Podcast
Questions and Answers
What is the primary function of the kidneys regarding waste?
What is the primary function of the kidneys regarding waste?
- Regulating blood pressure
- Absorbing nutrients
- Eliminating waste products (correct)
- Producing hormones
Which factor is NOT associated with increased glomerular filtration rate (GFR)?
Which factor is NOT associated with increased glomerular filtration rate (GFR)?
- Vasodilation of the afferent arteriole
- Vasoconstriction of the efferent arteriole
- Decreased plasma protein concentration (correct)
- Increased arterial blood pressure
Where does the majority of sodium reabsorption occur in the nephrons?
Where does the majority of sodium reabsorption occur in the nephrons?
- Distal convoluted tubule
- Collecting duct
- Loop of Henle
- Proximal convoluted tubule (correct)
Which structure is responsible for transporting materials from blood into the tubular lumen?
Which structure is responsible for transporting materials from blood into the tubular lumen?
What distinguishes the composition of glomerular filtrate from plasma?
What distinguishes the composition of glomerular filtrate from plasma?
Which pathway is involved when ions move across tubular cells?
Which pathway is involved when ions move across tubular cells?
What is the role of the Na+/K+ ATPase in renal physiology?
What is the role of the Na+/K+ ATPase in renal physiology?
How do increased plasma protein concentrations affect GFR?
How do increased plasma protein concentrations affect GFR?
What is the primary action of ADH when concentrations are above those required for antidiuresis?
What is the primary action of ADH when concentrations are above those required for antidiuresis?
Which derivative of ADH is specifically indicated for the treatment of diabetes insipidus?
Which derivative of ADH is specifically indicated for the treatment of diabetes insipidus?
What is the role of organic anion transporters (OATs) in renal secretion?
What is the role of organic anion transporters (OATs) in renal secretion?
How is ammonia formed in the distal convoluted tubule (Dct)?
How is ammonia formed in the distal convoluted tubule (Dct)?
Which ion is exchanged with organic cations during their transport into the tubular lumen?
Which ion is exchanged with organic cations during their transport into the tubular lumen?
What effect does ammonia have when combined with H+ in the renal tubules?
What effect does ammonia have when combined with H+ in the renal tubules?
What is the primary energy source for the transport mechanisms in the renal tubules?
What is the primary energy source for the transport mechanisms in the renal tubules?
Which derivative of ADH is primarily used as a vasoconstrictor during local anesthesia?
Which derivative of ADH is primarily used as a vasoconstrictor during local anesthesia?
What is the primary role of the thick ascending limb in the nephron?
What is the primary role of the thick ascending limb in the nephron?
Which theory explains the concentration and dilution of filtrate in the loop of Henle?
Which theory explains the concentration and dilution of filtrate in the loop of Henle?
How is Ca2+ primarily reabsorbed in the nephron?
How is Ca2+ primarily reabsorbed in the nephron?
What hormone primarily controls Na+ absorption and K+ secretion in the collecting tubules?
What hormone primarily controls Na+ absorption and K+ secretion in the collecting tubules?
What is the consequence of Na+/H+ exchange in the distal convoluted tubule when bicarbonate has been fully reabsorbed?
What is the consequence of Na+/H+ exchange in the distal convoluted tubule when bicarbonate has been fully reabsorbed?
Which of the following best describes the permeability of the distal convoluted tubule (Dct) to water?
Which of the following best describes the permeability of the distal convoluted tubule (Dct) to water?
What is the primary consequence of diuretic use on Na+ and K+ levels in the collecting duct?
What is the primary consequence of diuretic use on Na+ and K+ levels in the collecting duct?
Which type of cell in the collecting tubules is responsible for H+ secretion?
Which type of cell in the collecting tubules is responsible for H+ secretion?
How does aldosterone enhance Na+ reabsorption?
How does aldosterone enhance Na+ reabsorption?
What triggers the secretion of ADH from the posterior pituitary?
What triggers the secretion of ADH from the posterior pituitary?
What initiates the transport of NaCl in the early distal convoluted tubule?
What initiates the transport of NaCl in the early distal convoluted tubule?
Which of the following conditions leads to nephrogenic diabetes insipidus?
