Podcast
Questions and Answers
What physiological consequence would direct damage to the podocytes of the glomerulus most likely lead to?
What physiological consequence would direct damage to the podocytes of the glomerulus most likely lead to?
- Elevated erythropoietin production, leading to polycythemia.
- Decreased secretion of hydrogen ions in the distal convoluted tubule.
- Significant proteinuria (protein in urine) due to impaired filtration. (correct)
- Increased reabsorption of glucose in the proximal convoluted tubule.
The primary function of the renal cortex is to concentrate urine through the countercurrent mechanism.
The primary function of the renal cortex is to concentrate urine through the countercurrent mechanism.
False (B)
How does increased sympathetic nervous system activity directly affect glomerular filtration rate (GFR), and by what mechanism?
How does increased sympathetic nervous system activity directly affect glomerular filtration rate (GFR), and by what mechanism?
Increased sympathetic activity typically decreases GFR by constricting afferent arterioles, reducing blood flow to the glomerulus.
In response to hypovolemia, the kidneys release ______, initiating a cascade that ultimately increases blood pressure and sodium retention.
In response to hypovolemia, the kidneys release ______, initiating a cascade that ultimately increases blood pressure and sodium retention.
Match the following hormones with their primary effect on kidney function:
Match the following hormones with their primary effect on kidney function:
A patient presents with significantly decreased blood pressure due to severe hemorrhage. Which of the following compensatory mechanisms is the kidney least likely to employ in the immediate response?
A patient presents with significantly decreased blood pressure due to severe hemorrhage. Which of the following compensatory mechanisms is the kidney least likely to employ in the immediate response?
The ascending limb of the loop of Henle is permeable to water, facilitating water reabsorption into the medullary interstitium.
The ascending limb of the loop of Henle is permeable to water, facilitating water reabsorption into the medullary interstitium.
Explain the role of the macula densa in tubuloglomerular feedback and how it affects GFR.
Explain the role of the macula densa in tubuloglomerular feedback and how it affects GFR.
Damage to the juxtaglomerular cells would most directly impair the secretion of ______, affecting blood pressure regulation.
Damage to the juxtaglomerular cells would most directly impair the secretion of ______, affecting blood pressure regulation.
Match the following kidney structures with their primary function:
Match the following kidney structures with their primary function:
What is the key mechanism by which the loop of Henle contributes to the formation of concentrated urine?
What is the key mechanism by which the loop of Henle contributes to the formation of concentrated urine?
Atrial natriuretic peptide (ANP) increases sodium reabsorption in the distal convoluted tubule, countering the effects of aldosterone.
Atrial natriuretic peptide (ANP) increases sodium reabsorption in the distal convoluted tubule, countering the effects of aldosterone.
Describe how the kidneys compensate for metabolic acidosis, including the specific mechanisms and locations within the nephron.
Describe how the kidneys compensate for metabolic acidosis, including the specific mechanisms and locations within the nephron.
In the presence of high levels of ADH, the ______ becomes more permeable to water, leading to increased water reabsorption and concentrated urine.
In the presence of high levels of ADH, the ______ becomes more permeable to water, leading to increased water reabsorption and concentrated urine.
Match the following symptoms with the most likely underlying kidney function:
Match the following symptoms with the most likely underlying kidney function:
A patient is diagnosed with primary hyperaldosteronism. Which of the following sets of electrolyte imbalances would you most likely observe?
A patient is diagnosed with primary hyperaldosteronism. Which of the following sets of electrolyte imbalances would you most likely observe?
The efferent arteriole carries blood away from the glomerulus and directly supplies blood to the renal vein.
The efferent arteriole carries blood away from the glomerulus and directly supplies blood to the renal vein.
Explain the concept of pressure natriuresis and its importance in long-term blood pressure regulation.
Explain the concept of pressure natriuresis and its importance in long-term blood pressure regulation.
Blockage of the renal artery would lead to ______ to the kidneys, potentially causing acute kidney injury.
Blockage of the renal artery would lead to ______ to the kidneys, potentially causing acute kidney injury.
