context of IV anesthetics, what does the term 'context sensitive half-time' refer to?
In the context of IV anesthetics, what does the term 'context sensitive half-time' refer to?
Which drug is noted for having a dissociative anesthetic effect by acting on the NMDA receptor?
Which drug is noted for having a dissociative anesthetic effect by acting on the NMDA receptor?
What side effect is commonly associated with the use of Ketamine?
What side effect is commonly associated with the use of Ketamine?
What risk factor is associated with a decline in anesthesia-related mortality since the 1940s?
What risk factor is associated with a decline in anesthesia-related mortality since the 1940s?
Which type of anesthetic is delivered through a breathing tube into the lungs?
Which type of anesthetic is delivered through a breathing tube into the lungs?
What effect do opioids typically have when used in maintenance anesthesia?
What effect do opioids typically have when used in maintenance anesthesia?
What characterizes deep sedation compared to light sedation in terms of responsiveness?
What characterizes deep sedation compared to light sedation in terms of responsiveness?
Which of the following is a common side effect of benzodiazepines at high doses?
Which of the following is a common side effect of benzodiazepines at high doses?
Which type of sedation requires a breathing device to maintain airway patency?
Which type of sedation requires a breathing device to maintain airway patency?
What is the primary action mechanism of benzodiazepines?
What is the primary action mechanism of benzodiazepines?
What physiological change is associated with deep sedation regarding cardiovascular function?
What physiological change is associated with deep sedation regarding cardiovascular function?
What is the primary use of naloxone?
What is the primary use of naloxone?
Which of the following is a side effect of naloxone?
Which of the following is a side effect of naloxone?
What type of medication is commonly administered orally for sedation purposes?
What type of medication is commonly administered orally for sedation purposes?
Which drug class does fentanyl belong to?
Which drug class does fentanyl belong to?
Which sedative is known for its rapid onset and pleasant dreams?
Which sedative is known for its rapid onset and pleasant dreams?
What is the mechanism of action of morphine?
What is the mechanism of action of morphine?
What intervention is required for a patient experiencing bradycardia due to sedation?
What intervention is required for a patient experiencing bradycardia due to sedation?
What is a primary concern when prescribing higher opioid doses?
What is a primary concern when prescribing higher opioid doses?
What is the intended purpose of the harm reduction strategy involving naloxone?
What is the intended purpose of the harm reduction strategy involving naloxone?
What type of anesthesia can be achieved using local anesthetics?
What type of anesthesia can be achieved using local anesthetics?
What is a misconception about mixing hydromorphone with acetaminophen and naproxen?
What is a misconception about mixing hydromorphone with acetaminophen and naproxen?
Flashcards
What is Regional Anesthesia used for?
What is Regional Anesthesia used for?
Regional anesthesia is a type of anesthesia that numbs a specific area of the body. It is used for both post-operative pain relief and pain management during labor.
What is Regional Anesthesia?
What is Regional Anesthesia?
Regional anesthesia is a type of anesthesia that numbs a specific area of the body, typically by injecting a local anesthetic near the nerves that supply that area.
Epidural Anesthesia
Epidural Anesthesia
Epidural anesthesia involves injecting a local anesthetic into the epidural space, which surrounds the spinal cord. This provides pain relief to a larger area of the body.
Lidocaine: MOA
Lidocaine: MOA
Signup and view all the flashcards
Why use Epidural Anesthesia?
Why use Epidural Anesthesia?
Signup and view all the flashcards
Local Anesthesia: Examples
Local Anesthesia: Examples
Signup and view all the flashcards
Lidocaine Toxicity
Lidocaine Toxicity
Signup and view all the flashcards
What is Spinal Anesthesia?
What is Spinal Anesthesia?
Signup and view all the flashcards
Opiate Analgesics
Opiate Analgesics
Signup and view all the flashcards
Fentanyl
Fentanyl
Signup and view all the flashcards
Naloxone (Narcan)
Naloxone (Narcan)
Signup and view all the flashcards
What is the difference between Light Sedation and Deep Sedation?
What is the difference between Light Sedation and Deep Sedation?
Signup and view all the flashcards
Opioid Overdose Risk Factors
Opioid Overdose Risk Factors
Signup and view all the flashcards
What's the primary action of benzodiazepines?
What's the primary action of benzodiazepines?
Signup and view all the flashcards
Name two common benzodiazepines used for sedation.
