Podcast
Questions and Answers
Which of the following is the primary cause of limb loss in the United States?
Which of the following is the primary cause of limb loss in the United States?
- Cancer
- Vascular disease (correct)
- Congenital abnormalities
- Trauma
What percentage of US adults (18 and older) have diabetes, both diagnosed and undiagnosed?
What percentage of US adults (18 and older) have diabetes, both diagnosed and undiagnosed?
- 8%
- 13% (correct)
- 20%
- 5%
African Americans are how many times more likely than white Americans to have an amputation?
African Americans are how many times more likely than white Americans to have an amputation?
- 2 times
- 3 times
- 4 times (correct)
- 5 times
Which of the following factors is considered an independent predictor for lower extremity amputation in individuals with diabetes?
Which of the following factors is considered an independent predictor for lower extremity amputation in individuals with diabetes?
What is the primary surgical consideration when determining the level of amputation?
What is the primary surgical consideration when determining the level of amputation?
Which of the following best describes a Syme's amputation?
Which of the following best describes a Syme's amputation?
A transfemoral amputation is defined as amputation that occurs:
A transfemoral amputation is defined as amputation that occurs:
What is myodesis in the context of amputation surgery?
What is myodesis in the context of amputation surgery?
In a transtibial amputation, how much shorter is the fibula typically cut compared to the tibia?
In a transtibial amputation, how much shorter is the fibula typically cut compared to the tibia?
What is the primary proposed benefit of the Ertl procedure in transtibial amputations?
What is the primary proposed benefit of the Ertl procedure in transtibial amputations?
What is a potential impact of losing major adductor muscle attachments during a transfemoral amputation, if not addressed surgically?
What is a potential impact of losing major adductor muscle attachments during a transfemoral amputation, if not addressed surgically?
What is the main advantage of osseointegration compared to socket prostheses?
What is the main advantage of osseointegration compared to socket prostheses?
A study comparing osseointegration to socket prostheses found what percentage improvement in TUG values?
A study comparing osseointegration to socket prostheses found what percentage improvement in TUG values?
Which of the following is NOT a primary goal of postoperative dressings after amputation?
Which of the following is NOT a primary goal of postoperative dressings after amputation?
Which type of postoperative dressing is typically NOT used until after sutures are removed?
Which type of postoperative dressing is typically NOT used until after sutures are removed?
An immediate post-operative prosthesis (IPOP) provides excellent edema management and limb protection, but what is a significant disadvantage associated with its use?
An immediate post-operative prosthesis (IPOP) provides excellent edema management and limb protection, but what is a significant disadvantage associated with its use?
Which of the following is included in the postsurgical phase of care?
Which of the following is included in the postsurgical phase of care?
According to the VA/DoD Clinical Practice Guideline (CPG), what is a strong recommendation for rehabilitation of individuals with lower limb amputation?
According to the VA/DoD Clinical Practice Guideline (CPG), what is a strong recommendation for rehabilitation of individuals with lower limb amputation?
According to the VA/DoD CPG, which of the following factors is associated with poorer outcomes following acquired limb loss?
According to the VA/DoD CPG, which of the following factors is associated with poorer outcomes following acquired limb loss?
During the postsurgical phase after an amputation, which of the following is a primary goal related to the residual limb?
During the postsurgical phase after an amputation, which of the following is a primary goal related to the residual limb?
Which of the following is generally contraindicated during the postsurgical phase?
Which of the following is generally contraindicated during the postsurgical phase?
What is a primary goal of proper positioning in the postsurgical phase?
What is a primary goal of proper positioning in the postsurgical phase?
Which of the following is an important component of patient education during the postsurgical phase?
Which of the following is an important component of patient education during the postsurgical phase?
During the postsurgical examination, what is an important element of the 'History' component?
During the postsurgical examination, what is an important element of the 'History' component?
During the postsurgical examination, vital signs are reviewed as part of which examination component?
During the postsurgical examination, vital signs are reviewed as part of which examination component?
In the postsurgical examination, which of the following is assessed under 'Body Structure/Function'?
In the postsurgical examination, which of the following is assessed under 'Body Structure/Function'?
Which intervention is appropriate during the postsurgical phase?
Which intervention is appropriate during the postsurgical phase?
What is a key goal in the preprosthetic phase regarding residual limb care?
What is a key goal in the preprosthetic phase regarding residual limb care?
During transtibial residual limb assessment, where do you measure the length from?
During transtibial residual limb assessment, where do you measure the length from?
What is the definition of telescoping in the context of residual limb assessment?