Match the following terms with their definitions in the context of kidney physiology:
Match the following terms with their definitions in the context of kidney physiology:
In a patient with diabetes mellitus and uncontrolled hyperglycemia, what effect does this have on glucose reabsorption in the nephron?
In a patient with diabetes mellitus and uncontrolled hyperglycemia, what effect does this have on glucose reabsorption in the nephron?
The renal portal system ensures that blood flows directly from the afferent arteriole to the efferent arteriole without passing through a capillary network, allowing for faster filtration.
The renal portal system ensures that blood flows directly from the afferent arteriole to the efferent arteriole without passing through a capillary network, allowing for faster filtration.
Describe the myogenic mechanism of renal autoregulation and how it helps maintain a stable GFR.
Describe the myogenic mechanism of renal autoregulation and how it helps maintain a stable GFR.
Erythropoietin (EPO) is produced by the kidneys in response to ______, stimulating red blood cell production in the bone marrow.
Erythropoietin (EPO) is produced by the kidneys in response to ______, stimulating red blood cell production in the bone marrow.
Match the following functions with the corresponding part of the nephron:
Match the following functions with the corresponding part of the nephron:
Why is the maintenance of a medullary concentration gradient essential for proper kidney function?
Why is the maintenance of a medullary concentration gradient essential for proper kidney function?
The secretion process in the kidneys involves moving substances from the tubular fluid into the peritubular capillaries.
The secretion process in the kidneys involves moving substances from the tubular fluid into the peritubular capillaries.
Explain the role of angiotensin II in the renin-angiotensin-aldosterone system (RAAS) and its effects on systemic blood pressure.
Explain the role of angiotensin II in the renin-angiotensin-aldosterone system (RAAS) and its effects on systemic blood pressure.
The filtration fraction is calculated by dividing the ______ by the renal plasma flow (RPF).
The filtration fraction is calculated by dividing the ______ by the renal plasma flow (RPF).
Associate each kidney hormone with its primary effect on electrolyte balance:
Associate each kidney hormone with its primary effect on electrolyte balance:
In kidney dialysis, which physiological function of a healthy kidney is most directly replaced?
In kidney dialysis, which physiological function of a healthy kidney is most directly replaced?
Hyperfiltration in the kidneys is always a beneficial adaptive response, improving overall kidney function in the long term.
Hyperfiltration in the kidneys is always a beneficial adaptive response, improving overall kidney function in the long term.
Describe how the kidneys contribute to acid-base balance by regulating bicarbonate (HCO3-) levels in the blood.
Describe how the kidneys contribute to acid-base balance by regulating bicarbonate (HCO3-) levels in the blood.
Damage to the ______ would directly impair the kidney's ability to concentrate urine, leading to conditions like diabetes insipidus.
Damage to the ______ would directly impair the kidney's ability to concentrate urine, leading to conditions like diabetes insipidus.
Match the following kidney-related terms with their descriptions:
Match the following kidney-related terms with their descriptions:
What is the primary mechanism by which NSAIDs (nonsteroidal anti-inflammatory drugs) can lead to acute kidney injury?
What is the primary mechanism by which NSAIDs (nonsteroidal anti-inflammatory drugs) can lead to acute kidney injury?
Increased levels of ANP (atrial natriuretic peptide) would likely result in decreased GFR and increased sodium reabsorption.
Increased levels of ANP (atrial natriuretic peptide) would likely result in decreased GFR and increased sodium reabsorption.
Explain how hypovolemia leads to increased water reabsorption in the collecting ducts, including the hormones involved and their mechanisms of action.
Explain how hypovolemia leads to increased water reabsorption in the collecting ducts, including the hormones involved and their mechanisms of action.
The ______ detects changes in sodium concentration and regulates GFR through tubuloglomerular feedback.
The ______ detects changes in sodium concentration and regulates GFR through tubuloglomerular feedback.
Match the diagnostic term to it's definition:
Match the diagnostic term to it's definition:
Which of the following correctly describes the sequence of filtrate flow through the nephron?
Which of the following correctly describes the sequence of filtrate flow through the nephron?
