Podcast
Questions and Answers
What is the primary factor determining the rate of sodium transport in the proximal tubule?
What is the primary factor determining the rate of sodium transport in the proximal tubule?
- The permeability of the tight junctions between epithelial cells
- The concentration of sodium in the tubular lumen (correct)
- The presence of antidiuretic hormone (ADH)
- The transport maximum of the sodium pump
Why does sodium leak back into the tubular lumen in the proximal tubule?
Why does sodium leak back into the tubular lumen in the proximal tubule?
- The loose junctions between epithelial cells (correct)
- The presence of aquaporins in the cell membranes
- The action of aldosterone on the distal tubules
- The high permeability of the descending loop of Henle to water
How does the concentration gradient between the tubule lumen and the interstitial fluid affect water reabsorption?
How does the concentration gradient between the tubule lumen and the interstitial fluid affect water reabsorption?
- It has no effect on water reabsorption
- It drives osmosis in the opposite direction of solute movement
- It drives osmosis in the same direction as solute movement (correct)
- It increases the permeability of the tight junctions to water
Where in the nephron are tight junctions least permeable to water?
Where in the nephron are tight junctions least permeable to water?
Which of the following statements about water permeability in the nephron is incorrect?
Which of the following statements about water permeability in the nephron is incorrect?
How does aldosterone influence transport maximums?
How does aldosterone influence transport maximums?
What is the role of aquaporins in water reabsorption?
What is the role of aquaporins in water reabsorption?
Which of these factors is NOT involved in determining the rate of transport in the nephron?
Which of these factors is NOT involved in determining the rate of transport in the nephron?
What is the primary function of the thin descending limb of the loop of Henle?
What is the primary function of the thin descending limb of the loop of Henle?
Which of the following is NOT reabsorbed in the proximal tubule?
Which of the following is NOT reabsorbed in the proximal tubule?
What is the role of the sodium-potassium ATP pump in the thick ascending limb of the loop of Henle?
What is the role of the sodium-potassium ATP pump in the thick ascending limb of the loop of Henle?
What is the primary mechanism by which magnesium, calcium, and potassium are reabsorbed in the thick ascending limb?
What is the primary mechanism by which magnesium, calcium, and potassium are reabsorbed in the thick ascending limb?
Which of these is NOT a characteristic of the thin ascending limb of the loop of Henle?
Which of these is NOT a characteristic of the thin ascending limb of the loop of Henle?
What is the primary function of the sodium-hydrogen counter transporter in the thick ascending limb?
What is the primary function of the sodium-hydrogen counter transporter in the thick ascending limb?
Which of these solutes is reabsorbed in the proximal tubule?
Which of these solutes is reabsorbed in the proximal tubule?
Which of these statements correctly describes the role of the loop of Henle in urine concentration?
Which of these statements correctly describes the role of the loop of Henle in urine concentration?
What is the purpose of inulin in measuring GFR?
What is the purpose of inulin in measuring GFR?
What is the net filtration pressure in the capillaries?
What is the net filtration pressure in the capillaries?
What does a ratio of 3 for inulin concentration in the proximal tubule indicate?
What does a ratio of 3 for inulin concentration in the proximal tubule indicate?
What is the effect of increasing arterial pressure on peri tubular capillary hydrostatic pressure and reabsorption?
What is the effect of increasing arterial pressure on peri tubular capillary hydrostatic pressure and reabsorption?
What is tubular balance?
What is tubular balance?
How does increasing resistance in the afferent arterioles affect peri tubular capillary hydrostatic pressure and reabsorption?
How does increasing resistance in the afferent arterioles affect peri tubular capillary hydrostatic pressure and reabsorption?
How does tubular balance help prevent overloading of the distal tubular segments?
How does tubular balance help prevent overloading of the distal tubular segments?
What is the effect of raising the systemic plasma colloid osmotic pressure on peri tubular capillary reabsorption?
What is the effect of raising the systemic plasma colloid osmotic pressure on peri tubular capillary reabsorption?
What is the normal rate of tubular capillary reabsorption?
What is the normal rate of tubular capillary reabsorption?
What is the filtration coefficient?
What is the filtration coefficient?
Which of the following is NOT a factor that governs the rate of reabsorption across the peritubular capillaries?
Which of the following is NOT a factor that governs the rate of reabsorption across the peritubular capillaries?
How does tubular glomerular feedback contribute to renal autoregulation?
