Podcast
Questions and Answers
What factor significantly decreased mortality rates associated with pyogenic hepatic abscesses starting in the mid-20th century?
What factor significantly decreased mortality rates associated with pyogenic hepatic abscesses starting in the mid-20th century?
- Routine use of percutaneous aspiration.
- Development of more potent anti-sepsis medications.
- Increased use of liver resections.
- Routine surgical drainage and IV antibiotics. (correct)
Which of the following patient characteristics is NOT typically associated with amebic liver abscesses?
Which of the following patient characteristics is NOT typically associated with amebic liver abscesses?
- Male gender
- Advanced age (correct)
- History of travel to endemic areas.
- Poor living conditions
What is the primary mechanism by which Entamoeba histolytica causes tissue damage in amebic liver abscesses?
What is the primary mechanism by which Entamoeba histolytica causes tissue damage in amebic liver abscesses?
- Release of toxins that induce widespread inflammation.
- Obstruction of the portal vein leading to ischemic necrosis.
- Lysis of tissues by trophozoites through cell adherence and activation. (correct)
- Direct bacterial infection of the liver tissue.
A patient with a pyogenic liver abscess is not a surgical candidate and refuses invasive procedures. What is a reasonable treatment approach?
A patient with a pyogenic liver abscess is not a surgical candidate and refuses invasive procedures. What is a reasonable treatment approach?
Which of the following best describes the appearance of hepatic amebic abscess material upon aspiration?
Which of the following best describes the appearance of hepatic amebic abscess material upon aspiration?
What is a key reason why early estimates of amebiasis prevalence were unreliable?
What is a key reason why early estimates of amebiasis prevalence were unreliable?
In what regions is amebiasis considered a significant health problem?
In what regions is amebiasis considered a significant health problem?
What is the role of antiamebic IgA antibodies in the progression of amebic liver disease?
What is the role of antiamebic IgA antibodies in the progression of amebic liver disease?
Which of the following factors is associated with a poor outcome in patients with hepatic pyogenic abscess?
Which of the following factors is associated with a poor outcome in patients with hepatic pyogenic abscess?
What is typically the first step in the pathogenesis of amebiasis following ingestion of Entamoeba histolytica cysts?
What is typically the first step in the pathogenesis of amebiasis following ingestion of Entamoeba histolytica cysts?
Flashcards
Pyogenic Hepatic Abscess Risk factors
Pyogenic Hepatic Abscess Risk factors
In contrast to pyogenic hepatic abscesses, pyogenic liver abscesses tend to affect Hispanic men, aged 20 to 40, with a history of travel to or origination from an area of poverty and cramped living conditions are associated with an increased risk of infection.
Amebiasis
Amebiasis
Amebiasis is a disease largely found in tropical and developing countries; however, it can pose a problem in developed countries due to immigration and travel. Areas that are endemic include Mexico, India, Africa, and parts of Central and South America.
Antiamebic antibodies
Antiamebic antibodies
Antiamebic antibodies develop approximately 7 to 10 days after the onset of disease or an amebic hepatic abscess. IgA antibodies have been shown to inhibit adherence of amebic trophozoites to colonic epithelium in vitro.
Hepatic Amebic Abscess
Hepatic Amebic Abscess
Signup and view all the flashcards
Hepatic Amebic Abscess Progression
Hepatic Amebic Abscess Progression
Signup and view all the flashcards
Pyogenic Hepatic Abscess Mortality
Pyogenic Hepatic Abscess Mortality
Signup and view all the flashcards
Poor Prognosis Factors (Pyogenic)
Poor Prognosis Factors (Pyogenic)
Signup and view all the flashcards
Severe Infection Signs
Severe Infection Signs
Signup and view all the flashcards
E. histolytica
E. histolytica
Signup and view all the flashcards
Study Notes
- Study notes on Liver Abscesses
Treatment Options and Outcomes for Pyogenic Hepatic Abscess
- Percutaneous catheter drainage has a higher success rate (100%) vs. aspiration
- Aspiration has a success rate of 60%
- Success rates were similar between aspiration alone and aspiration plus catheter drainage, in terms of treatment success rate, hospital stay, antibiotic duration, and mortality
- The aspiration-only group required more aspirations than the catheter drainage group, with 40% needing two aspirations and 20% needing three
- Catheter drainage is the preferred treatment, but an initial single aspiration is worth considering
- Some reports show success with antibiotics alone, but most of these patients had a diagnostic aspiration or partial drainage
- Antibiotic treatment without drainage may result in high mortality (59%-100%)
- For patients not fit for surgery or refusing invasive procedures, antibiotic treatment may be attempted but isn't generally recommended
- Liver resection is occasionally needed, such as for infected hepatic malignant neoplasms, hepatolithiasis, or intrahepatic biliary stricture; some patients may benefit from resection if there is severe hepatic destruction
Trends in Mortality
- Mortality from pyogenic hepatic abscess has greatly decreased in the last 70 years
- Before the use of surgical drainage, the condition was uniformly fatal
- Surgical drainage and IV antibiotics reduced mortality to around 50% until the early 1980s
- Since the 1980's mortality rates have fallen to 10% to 20%
- The 1990s saw mortality below 10%
- Memorial Sloan-Kettering Cancer Center (MSKCC) reported a 3% mortality in their recent series
Factors Affecting Prognosis
- Presence of malignant disease
- Factors linked to malignant disease (e.g., jaundice, high LFT results)
- Signs of sepsis all indicate a poor prognosis
- Chronic disease signs like hypoalbuminemia often indicate a poor outcome
- Severe infection signs: leukocytosis, Acute Physiology and Chronic Health Evaluation II (APACHE II) scores, abscess rupture, bacteremia, and shock indicates mortality
- Two thirds of percutaneous and surgical case series show effective success and mortality rates
Amebic Abscess Epidemiology
- Amebiasis is a common disease in tropical and developing countries
- It is also an issue in developed countries with significant immigration and travel
- Common in Mexico, India, Africa, and parts of Central and South America
- The World Health Organization (WHO) estimated 40 to 50 million people in 1995 had amebic colitis or liver abscess and that resulted in 40,000 to 100,000 deaths each year
- Previous estimates didn't differentiate between E. histolytica (pathogenic) and Entamoeba dispar (nonpathogenic)
- Male homosexuals, previously thought to be frequently infected with E. histolytica, actually have E. dispar
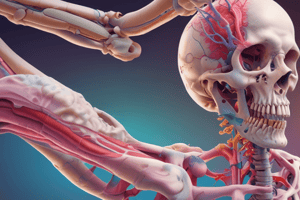
Amebic Abscess Pathogenesis
- E. histolytica is a protozoan within the Entamoeba genus
- Not all E. histolytica strains are pathogenic
- Ingestion of E. histolytica cysts causes amebiasis through contaminated water, vegetables, or human contact
- Cysts pass to the intestines and then to the colon, infecting the mucosa
- Trophozoites thought to enter the portal venous system, causing necrosis by lysing tissues through cell adherence, activation, and protein hydrolysis
- This process results in localized hepatic necrosis and accumulating debris with amebic trophozoites
- Early development is associated with these
- Antiamebic antibodies, particularly IgA, are developed, but do not halt progression
- A cell-mediated mechanism is now believed to be key
Amebic Abscess Pathology
- Hepatic amebic abscess is enzymatic necrosis, producing liquefied liver tissue, with the appearance of "anchovy sauce"
- Bacterial infection isn't usually present unless there has been a perforation
- Hydrolysis continues until Glisson's capsule, resistant to this process, is reached, forming a cavity that is typically limited by the peritoneum
- It has no real fibrous capsule
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.