The primary function of the renal cortex is to concentrate urine before excretion.
The primary function of the renal cortex is to concentrate urine before excretion.
What is the main structural difference between the afferent and efferent arterioles, and how does this difference contribute to glomerular filtration?
What is the main structural difference between the afferent and efferent arterioles, and how does this difference contribute to glomerular filtration?
The countercurrent mechanism in the loop of Henle relies on the ______ loop being permeable to water and impermeable to ions, while the ______ loop is impermeable to water but actively transports ions.
The countercurrent mechanism in the loop of Henle relies on the ______ loop being permeable to water and impermeable to ions, while the ______ loop is impermeable to water but actively transports ions.
Which process is primarily responsible for the reabsorption of glucose in the proximal convoluted tubule (PCT)?
Which process is primarily responsible for the reabsorption of glucose in the proximal convoluted tubule (PCT)?
Secretion is the process by which substances move from the nephron tubule into the peritubular capillaries.
Secretion is the process by which substances move from the nephron tubule into the peritubular capillaries.
How does the secretion of hydrogen ions (H+) in the distal convoluted tubule (DCT) contribute to the maintenance of acid-base balance in the body?
How does the secretion of hydrogen ions (H+) in the distal convoluted tubule (DCT) contribute to the maintenance of acid-base balance in the body?
Glomerular filtration rate (GFR) is maintained relatively constant through autoregulation, involving constriction of the ______ arteriole when blood pressure increases.
Glomerular filtration rate (GFR) is maintained relatively constant through autoregulation, involving constriction of the ______ arteriole when blood pressure increases.
Which hormone directly increases sodium reabsorption in the distal convoluted tubule (DCT) and collecting duct?
Which hormone directly increases sodium reabsorption in the distal convoluted tubule (DCT) and collecting duct?
Antidiuretic hormone (ADH) decreases water reabsorption in the collecting ducts, leading to more dilute urine.
Antidiuretic hormone (ADH) decreases water reabsorption in the collecting ducts, leading to more dilute urine.
How does atrial natriuretic peptide (ANP) counteract the effects of the renin-angiotensin-aldosterone system (RAAS) in regulating blood pressure and fluid balance?
How does atrial natriuretic peptide (ANP) counteract the effects of the renin-angiotensin-aldosterone system (RAAS) in regulating blood pressure and fluid balance?
Parathyroid hormone (PTH) increases calcium reabsorption in the kidneys while inhibiting ______ reabsorption.
Parathyroid hormone (PTH) increases calcium reabsorption in the kidneys while inhibiting ______ reabsorption.
Which of the following demonstrates the direct link between the cardiovascular system and kidney function?
Which of the following demonstrates the direct link between the cardiovascular system and kidney function?
The kidneys participate in the endocrine system by producing hormones such as insulin to regulate blood glucose levels.
The kidneys participate in the endocrine system by producing hormones such as insulin to regulate blood glucose levels.
How do the kidneys and the respiratory system coordinate to maintain acid-base balance in the body?
How do the kidneys and the respiratory system coordinate to maintain acid-base balance in the body?
Sympathetic nervous system activity regulates kidney function mainly through controlling renal ______.
Sympathetic nervous system activity regulates kidney function mainly through controlling renal ______.
What direct effect does chronic kidney disease (CKD) have on the cardiovascular system?
What direct effect does chronic kidney disease (CKD) have on the cardiovascular system?
Dialysis is a curative treatment for chronic kidney disease, restoring kidney function completely.
Dialysis is a curative treatment for chronic kidney disease, restoring kidney function completely.
Describe the importance of the juxtaglomerular apparatus in maintaining systemic blood pressure.
Describe the importance of the juxtaglomerular apparatus in maintaining systemic blood pressure.
Match the following terms with their corresponding descriptions:
Match the following terms with their corresponding descriptions:
In the context of kidney function, what does 'nephron clearance' specifically measure?
In the context of kidney function, what does 'nephron clearance' specifically measure?
Tubular fluid in the nephron remains consistent in composition throughout its passage, with no alteration in its solute concentration or volume.