How does tubular glomerular feedback contribute to renal autoregulation?
What is the primary force that drives reabsorption in the peri tubular capillaries?
What is the primary force that drives reabsorption in the peri tubular capillaries?
If the capillary pressure is 13 mmHg and the interstitial hydrostatic pressure is 6 mmHg, what is the net filtration pressure?
If the capillary pressure is 13 mmHg and the interstitial hydrostatic pressure is 6 mmHg, what is the net filtration pressure?
What is the percentage of filtrate reabsorbed by the proximal tubules?
What is the percentage of filtrate reabsorbed by the proximal tubules?
What is the effect of increasing the capillary osmotic pressure on the net filtration pressure?
What is the effect of increasing the capillary osmotic pressure on the net filtration pressure?
What is the primary method by which creatinine is removed from the body?
What is the primary method by which creatinine is removed from the body?
If the rate of creatinine excretion is less than the rate of glomerular filtration, what can be concluded?
If the rate of creatinine excretion is less than the rate of glomerular filtration, what can be concluded?
What is the relationship between creatinine clearance and GFR?
What is the relationship between creatinine clearance and GFR?
What is the filtration fraction?
What is the filtration fraction?
What is the significance of measuring creatinine in the blood?
What is the significance of measuring creatinine in the blood?
What is the primary effect of ANP on the renal tubules?
What is the primary effect of ANP on the renal tubules?
Which hormone increases tubular reabsorption of calcium?
Which hormone increases tubular reabsorption of calcium?
What is the effect of sympathetic stimulation on the renal tubules?
What is the effect of sympathetic stimulation on the renal tubules?
What is the definition of renal clearance?
What is the definition of renal clearance?
What is the relationship between the rate of excretion of a substance and its filtration rate?
What is the relationship between the rate of excretion of a substance and its filtration rate?
Which substance is used to calculate GFR because it is freely filtered and not reabsorbed or secreted?
Which substance is used to calculate GFR because it is freely filtered and not reabsorbed or secreted?
What is the primary mechanism by which creatinine is cleared from the body?
What is the primary mechanism by which creatinine is cleared from the body?
Why is creatinine a suitable marker for estimating GFR?
Why is creatinine a suitable marker for estimating GFR?
Flashcards
Water Permeability
Water Permeability
The capacity of cell membranes to allow water to pass through them.
Proximal Tubule Function
Proximal Tubule Function
Reabsorbs glucose, amino acids, bicarbonate, and excretes waste products.
Loop of Henle Segments
Loop of Henle Segments
Consists of thin descending, thin ascending, and thick ascending limbs with different functions.
Thin Descending Limb
Thin Descending Limb
Signup and view all the flashcards
Thick Ascending Limb
Thick Ascending Limb
Signup and view all the flashcards
Sodium-Potassium ATP Pump
Sodium-Potassium ATP Pump
Signup and view all the flashcards
Secondary Active Transport
Secondary Active Transport
Signup and view all the flashcards
Tubular Lumen Charge
Tubular Lumen Charge
Signup and view all the flashcards
Inulin
Inulin
Signup and view all the flashcards
GFR (Glomerular Filtration Rate)
GFR (Glomerular Filtration Rate)
Signup and view all the flashcards
Tubular Absorption
Tubular Absorption
Signup and view all the flashcards
Proximal Tubule Effect
Proximal Tubule Effect
Signup and view all the flashcards
Tubular Balance
Tubular Balance
Signup and view all the flashcards
Hydrostatic and Colloid Forces
Hydrostatic and Colloid Forces
Signup and view all the flashcards
Renal Autoregulation
Renal Autoregulation
Signup and view all the flashcards
Filtrate Absorption Rate
Filtrate Absorption Rate
Signup and view all the flashcards
Electrochemical Gradient
Electrochemical Gradient
Signup and view all the flashcards
Transport Maximum
Transport Maximum
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
Osmosis
Osmosis
Signup and view all the flashcards
Aquaporins
Aquaporins
Signup and view all the flashcards
Distal Tubule Water Permeability
Distal Tubule Water Permeability
Signup and view all the flashcards
Loop of Henle
Loop of Henle
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Creatinine Clearance
Creatinine Clearance
Signup and view all the flashcards