Name two common benzodiazepines used for sedation.
Signup and view all the flashcards
Regional Anesthesia
Regional Anesthesia
Signup and view all the flashcards
Conscious Sedation
Conscious Sedation
Signup and view all the flashcards
What's a possible side effect of high benzodiazepine doses?
What's a possible side effect of high benzodiazepine doses?
Signup and view all the flashcards
General Anesthesia
General Anesthesia
Signup and view all the flashcards
What is propofol's mechanism of action?
What is propofol's mechanism of action?
Signup and view all the flashcards
Risk Stratification
Risk Stratification
Signup and view all the flashcards
What's the key difference between propofol use with and without other anesthetic?
What's the key difference between propofol use with and without other anesthetic?
Signup and view all the flashcards
What are some procedures where sedation is often used?
What are some procedures where sedation is often used?
Signup and view all the flashcards
What are the two main types of sedation?
What are the two main types of sedation?
Signup and view all the flashcards
Induction Phase
Induction Phase
Signup and view all the flashcards
Maintenance Anesthesia
Maintenance Anesthesia
Signup and view all the flashcards
Emergence Phase
Emergence Phase
Signup and view all the flashcards
Context Sensitive Half-Time
Context Sensitive Half-Time
Signup and view all the flashcards
GABA
GABA
Signup and view all the flashcards
NMDA Antagonist
NMDA Antagonist
Signup and view all the flashcards
Dissociative Anesthesia
Dissociative Anesthesia
Signup and view all the flashcards
Anesthesia-Related Mortality
Anesthesia-Related Mortality
Signup and view all the flashcards
Study Notes
Good Drugs, Bad Drugs & Anesthesia Part II
- Presented by Dr. Tonia Timperley Tauh MD FRCPC
- Contact information provided
Last Lecture Good Drugs Bad Drugs Part I
- Pain Management:
- Non-opiate analgesia
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Acetaminophen
- Methocarbamol
- Opiates analgesia
Drug: Fentanyl/Morphine
- Class: Opiates
- Mechanism of Action (MOA): Calcium channel blocker
- Uses: Analgesia, additive anesthesia, sedation
- Side Effects: (List incomplete)
Side Effects of Hydrocodone
- Central Nervous System: Drowsiness, dizziness, lightheadedness, fuzzy thinking, anxiety, abnormally happy or sad mood
- Skin: Rash, itching
- Respiratory: Slowed or irregular breathing, chest tightness
- Throat: Dryness
- Gastrointestinal: Nausea, vomiting
- Urinary: Difficulty urinating
- Intestinal: Constipation
Illegal Drug Overdose Deaths in BC (Figure 1)
- Data presented for the years 1991-2017
- Shows a significant increase in overdose deaths over time
- Death rate per 100,000 population is presented
Predictors of Fatal and Nonfatal Opioid Overdose
- Increased Risk Factors
- Higher opioid dose
- Three or more prescribers
- Four or more dispensing pharmacies
- Prescription of fentanyl
- Current substance abuse
- Mental health diagnoses (depression, bipolar disorder)
- Pancreatitis
Case #2
- 35-year-old female, 4 days post motor vehicle accident surgery
- Prescribed Hydromorphone (Dilaudid)
- Patient takes acetaminophen, naproxen, and hydromorphone, and brother suggests it is dangerous to mix these drugs
- Question: Is mixing these drugs dangerous?
Opiate Antagonist: Naloxone (Narcan)
- Mechanism of Action: Binds onto the opiate mu receptor with high affinity, reversing depressed respiration
- Use: Reverses opioid overdose
- Side effects: Reverses analgesia
- Mechanism of action: Reverses opioid overdose from its stronger affinity to opioid receptors
Drug: Naloxone
- Class: Opioid antagonist
- Mechanism of Action (MOA): Binds to the opioid mu receptor with high affinity, displacing opioids, rapidly reverses any molecules occupying the mu receptor
- Use: Reverses respiratory depression, treats opioid-induced pruritis
- Side Effects: Reverses analgesia
Objectives
- Local anesthetic
- Regional anesthesia
- Sedation anesthetic (Conscious Sedation)
- General anesthetic
Good Drugs or Bad Drugs?
- All good drugs have bad ways to use them
- All bad drugs have good ways to use them
- Use information about risks to stratify.