Tubular fluid in the nephron remains consistent in composition throughout its passage, with no alteration in its solute concentration or volume.
Explain the physiological mechanism behind pressure natriuresis and its role in regulating blood pressure.
Explain the physiological mechanism behind pressure natriuresis and its role in regulating blood pressure.
The macula densa regulates GFR through tubuloglomerular feedback by sensing changes in ______ concentration in the distal tubule.
The macula densa regulates GFR through tubuloglomerular feedback by sensing changes in ______ concentration in the distal tubule.
Which process leads to the formation of urea?
Which process leads to the formation of urea?
Elevated levels of creatinine in the blood typically indicate improved kidney function.
Elevated levels of creatinine in the blood typically indicate improved kidney function.
Explain the difference between acute kidney injury (AKI) and chronic kidney disease (CKD) in terms of onset and potential for recovery.
Explain the difference between acute kidney injury (AKI) and chronic kidney disease (CKD) in terms of onset and potential for recovery.
[Blank] refers to a condition where the kidneys filter more blood than normal, potentially leading to kidney damage in the long term.
[Blank] refers to a condition where the kidneys filter more blood than normal, potentially leading to kidney damage in the long term.
Which of the following directly affects the kidneys' ability to concentrate urine and can be indicative of kidney dysfunction?
Which of the following directly affects the kidneys' ability to concentrate urine and can be indicative of kidney dysfunction?
Flashcards
Kidney
Kidney
Organs that filter blood to remove waste and excess substances, maintaining balance in the body.
Nephron
Nephron
The functional unit of the kidney. Each kidney contains around 1 million nephrons that filter blood, reabsorb useful substances, and excrete waste as urine.
Glomerulus
Glomerulus
A network of tiny blood vessels (capillaries) in the nephron where blood is filtered.
Bowman's Capsule
Bowman's Capsule
Signup and view all the flashcards
Proximal Convoluted Tubule (PCT)
Proximal Convoluted Tubule (PCT)
Signup and view all the flashcards
Loop of Henle
Loop of Henle
Signup and view all the flashcards
Distal Convoluted Tubule (DCT)
Distal Convoluted Tubule (DCT)
Signup and view all the flashcards
Collecting Duct
Collecting Duct
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Filtrate
Filtrate
Signup and view all the flashcards
Reabsorption
Reabsorption
Signup and view all the flashcards
Secretion
Secretion
Signup and view all the flashcards
Urine
Urine
Signup and view all the flashcards
Renin-Angiotensin-Aldosterone System (RAAS)
Renin-Angiotensin-Aldosterone System (RAAS)
Signup and view all the flashcards
Antidiuretic Hormone (ADH)
Antidiuretic Hormone (ADH)
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
Countercurrent Mechanism
Countercurrent Mechanism
Signup and view all the flashcards
Filtration Fraction
Filtration Fraction
Signup and view all the flashcards
Renal Blood Flow (RBF)
Renal Blood Flow (RBF)
Signup and view all the flashcards
Efferent Arteriole
Efferent Arteriole
Signup and view all the flashcards
Afferent Arteriole
Afferent Arteriole
Signup and view all the flashcards
Peritubular Capillaries
Peritubular Capillaries
Signup and view all the flashcards
Vasa Recta
Vasa Recta
Signup and view all the flashcards
Excretion
Excretion
Signup and view all the flashcards
Nephron Clearance
Nephron Clearance
Signup and view all the flashcards
Tubular Fluid
Tubular Fluid
Signup and view all the flashcards
Pressure Natriuresis
Pressure Natriuresis
Signup and view all the flashcards
Macula Densa
Macula Densa
Signup and view all the flashcards
Urea
Urea
Signup and view all the flashcards
Creatinine
Creatinine
Signup and view all the flashcards
Kidney Dialysis
Kidney Dialysis
Signup and view all the flashcards
Hyperfiltration
Hyperfiltration
Signup and view all the flashcards
Ureter
Ureter
Signup and view all the flashcards
Bladder
Bladder
Signup and view all the flashcards
Urethra
Urethra
Signup and view all the flashcards
Diuresis
Diuresis
Signup and view all the flashcards