What is the definition of telescoping in the context of residual limb assessment?
Which of the following is part of preprosthetic phase interventions?
Which of the following is part of preprosthetic phase interventions?
For which stage scar massage and desensitization techniques are appropriate?
For which stage scar massage and desensitization techniques are appropriate?
Which of the following statements is true regarding desensitization techniques?
Which of the following statements is true regarding desensitization techniques?
Which of the following is a good skin care advise for those with a amputation?
Which of the following is a good skin care advise for those with a amputation?
Which of the following can be one of the metabolic costs for ambulation with prosthesis?
Which of the following can be one of the metabolic costs for ambulation with prosthesis?
Which of the following methods are appropriate for peak aerobic capacity testing?
Which of the following methods are appropriate for peak aerobic capacity testing?
What is a current non-pharmacological pain management for amputees?
What is a current non-pharmacological pain management for amputees?
Which of the following best describes augmented reality as a non-pharmacological pain management?
Which of the following best describes augmented reality as a non-pharmacological pain management?
What is a drawback for virtual reality as a non-pharmacological pain management?
What is a drawback for virtual reality as a non-pharmacological pain management?
Flashcards
Objectives of amputation surgery?
Objectives of amputation surgery?
Describe the epidemiology, etiology and risk factors of lower extremity amputation surgery.
Amputation level definition
Amputation level definition
Define the levels of amputation and the surgical procedures associated with each level.
Postoperative dressings
Postoperative dressings
Identify the types of postoperative dressings and their advantages/disadvantages.
Postoperative vs preprosthetic phases
Postoperative vs preprosthetic phases
Signup and view all the flashcards
Postoperative examinations
Postoperative examinations
Signup and view all the flashcards
Phase specific interventions
Phase specific interventions
Signup and view all the flashcards
Limb loss population in the U.S.
Limb loss population in the U.S.
Signup and view all the flashcards
Primary cause of limb loss
Primary cause of limb loss
Signup and view all the flashcards
Diabetes related amputations
Diabetes related amputations
Signup and view all the flashcards
Diabetes Prevalence
Diabetes Prevalence
Signup and view all the flashcards
Independent predictors
Independent predictors
Signup and view all the flashcards
Claudication
Claudication
Signup and view all the flashcards
Critical limb ischemia
Critical limb ischemia
Signup and view all the flashcards
ABPI (ankle-brachial pressure index)
ABPI (ankle-brachial pressure index)
Signup and view all the flashcards
Surgical considerations for amputation
Surgical considerations for amputation
Signup and view all the flashcards
Partial toe amputation
Partial toe amputation
Signup and view all the flashcards
Toe disarticulation
Toe disarticulation
Signup and view all the flashcards
Partial foot/ray resection
Partial foot/ray resection
Signup and view all the flashcards
Transmetatarsal (Lisfranc) amputation
Transmetatarsal (Lisfranc) amputation
Signup and view all the flashcards
Ankle disarticulation (Syme’s)
Ankle disarticulation (Syme’s)
Signup and view all the flashcards
Long transtibial amputation
Long transtibial amputation
Signup and view all the flashcards
Transtibial amputation
Transtibial amputation
Signup and view all the flashcards
Short transtibial amputation
Short transtibial amputation
Signup and view all the flashcards
Knee disarticulation
Knee disarticulation
Signup and view all the flashcards
Long transfemoral amputation
Long transfemoral amputation
Signup and view all the flashcards
Transfemoral amputation
Transfemoral amputation
Signup and view all the flashcards
Short transfemoral amputation
Short transfemoral amputation
Signup and view all the flashcards
Hip disarticulation
Hip disarticulation
Signup and view all the flashcards
Transpelvectomy or hemipelvectomy
Transpelvectomy or hemipelvectomy
Signup and view all the flashcards
Hemicorporectomy
Hemicorporectomy
Signup and view all the flashcards
Principles of amputation surgery
Principles of amputation surgery
Signup and view all the flashcards
Transtibial Bone
Transtibial Bone
Signup and view all the flashcards
Transtibial skin flaps
Transtibial skin flaps
Signup and view all the flashcards
Myofascial
Myofascial
Signup and view all the flashcards
Myoplasty
Myoplasty
Signup and view all the flashcards
Myodesis
Myodesis
Signup and view all the flashcards
Tenodesis
Tenodesis
Signup and view all the flashcards
Ertl procedure
Ertl procedure
Signup and view all the flashcards
Transfemoral surgical options
Transfemoral surgical options
Signup and view all the flashcards
Postoperative Dressings
Postoperative Dressings
Signup and view all the flashcards
Study Notes
LE Amputation Surgery & Postoperative Care
- Objectives include describing the epidemiology, etiology, and risk factors of lower extremity amputation surgery