Which of the following conditions leads to nephrogenic diabetes insipidus?
What effect does ADH have on the collecting duct?
What effect does ADH have on the collecting duct?
What is the result of ADH deficiency in the kidneys?
What is the result of ADH deficiency in the kidneys?
What is a consequence of enhanced Na+ reabsorption in the nephron?
What is a consequence of enhanced Na+ reabsorption in the nephron?
In what scenario would you expect a significant increase in daily urine output?
In what scenario would you expect a significant increase in daily urine output?
What is the primary role of Na+/K+ ATPase in the transport of Na+ during reabsorption?
What is the primary role of Na+/K+ ATPase in the transport of Na+ during reabsorption?
How is HCO3- primarily reabsorbed in the proximal convoluted tubule (PCT)?
How is HCO3- primarily reabsorbed in the proximal convoluted tubule (PCT)?
What mainly drives the passive reabsorption of water in the proximal convoluted tubule?
What mainly drives the passive reabsorption of water in the proximal convoluted tubule?
What is the major ion reabsorption mechanism in the thick ascending limb?
What is the major ion reabsorption mechanism in the thick ascending limb?
Why does the filtrate become more diluted as it ascends in the thick ascending limb?
Why does the filtrate become more diluted as it ascends in the thick ascending limb?
What physiological condition favors the passive reabsorption of water in the descending limb?
What physiological condition favors the passive reabsorption of water in the descending limb?
Which ions are primarily involved in the reabsorption through the paracellular pathway?
Which ions are primarily involved in the reabsorption through the paracellular pathway?
What mechanism allows CL- to be transported into the blood in the proximal convoluted tubule?
What mechanism allows CL- to be transported into the blood in the proximal convoluted tubule?
Flashcards are hidden until you start studying
Study Notes
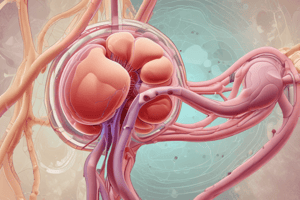
Kidney Functions
- The kidneys eliminate waste products, regulate extracellular fluid volume, electrolyte content, and pH.
- They receive approximately 1/4 of the cardiac output, filter 125 ml of fluid per minute, and excrete 1.5 L of urine per day.
Glomerular Filtration
- The glomerular filtrate is identical to plasma, except it lacks proteins.
- Factors affecting glomerular filtration rate (GFR) include intra-glomerular hydrostatic pressure, intra-glomerular osmotic pressure, and intra-capsular hydrostatic pressure.
Tubular Reabsorption & Secretion
- Tubular reabsorption is the transport of substances from the tubular lumen to the blood, while tubular secretion is the transport from blood to the tubular lumen.
- The lumenal surface of the tubular cell is the brush border (apical) membrane, while the other sides are the basolateral membrane.
- Tight junctions separate the intercellular space from the lumen.
- Ions and water can move via the transcellular pathway across the tubular cells or the paracellular pathway through tight junctions.
Sodium Reabsorption
- Approximately 67% of Na+ is reabsorbed in the proximal convoluted tubule (PCT).
- Na+ is reabsorbed in exchange for H+ via the Na+/H+ antiporter.
- Intracellular carbonic anhydrase is essential for H+ production.
- Na+ is transported into the blood via Na+/K+ ATPase in the basolateral membrane.
- Na+/H+ antiport is driven by Na+/K+ ATPase.
Bicarbonate Reabsorption
- HCO3- is completely reabsorbed in the PCT.
- HCO3- combines with H+ forming H2CO3, which dissociates into CO2 and water.
- CO2 is passively reabsorbed.
Water Reabsorption
- Water is passively reabsorbed through the paracellular pathway, driven by Na+ reabsorption.
- Na+ secreted by Na+/K+ ATPase raises the osmolality of the lateral intercellular space, driving water movement and Na+ reabsorption by convection.
Chloride Reabsorption
- Cl- is transported into the blood partly via the paracellular pathway and partly in exchange for anions like formate and oxalate.
- The fluid leaving the PCT remains isosmotic to the filtrate entering Bowman's capsule.