Polydipsia
Polydipsia
Signup and view all the flashcards
Polyuria
Polyuria
Signup and view all the flashcards
Osmolarity
Osmolarity
Signup and view all the flashcards
Acid-Base Balance
Acid-Base Balance
Signup and view all the flashcards
Glucose Reabsorption
Glucose Reabsorption
Signup and view all the flashcards
Urinous GFR (Filtration) Rate
Urinous GFR (Filtration) Rate
Signup and view all the flashcards
Renal Portal System
Renal Portal System
Signup and view all the flashcards
High Osmolarity
High Osmolarity
Signup and view all the flashcards
Low Osmolarity
Low Osmolarity
Signup and view all the flashcards
Juxtaglomerular Cells
Juxtaglomerular Cells
Signup and view all the flashcards
Hypovolemia
Hypovolemia
Signup and view all the flashcards
Hypoperfusion
Hypoperfusion
Signup and view all the flashcards
Study Notes
- The kidneys regulate fluid balance, electrolytes, and waste products
- Kidneys filter blood to create urine
- They maintain blood pressure and acid-base balance
- Kidneys also secrete hormones
Kidney Anatomy and Structure
- Kidneys are bilateral organs on either side of the spine
Nephron
- Nephron: the functional unit of the kidney responsible for filtering blood and forming urine
- Each kidney contains about one million nephrons
Components of the Nephron
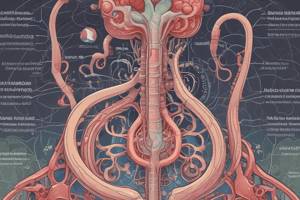
- Glomerulus: a network of capillaries where blood is first filtered
- Bowman’s Capsule: encapsulates the glomerulus and receives the filtrate
Tubules
- Proximal Convoluted Tubule (PCT): reabsorbs nutrients, electrolytes, and water
- Loop of Henle: creates a concentration gradient for water and salt reabsorption
- Distal Convoluted Tubule (DCT): fine-tunes reabsorption and secretes substances like H+ and K+
- Collecting Duct: collects urine from multiple nephrons and plays a major role in water reabsorption, influenced by hormones like antidiuretic hormone (ADH)
Renal Cortex and Medulla
- Renal cortex: the outer region where most nephrons' glomeruli reside, playing a crucial role in early filtration and reabsorption
- Renal medulla: beneath the cortex, contains loops of Henle and collecting ducts, primarily involved in concentrating urine and regulating water balance
Key Renal Functions
- Filtration, reabsorption, secretion, and excretion
Filtration
- Filtration occurs in the glomerulus, where blood enters through the afferent arteriole and is filtered into the Bowman’s capsule
- The filtrate contains water, ions, glucose, and waste products like urea
- High blood pressure increases the filtration rate, potentially damaging the glomeruli
- Low blood pressure reduces filtration, causing waste accumulation
Reabsorption
- Reabsorption primarily occurs in the proximal convoluted tubule (PCT), but also in the loop of Henle, distal convoluted tubule (DCT), and collecting duct
- Water, glucose, amino acids, and electrolytes (Na+, K+, Cl-) are reabsorbed into the bloodstream
- Reabsorption helps maintain homeostasis by regulating the body's levels of nutrients and electrolytes
- The loop of Henle uses a countercurrent exchange mechanism to create a concentration gradient, crucial for water and salt balance
Secretion
- Substances like hydrogen ions (H+), potassium (K+), and certain drugs are secreted into the filtrate, especially in the DCT and collecting ducts
- Secretion helps remove waste products from the bloodstream and regulates pH by controlling H+ levels
Excretion
- After filtration, reabsorption, and secretion, waste products form urine
- Urine contains excess water, urea, uric acid, and other waste products
- Kidneys excrete urine through the ureters, which transport it to the bladder for storage before elimination via the urethra
Regulation of Kidney Functions
Autoregulation of GFR
- Kidneys adjust the diameter of afferent and efferent arterioles to maintain a constant glomerular filtration rate (GFR)
- When blood pressure increases, the kidneys constrict the afferent arteriole to prevent an increase in glomerular filtration
Hormonal Regulation
- Renin-Angiotensin-Aldosterone System (RAAS) helps regulate blood pressure and sodium balance
- Low blood pressure causes juxtaglomerular cells to release renin, activating angiotensin II