WebMD (Humor)
- A humorous take on the potential for exaggeration in medical information
Local Anesthetic
- Mechanism of action: Blocks the propagation of nerve action by blocking sodium channels
- Examples:
- Cocaine
- Lidocaine
- Prilocaine
- Bupivacaine
Regional Anesthesia
- Involves injecting local anesthetic to block a large area of the body, such as an arm or leg.
- This avoids the need for general anesthesia
- Used for surgical anesthesia, post-operative pain and labor analgesia
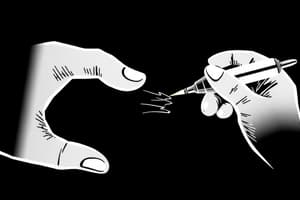
Mechanism of Action: Diagrams
- Diagrams illustrating the processes of pain transmission and the blocking effect of anesthetic
Local Anesthetic: Specifics
- Lidocaine – sodium channel blocker.
- Prevents propagation of nerve action
Regional Anesthesia - Epidural vs Spinal
- Diagram comparing and contrasting epidural and spinal anesthesia.
- Locations
- Techniques used
Regional Anesthesia - Epidural
- A form of regional anesthesia
- Involves injection of local anesthetic and/or opiates into the epidural space
- Uses: Continuous analgesia for labor pain, post operative pain after abdominal or chest surgery
Regional Anesthesia - Types
- Spinal
- Epidural
- Peripheral Nerve blocks
- TAP block
- Digital ring block
Why Epidural?
- Pain control intra and post operative care
- Use less general anesthetic
- An infusion or patient-controlled analgesia
- Use less opiates systemically
- Less side effects like constipation sedation and respiratory depression
Question
- 46-year-old female for a tooth extraction.
- What is the mechanism of action of lidocaine?
- What are some local anesthetic toxicity signs and symptoms?
Drug: Lidocaine/Cocaine
- Class: Local anesthetic
- Mechanism of Action (MOA): Sodium channel blocker
- Uses: Local or regional anesthetic for procedures like dental work, surgery, labor, and pain management.
- Side Effects: Seizures, arrhythmia, and complete heart block
A 34-year-old Gorilla Health Check Up (Humour)
Common Questions Before Anesthesia
- Patient concerns about dying or having pain during anesthesia.
- Asking about procedures regarding alertness and possible allergies.
- Knowing the guidelines of whether food or drink is allowed.
- Desired level of anesthesia needed.
Light, Deep, General Sedation
- Table comparing light, deep, and general sedation levels based on responsiveness, airway, respiration, ventilation, and cardiovascular function
- Responsiveness: Normal response to commands, purposeful response to pain, no response to pain
- Airway: Unaffected, mildly collapsed, no intervention, breathing device needed
- Respiration & Ventilation: Spontaneous breathing, slow deep breaths needing supplemental oxygen, inadequate breathing requiring mechanical ventilation or assisted breathing
- Cardiovascular Function: Normal, bradycardia, hypotension, impaired function requiring pharmacological support
Sedation via Oral or IV
- Explain sedation may be via oral medication or intravenous (IV) medication
Benzodiazepines
- Mechanism of action: Benzodiazepine-receptor binding enhances the inhibitory effects of various neurotransmitters (e.g., GABA)
- Examples:
- Oral: Ativan (lorazepam), oxazepam
- IV: Midazolam
- Side effects: Respiratory depression at high doses
When You Go to Your Dentist, Endoscopy, Colonoscopy, etc
- Discuss anxiety and the benefit in having sedation during these procedures.
Propofol
- Mechanism of Action: Facilitation of inhibitory neurotransmission mediated by GABA
- Rapid Onset & Pleasant Dreams - pleasant experience is possible
- Side Effects: Burns on injection, hypotension, bradycardia
Risks of Dying Under Anesthesia
- Historical risks (e.g., 1940s 1:1000, 2010s 1:1.1 million per year)
- Factors like surgical technique, anesthetic techniques, monitoring and preoperative assessment
1987 - Saturation Probe & Present Day
- Show and compare older style and present day equipment for monitoring patients.
Cardiac Surgery Anesthesia
Anesthesia-Related Mortality
- Epidemiology of Anesthesia-related Mortality; United States (1999-2005) data.
- Rates presented; rates for males, females, hospital discharges and based on age groups.
- Transport Canada Fatal Collision data including rates for 2017.
Questions?
- Contact information provided for Dr. Tonia Timperley Tauh.
- Disclaimer related to the content provided.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.