- Understanding levels of amputation and related procedures
- Identifying postoperative dressings and discussing post and preprosthetic phase goals
Epidemiology/Etiology
- Approximately 2.3 million people in the U.S. are living with limb loss
- 465,000 amputations occur in the U.S. annually
- Vascular disease is the primary cause (54%), including diabetes and PAD, followed by trauma (45%), and CA (<2%)
- Half of vascular disease amputees die within five years
- 55% of diabetics with a lower limb amputation require amputation of the second leg within 2-3 years
- African Americans have four times the amputation risk compared to white Americans
- 13% of US adults (≥18 years) have diabetes (diagnosed and undiagnosed)
- 60% of non-traumatic amputations occur in individuals >20 years with diabetes
- 90% of diabetics undergoing amputation had a pre-existing foot ulcer
Risk Factors for LE Amputation (Diabetics)
- Independent predictors include level of glucose control
- Duration of diabetes, baseline systolic BP, microvascular changes (retinopathy, neuropathy, & nephropathy), and history of stroke
- Non-predictive factors include type of diabetes, cigarette smoking, and total cholesterol
PAD: Symptoms and Signs
- Peripheral artery disease (PAD) usually results from atherosclerosis
- Atherosclerotic plaque causes arterial stenosis or occlusion, reducing blood flow to the limb
- Most patients are asymptomatic
- Many patients experience intermittent claudication (pain on walking)
- Critical limb ischemia is a condition when reduced blood flow causes rest pain/tissue loss
Claudication
- Aching or burning is experienced in the leg muscles
- Pain is reliably reproduced at a distance of walking
- Pain is relieved within minutes on rest
Critical Limb Ischemia
- It involves ulcers or gangrene
- It involves rest pain in foot for over two weeks
- It may be resistant to opiate analgesia
- Hard to differentiate from neuropathy
- Hanging the leg out of bed helps patients find relief
ABPI and PAD
- ABPI of ≤0.9 is diagnostic of PAD
- ABPI of ≤0.5 suggests critical limb ischemia
- Incompressible (ABPI >1.2) values are seen in patients with arterial calcification, notably those with diabetes and/or chronic kidney disease
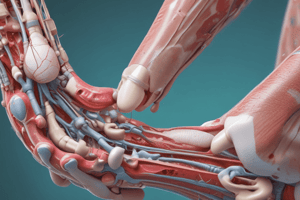
Levels of Amputation
- Surgical considerations include viability of tissue, nature of injury, and post-op function
- Levels include partial toe (excision of any part of one or more toes) and toe disarticulation (at the metatarsal phalangeal joint)
- Partial Foot/Ray Resection includes resection of the 3rd, 4th, 5th metatarsals and digits
- Transmetatarsal (Lisfranc) is an amputation through the midsection of all metatarsals
- Ankle disarticulation (Syme's) involves ankle disarticulation with heel pad attached to distal tibia end
- Long transtibial is >50% of tibia length while transtibial is between 20-50% of tibia length
- Short Transtibial is <20% of tibia length
- Knee disarticulation occurs through the knee joint
- Long transfemoral is >60% of the femoral length; transfemoral is between 30-60% of length
- Short transfemoral is <30% of femoral length; hip disarticulation is through the hip/pelvis
- Transpelvectomy/hemipelvectomy involves resection of part of the pelvis; hemicorporectomy amputates both lower limbs and the pelvis below L4-5
Principles of Surgery
- Involves limb length considerations
- Management of potentially painful neuromas
- Management of severed muscles
Surgical Principles
- Myofascial involves attaching muscle to fascia
- Myoplasty involves attaching anterior and posterior compartment muscles over the end of bone
- Myodesis involves anchoring muscle to bone, and tenodesis involves attaching tendon to bone
- Incisions and management of skin flaps determine residual limb shape
Transtibial Amputation
- Distal ends are beveled for comfort and Fibula is ~1 cm shorter than tibia
- Equal length AP flaps, or a long posterior flap gives improved padding/vascularity
- Bone bridge Ertl procedure
Transtibial Amputation Studies
- TAO (Transtibial Amputation Outcomes) Study
- The Burgess procedure involves a long posterior flap overlapping the distal residual end
- The Ertl procedure includes a bone bridge connecting the distal tibia and fibula
- Ertl procdure may provide a more stable base for prosthetic bearing
Transfemoral Amputation
- Myodesis of the adductor magnus to the femur
- Attachment of major adductor muscles may impact femoral alignment if not addressed
- Myoplasty of the quadriceps and hamstrings is a potential surgical option
- Skin Flaps may be of equal length or a long medial flap (sagittal plane)
Postoperative Dressings
- Goals involve protecting incision and residual limb (RL)
- Facilitating incision healing and managing edema and pain
Postoperative Dressings Types
- Elastic wraps are readily available/accessible; allow incision access, are difficult to don, minimally protect limb, and require frequent reapplication
- Shrinkers are easy to apply and manage edema; not used until after suture removal
- Semirigid dressings better manage edema and protect the limb; require frequent changing
- Removable rigid dressings are effective at edema management and limb protection; they are expensive and needs skilled clinician.