- Angiotensin II triggers aldosterone release (increases sodium reabsorption) and causes vasoconstriction to raise blood pressure
- Antidiuretic Hormone (ADH) controls water reabsorption in the collecting ducts
- In the presence of ADH, water reabsorption increases, leading to more concentrated urine
- ADH release is triggered by increased blood osmolarity or decreased blood volume
- Atrial Natriuretic Peptide (ANP) inhibits the RAAS system and promotes sodium excretion
- ANP is released by the heart in response to increased blood volume
- It reduces sodium reabsorption and relaxes afferent arterioles, increasing GFR and urine production to reduce blood volume
- Parathyroid Hormone (PTH) regulates calcium and phosphate balance by increasing calcium reabsorption and inhibiting phosphate reabsorption in the kidneys
Interaction with Other Body Systems
Cardiovascular System
- Blood pressure directly affects the kidneys' ability to filter blood
- The kidneys use renin to influence blood pressure (via RAAS), demonstrating a close relationship with the cardiovascular system in regulating fluid balance
Endocrine System
- Kidneys release erythropoietin (EPO) for red blood cell production
- The kidneys participate in the activation of vitamin D, which influences calcium balance
Respiratory System
- Kidneys and lungs contribute to acid-base balance where kidneys excrete H+ ions and reabsorb bicarbonate (HCO₃-) to help regulate pH
- The lungs control CO2 levels in the blood
Nervous System
- Kidneys are regulated by the sympathetic nervous system (for blood flow control)
- Kidneys also regulated by signaling from the hypothalamus, to regulate ADH secretion in response to hydration status
Homeostasis and Kidney Disease
- Kidneys central to homeostasis by regulating blood volume, pressure, and composition
- Disruption in kidney function—such as in chronic kidney disease (CKD), acute renal failure, or glomerulonephritis—can lead to imbalanced fluid levels, electrolyte disturbances, and toxin accumulation
- Severe cases may require dialysis or kidney transplants
Detailed functions
Kidney Structure and Anatomy
- Each kidney contains around a million nephrons
- Nephrons are microscopic units responsible for filtering blood and forming urine
- Each nephron consists of a renal corpuscle (glomerulus and Bowman’s capsule) and a renal tubule (proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct)
Renal Cortex and Medulla
- Renal Cortex: outer region housing glomeruli and proximal/distal convoluted tubules, where most filtration and the beginning of reabsorption occur
- Renal Medulla: deeper region containing loops of Henle and collecting ducts, important for establishing concentration gradients and fine-tuning water and electrolyte reabsorption
Vascular Supply
- Blood enters through the renal artery and branches into smaller arterioles, supplying blood to each nephron via the afferent arteriole, leading to the glomerulus
- Blood exits the glomerulus via the efferent arteriole
- Remaining blood flows through the peritubular capillaries surrounding the renal tubules
Renal Function in Detail
Glomerular Filtration
- Filters blood through the glomerular membrane into the Bowman’s capsule, with small molecules passing into the filtrate and larger molecules retained
Mechanism
- Filtration barrier consists of:
- Endothelium of glomerular capillaries with fenestrations
- Basement membrane acting as a charge and size filter
- Podocytes with foot processes regulating filtration
- Filtration is driven by glomerular hydrostatic pressure, opposed by colloid osmotic pressure and capsular hydrostatic pressure
Filter Load and GFR
- Glomerular filtration rate (GFR) is the rate at which plasma is filtered into the Bowman’s capsule, typically around 120-125 mL/min in a healthy adult
- GFR is a key measure of kidney function, reflecting the kidneys’ ability to filter blood
Reabsorption of Solutes and Water
Proximal Convoluted Tubule (PCT)
- The site of bulk reabsorption, reabsorbing about 65% of filtered sodium, chloride, and water, along with 100% of glucose and amino acids through active and passive transport
- Sodium is actively transported out via Na+/K+ ATPase, with water following passively due to osmosis
Loop of Henle