Descending Limb of the Loop of Henle
- Water is passively reabsorbed due to the hypertonic interstitial fluid of the medulla.
- The filtrate becomes more concentrated (hyperosmotic).
Ascending Limb of the Loop of Henle
- Approximately 20% of filtered Na+ is reabsorbed.
- Na+, K+, and Cl- enter the cell across the apical membrane via a Na+/K+/2Cl- symporter, powered by Na+/K+ ATPase.
- Na+ is transported into the blood via Na+/K+ ATPase.
- Cl- is transported into the blood via Cl- channels and a K+/Cl- symporter.
- Most of the K+ taken by the Na+/K+/2Cl- symporter returns to the lumen through apical K+ channels.
- The thick ascending limb is impermeable to water, resulting in further dilution of the filtrate.
- The thick ascending limb is the "diluting segment."
- The concentration and dilution of filtrate in the loop of Henle is called the "counter-current multiplier theory."
Distal Convoluted Tubule (DCT)
- Approximately 7% of filtered Na+ is reabsorbed.
- NaCl is reabsorbed without water, further diluting the filtrate.
- NaCl is reabsorbed via a Na+/Cl- symporter, driven by Na+/K+ ATPase.
Calcium Reabsorption
- Ca2+ is transported through channels in the apical membrane and into the blood via a Na+/Ca2+ antiporter.
- Parathyroid hormone (PTH) and calcitriol increase Ca reabsorption.
- Ca2+ is also reabsorbed via the paracellular pathway in the ascending limb.
Hydrogen Ion Secretion
- When all filtered HCO3- is reabsorbed, Na+/H+ exchange continues in the DCT.
- H+ is added to Na2HPO4 to give NaH2PO4 and to NH3 to give NH4+.
- Intracellular carbonic anhydrase is essential for H+ production.
Collecting Tubules
- The collecting tubules consist of principal cells (Na+ reabsorption and K+ secretion) and intercalated cells (H+ secretion).
- Ion and water movement is regulated by hormones:
- Aldosterone: controls Na+ reabsorption and K+ secretion.
- Antidiuretic hormone (ADH, vasopressin): controls water reabsorption.
- ADH binds to V2 receptors in the collecting duct cells, increasing water channel expression and rendering the segment permeable to water.
- ADH deficiency (diabetes insipidus) can be neurogenic (due to ADH deficiency) or nephrogenic (due to kidney insensitivity to ADH).
Potassium Secretion
- Potassium secretion is coupled to Na+ reabsorption and is increased by:
- More Na+ reaching the collecting duct (due to diuretics).
- Diuretics increasing Na+ reabsorption in the collecting duct, leading to K+ loss and hypokalemia.
Aldosterone
- Aldosterone enhances Na+ reabsorption and K+ excretion by:
- Stimulating Na+/H+ exchange via membrane aldosterone receptors.
- Activating Na+ channels in the apical membrane.
- Increasing the number of basolateral Na+/K+ ATPase.
Antidiuretic Hormone (ADH)
- ADH is secreted by the posterior pituitary in response to:
- Increased blood osmolality, stimulating osmoreceptors in the hypothalamus.
- Increased blood volume or pressure, inhibiting ADH secretion.
- ADH binds to V2 receptors, increasing water channel expression and allowing passive water reabsorption, resulting in concentrated urine.
- ADH deficiency leads to dilute urine production, polyuria, nocturia, and compensatory polydipsia.
- High ADH concentrations can stimulate V1 receptors in blood vessels, causing vasoconstriction (vasopressin) and increasing blood pressure.
Organic Acid and Base Secretion
- Organic molecules enter the renal tubules by glomerular filtration or are actively secreted directly into the tubules in the PCT.
- Organic anions (A-) are exchanged with α-ketoglutarate via organic anion transporters (OATs) and diffuse into the lumen.
- Organic cations (C+) diffuse into the cell and are actively transported into the lumen in exchange for H+.
- Both systems are powered by Na+/K+ ATPase.
Ammonia Secretion
- Ammonia is formed in the DCT by deamination of glutamine.
- Ammonia diffuses into the lumen and combines with H+ forming NH4+, preventing H+ accumulation in the filtrate.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.