- Immediate post-operative prosthesis (IPOP) offer excellent limb protection and edema management; no incisional access are costly
Phases of Care
- The preoperative phase, the postsurgical phase, and the preprosthetic phase of care are all key
- Postsurgical: It is the period of time between surgery and the discharge from an acute care hospital
- Preprosthetic: It is the time between discharge and fitting of definitive prostheses
VA/DoD CPG
- There is a strong level of evidence to consider the patient's birth sex and self-identified gender identity in individualized treatment plans
- There is strong evidence for instituting rehabilitation training with both open and closed chain exercises and progressive resistance
- Valid, reliable, and responsive functional outcome measures should be used
- Factors that are associated with poorer outcomes following acquired limb loss such as smoking should be assessed
Postsurgical Phase Goals
- Goals include promoting healing of the residual limb by managing RL pain, optimizing ROM, protect remaining limb, provide HEP, encourage independence, and provide patient education & proper positioning to avoid contractures
Postsurgical Examination
- Review history like amputation type and level
- Review the status of residual limb, OOB status, and vital signs (pre and post activity)
- Review respiratory and Integumentary systems
- Neuromuscular system review also take place
- Pain is considered and tested
- Body Structure/Function tested alongside extremity strength, ROM
- Activity Level evaluated (seated/standing) & Functional status are all essential
Postsurgical Phase Interventions
- Includes positioning/AROM of RL
- Functional training is used, along with instruction to protect the RL like minimize pressure/drag
- Balance training of both Standing and seated and ambulation training
- Exercises for intact extremities and maintain strength
- Limb care, both intact and residual is a priority
Preprosthetic Phase Goals
- The goals are independence in residual limb care
- Functional mobility and transfers
- Performing a HEP and managing the uninvolved LE
- Demonstrate cardiorespiratory endurance for prosthetic use
Preprosthetic Examination
- Focuses on psychological/emotional status, amputation history, and associated diseases
- Systems Review includes cardiopulmonary measures, integumentary like skin grafts, neuromuscular measures
- Mental status, RL/phantom pain, sensation/coordination/balance are considered
- Pulses/color/temperature/edema/intermittent claudication are also focused on
Systems Review
- Musculoskeletal exam, ROM, as well as RL hip and knee should be conducted
- Strenght/endurance, and Core strenth are crucial
Residual Limb
- Length and bone vs soft tissue length need to be assessed
- Shape assessment and any abnormalies need reporting
Residual Limb Assesment
- Transtibial - Girth with Medial joint lines every 2-3 inches and length as well
- Transfemoral - Girth from Ischial Tuberosity to greater trochanter. Length and and proximalk landmark to end of bone
Phantom Limb Sensation
- Phantom limb sensation reports that the part of the amputated limb is still there
- "Telescoping" involves feeling the distal end, and not the mid-portion of the phantom limb
- Typically resolves itself within 2-3 years
- Phantom limb pain occurs in ~80% of all amputations
Balance/Mobility Activities
- Balance/Mobility activities of amputation care may include ROM exercises and Psychological Support
- Cardiopulmonary endurance exercises are utilized for rehabiltation
Metabolic costs of ambulation
- It becomes higher with prosthesis use Metabolic costs:
- partial foot: Increased ~15%
- Traumatic transtibial: Increased ~25%
- Vascular transtibial: Increased ~40%
- Traumatic transfemoral: Increased ~68%
- Vascular transfemoral: Increased ~100%
Pain Management
- Non-Pharmacological interventions include Mirror Therapy and TENS(positive effects however poor quality of evidence)
- Acupuncture (positive effects however poor quality of evidence)
- Includes Motor Imagery and Virtual Reality (positive effects however poor quality of evidence for both VR and Augmented reality)
- Virtual and Augmented realities have shown to impact positively those in rehabilitation
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.