- Integral in concentrating urine and establishing a medullary concentration gradient
- The descending loop is permeable to water but impermeable to ions, so water is reabsorbed as the filtrate moves through the hyperosmolar medulla
- The ascending loop is impermeable to water but actively reabsorbs sodium, chloride, and potassium through Na+/K+/2Cl- symporters, creating high osmolarity in the medulla
Distal Convoluted Tubule (DCT)
- Selective reabsorption of sodium, chloride, and calcium occurs, regulated by hormones like aldosterone (increases sodium reabsorption) and parathyroid hormone (PTH, promotes calcium reabsorption)
Collecting Duct
- The final site of water reabsorption regulated by antidiuretic hormone (ADH), which inserts aquaporins into the membrane of the collecting duct
- Aldosterone acts here to increase sodium reabsorption in exchange for potassium secretion
Secretion
- Active transport of substances from the peritubular capillaries into the nephron tubule, eliminating waste and regulating electrolytes/acid-base balance
Substances Secreted
- Potassium (K+): secreted in the DCT and collecting duct in exchange for sodium to maintain electrolyte balance
- Hydrogen ions (H+): secreted in the DCT to regulate blood pH
- Ammonia (NH3) and urea are secreted as part of nitrogenous waste elimination
Importance of Secretion
- Electrolyte Balance: H+ and K+ secretion vital to maintain acid-base/potassium homeostasis
- Detoxification: substances like drugs, toxins, and excess ions that were not filtered by the glomerulus are secreted here to be excreted
Regulatory Mechanisms of Kidney Function
Renal Autoregulation
- Kidneys have intrinsic mechanisms to maintain a stable GFR despite fluctuations in blood pressure, through changes in afferent and efferent arteriole diameter
Myogenic Mechanism
- If blood pressure increases, the afferent arteriole constricts to prevent an increase in filtration pressure
Tubuloglomerular Feedback
- The macula densa in the distal tubule detects flow rate and sodium concentration
- If the flow rate is too high, it signals the afferent arteriole to constrict
Hormonal Regulation
Renin-Angiotensin-Aldosterone System (RAAS)
- Triggered when blood volume or pressure drops
- The kidneys release renin, converting angiotensinogen (from the liver) into angiotensin I
- Angiotensin I is converted to angiotensin II by ACE (angiotensin-converting enzyme) in the lungs
- Angiotensin II stimulates aldosterone release (increasing sodium reabsorption) and causes vasoconstriction to raise blood pressure
- It also stimulates thirst and ADH secretion, enhancing water retention
Antidiuretic Hormone (ADH)
- When blood osmolarity is high, ADH is released from the posterior pituitary to promote water reabsorption in the collecting ducts
Atrial Natriuretic Peptide (ANP)
- ANP is released from the heart in response to increased blood volume, promoting natriuresis (sodium excretion) and increasing urine output
- ANP also inhibits RAAS, reducing blood pressure
Interactions with Other Body Systems
Cardiovascular System
- The kidneys regulate blood volume and blood pressure through RAAS and ADH
- Blood pressure affects GFR directly, and the kidneys’ autoregulatory mechanisms ensure consistent filtration
Endocrine System
- The kidneys regulate blood calcium levels by converting vitamin D into its active form, calcitriol
- Erythropoietin is produced by the kidneys in response to low oxygen levels, stimulating red blood cell production in the bone marrow
Respiratory System
- The kidneys contribute to acid-base balance by excreting hydrogen ions (H+) and reabsorbing bicarbonate (HCO₃-)
Renal Dysfunction and Diseases
- Kidney diseases like CKD or AKI affect the kidney’s ability to filter blood, reabsorb nutrients, and excrete waste, leading to fluid retention, electrolyte imbalances, and toxin accumulation
- These issues can affect the cardiovascular and nervous systems
Key Term Definitions
Kidney
- Organs that filter blood to remove waste and excess substances, maintaining balance in the body
Nephron
- The functional unit of the kidney, filtering blood, reabsorbing useful substances, and excreting waste as urine
Glomerulus
- A network of tiny blood vessels (capillaries) in the nephron where blood is filtered