Renal Plasma Flow
Renal Plasma Flow
Signup and view all the flashcards
Filtration Fraction
Filtration Fraction
Signup and view all the flashcards
Tubular Reabsorption and Secretion
Tubular Reabsorption and Secretion
Signup and view all the flashcards
Net Filtration Pressure
Net Filtration Pressure
Signup and view all the flashcards
Reabsorption
Reabsorption
Signup and view all the flashcards
Filtration Coefficient
Filtration Coefficient
Signup and view all the flashcards
Hydrostatic Pressure
Hydrostatic Pressure
Signup and view all the flashcards
Colloid Osmotic Pressure
Colloid Osmotic Pressure
Signup and view all the flashcards
Interstitial Hydrostatic Pressure
Interstitial Hydrostatic Pressure
Signup and view all the flashcards
Arterial Pressure Influence
Arterial Pressure Influence
Signup and view all the flashcards
Systemic Plasma Colloid Osmotic Pressure
Systemic Plasma Colloid Osmotic Pressure
Signup and view all the flashcards
ANP Function
ANP Function
Signup and view all the flashcards
Parathyroid Hormone
Parathyroid Hormone
Signup and view all the flashcards
Sympathetic Stimulation
Sympathetic Stimulation
Signup and view all the flashcards
Renal Clearance
Renal Clearance
Signup and view all the flashcards
GFR Calculation
GFR Calculation
Signup and view all the flashcards
Creatinine
Creatinine
Signup and view all the flashcards
Sodium and Water Reabsorption
Sodium and Water Reabsorption
Signup and view all the flashcards
Filtration Rate
Filtration Rate
Signup and view all the flashcards
Study Notes
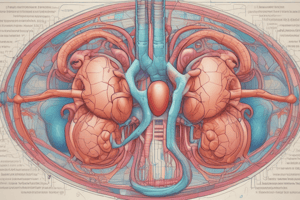
Reabsorption in the Tubules
- Reabsorption of large molecules like proteins occurs via pinocytosis. Proteins attach to the brush border, are encapsulated, digested into amino acids, and reabsorbed through the basal lateral membrane. This is active transport requiring energy.
Filtration
- Filtration is non-selective, meaning substances not bound to proteins are filtered.
- Glomerular filtration is significant compared to urine output.
- Tubular reabsorption is highly selective.
- Substances like glucose and amino acids are almost completely reabsorbed, while sodium and chloride vary based on body needs. Waste products like urea are poorly reabsorbed and excreted.
- Reabsorption mechanisms can be controlled independently.
Reabsorption Mechanisms
- Substances must move from the tubular lumen through the tubular epithelial membrane to the renal interstitial fluid, then through the peritubular capillary membrane to the blood.
- Transcellular or paracellular pathways can be used.
- Hydrostatic and colloid osmotic pressures regulate absorption.
Active Transport
- Active transport moves substances against electrochemical gradients, requiring energy (e.g., sodium-potassium ATPase pump).
Secondary Active Transport
- Coupled indirectly to an energy source (e.g., ion gradients).
- Sodium-potassium pump creates a low intracellular sodium concentration, driving sodium into the cell. This then drives other substances into the cell.
Tubular Reabsorption Summary
- Step 1: Sodium diffuses from the tubular lumen to the cell.
- Step 2: Sodium moves across the basal outer membrane, against the electrochemical gradient, via sodium potassium ATPase pump
- Step 3: Sodium, water and other substances are reabsorbed from the interstitial fluid into peritubular capillaries, driven by hydrostatic and colloid osmotic pressure gradients.
Secondary Active Transport (Glucose/Amino Acids)
- Sodium gradient facilitates movement of glucose/amino acids into the cell
- Carrier proteins in the apical membrane couple Na+ gradient to glucose movement (secondary active transport)
Transport Maximum
- Limited rate of reabsorption due to saturation of transport systems.
- When the load exceeds the transport maximum, excess substances are excreted in the urine. (e.g., glucose)
Reabsorption of Water
- Proximal tubule highly permeable to water, reabsorbing most water.
- Loop of Henle: Descending limb is highly permeable to water; Ascending limb is impermeable to water.
- Distal tubules and collecting ducts: Water permeability regulated by ADH (antidiuretic hormone).
Sodium and Chloride Reabsorption
- Sodium reabsorption is coupled to chloride reabsorption.
- Chloride concentration gradient in tubular fluids drives passive chloride reabsorption.
Other substances
- Urea reabsorption, but to a lesser extent than chloride.
- Creatinine is not reabsorbed, excreted in the urine.
Electrochemical Gradient
- Water follows sodium and chloride to maintain osmotic balance.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.