Bowman's Capsule
- A cup-like structure that surrounds the glomerulus, collecting filtered blood plasma (filtrate)
Proximal Convoluted Tubule (PCT)
- The first part of the nephron where most reabsorption of water, ions, and nutrients happens back into the blood
Loop of Henle
- A U-shaped part of the nephron, responsible for creating a concentration gradient in the kidney to conserve water
Distal Convoluted Tubule (DCT)
- The part of the nephron where more ions are reabsorbed and waste products are secreted into urine
Collecting Duct
- A tube where urine from several nephrons collects, adjusting the concentration of urine by reabsorbing water
Glomerular Filtration Rate (GFR)
- The rate at which the kidneys filter blood, helping evaluate kidney
Filtrate
- The liquid that is filtered from the blood, needing further processing in the nephron to form urine
Reabsorption
- The process of moving substances from the filtrate back into the blood
Secretion
- The process of moving waste products and excess substances from the blood into the filtrate
Urine
- The final product excreted by the kidneys, consisting of waste products
Renin-Angiotensin-Aldosterone System (RAAS)
- A hormone system that regulates blood pressure, blood volume, and sodium balance
Antidiuretic Hormone (ADH)
- A hormone that controls water reabsorption by the kidneys, concentrating the urine
Aldosterone
- A hormone that acts on the kidneys to increase sodium and water reabsorption and potassium excretion
Countercurrent Mechanism
- A process in the loop of Henle that helps create a concentration gradient
Filtration Fraction
- The fraction of plasma entering the kidneys that gets filtered into the nephron
Renal Blood Flow (RBF)
- The amount of blood delivered to the kidneys per minute
Efferent Arteriole
- The blood vessel that carries blood away from the glomerulus after filtration
Afferent Arteriole
- The blood vessel that carries blood toward the glomerulus
Peritubular Capillaries
Small blood vessels that surround the renal tubules, allowing reabsorption and secretion
Vasa Recta
- Specialized capillaries that surround the loop of Henle
Excretion
- The removal of waste products from the body through urine
Nephron Clearance
- The rate at which a substance is cleared from the blood by the kidneys per minute
Tubular Fluid
- The fluid within the nephron resulting from blood filtration
Pressure Natriuresis
- The process by which increased blood pressure leads to increased excretion of sodium and water
Macula Densa
- Specialized cells in the distal convoluted tubule that regulate GFR
Urea
- A nitrogenous waste product formed by the breakdown of proteins
Creatinine
- A byproduct of muscle metabolism, used to estimate kidney function
Kidney Dialysis
- A medical procedure that artificially removes waste and excess fluid from the blood
Hyperfiltration
- A condition where the kidneys filter more blood than normal
Ureter
- The tube that carries urine from the kidneys to the bladder
Bladder
A muscular sac that stores urine
Urethra
- The tube through which urine is excreted from the bladder
Diuresis
- The increased production of urine
Polydipsia
- Excessive thirst
Polyuria
- Excessive urine production
Osmolarity
- The concentration of solutes in a solution
Acid-Base Balance
- The process by which the kidneys regulate the blood's pH
Glucose Reabsorption
- The process by which the kidneys reabsorb glucose from the filtrate
Urinous GFR (Filtration) Rate
- A measure of how much urine is produced as a function of filtration by the kidneys
Additional Terms
Portal System (Renal Portal System)
- Blood flows through two capillary networks (glomerulus → peritubular capillaries/vasa recta) for filtration, reabsorption, and secretion
High Osmolarity
- More solutes, produces concentrated urine
Low Osmolarity
- Fewer solutes, produces diluted urine
Juxtaglomerular Cells
- Monitor BP & sodium, releasing Renin to increase BP and sodium retention
Hypovolemia
- Low blood volume, leading to retaining water & sodium and activating RAAS
Hypoperfusion
- Low blood flow to kidneys, activating RAAS, and reducing urine production with risk of kidney damage
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.