Podcast
Questions and Answers
What are the primary components of blood that need to be described in detail?
What are the primary components of blood that need to be described in detail?
- Platelets, RBCs, and plasma proteins (correct)
- White blood cells and lymphatic fluid
- Red blood cells and neutrophils only
- Electrolytes and nutrient molecules
What is a defining characteristic of the differentiation process of marrow precursor cells into mature blood cells?
What is a defining characteristic of the differentiation process of marrow precursor cells into mature blood cells?
- It results in mature cells that are morphologically identical
- It is completed in less than 24 hours for all cell types
- It is governed solely by external environmental factors
- It varies significantly in duration among different cell types (correct)
What distinguishes primary hemostasis from secondary hemostasis in terms of bleeding types?
What distinguishes primary hemostasis from secondary hemostasis in terms of bleeding types?
- Secondary hemostasis affects blood vessels but not platelets
- Primary hemostasis involves issues with vessel walls and platelets (correct)
- Location of bleeding is always in the skeletal system for primary hemostasis
- Primary hemostasis is characterized by severe bleeding with delayed onset
Which of the following accurately describes thrombocytopenia?
Which of the following accurately describes thrombocytopenia?
In comparing von Willebrand disease and Hemophilia A, which statement is true in terms of lab features?
In comparing von Willebrand disease and Hemophilia A, which statement is true in terms of lab features?
What is a common treatment approach for both von Willebrand disease and Hemophilia A?
What is a common treatment approach for both von Willebrand disease and Hemophilia A?
What is the primary hormone responsible for driving erythropoiesis?
What is the primary hormone responsible for driving erythropoiesis?
Which characteristic distinguishes reticulocytes from mature red blood cells?
Which characteristic distinguishes reticulocytes from mature red blood cells?
How long does it typically take for erythrocytes to mature and enter circulation?
How long does it typically take for erythrocytes to mature and enter circulation?
What percentage of red blood cells (RBCs) are physiologically replaced by the marrow each day?
What percentage of red blood cells (RBCs) are physiologically replaced by the marrow each day?
How is the lifespan of a mature red blood cell typically described?
How is the lifespan of a mature red blood cell typically described?
What clinical test can aid in the determination of the type of anemia a patient may have?
What clinical test can aid in the determination of the type of anemia a patient may have?
Which cellular change is observed in erythrocytopoiesis?
Which cellular change is observed in erythrocytopoiesis?
Which of the following statements about hematopoietic stem cells is true?
Which of the following statements about hematopoietic stem cells is true?
What is the primary function of hematopoiesis in the human body?
What is the primary function of hematopoiesis in the human body?
Which cellular element of blood is primarily responsible for immune response?
Which cellular element of blood is primarily responsible for immune response?
What does the term 'megakaryocytopoiesis' specifically refer to?
What does the term 'megakaryocytopoiesis' specifically refer to?
Which component mentioned is NOT part of the cellular elements found in blood?
Which component mentioned is NOT part of the cellular elements found in blood?
Approximately how many proteins have been identified in plasma?
Approximately how many proteins have been identified in plasma?
Which organ is primarily responsible for producing many proteins of the hemostatic system?
Which organ is primarily responsible for producing many proteins of the hemostatic system?
What is the average adult blood volume in liters?
What is the average adult blood volume in liters?
Which type of cell differentiation occurs during granulocytopoiesis?
Which type of cell differentiation occurs during granulocytopoiesis?
Which type of bleeding is most commonly associated with disorders of primary hemostasis?
Which type of bleeding is most commonly associated with disorders of primary hemostasis?
What characteristic feature differentiates petechiae from purpura?
What characteristic feature differentiates petechiae from purpura?
In patients with primary hemostasis disorders, when does bleeding typically occur after trauma?
In patients with primary hemostasis disorders, when does bleeding typically occur after trauma?
Which of the following is a common acquired cause of thrombocytopenia?
Which of the following is a common acquired cause of thrombocytopenia?
What type of bleeding typically occurs with coagulation factor deficiencies?
What type of bleeding typically occurs with coagulation factor deficiencies?
Ecchymoses are characterized by which of the following?
Ecchymoses are characterized by which of the following?
What is the primary defect in primary hemostasis disorders?
What is the primary defect in primary hemostasis disorders?
When considering skin bleeding, which factor would indicate a defect in primary hemostasis?
When considering skin bleeding, which factor would indicate a defect in primary hemostasis?
What primarily causes anemia?
What primarily causes anemia?
Which mechanism does NOT contribute to anemia?
Which mechanism does NOT contribute to anemia?
What is the average lifespan of platelets in circulation?
What is the average lifespan of platelets in circulation?
What is the primary role of the hemostasis system?
What is the primary role of the hemostasis system?
What distinguishes platelets in their formation?
What distinguishes platelets in their formation?
Which statement about the hemostasis system is TRUE?
Which statement about the hemostasis system is TRUE?
What is the main function of megakaryocytes in the blood system?
What is the main function of megakaryocytes in the blood system?
What does MCV (mean corpuscular volume) indicate?
What does MCV (mean corpuscular volume) indicate?
Flashcards are hidden until you start studying
Study Notes
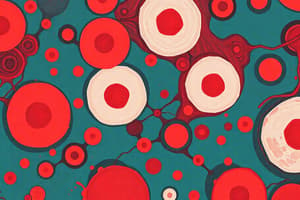
Introduction to Blood Overview
- Average adult blood volume: 5-6 liters.
- Blood comprises cellular elements (WBCs, RBCs, platelets) and non-cellular components (plasma).
- Cellular components primarily sourced from bone marrow, lymph nodes, and thymus.
- Hematopoiesis: differentiation of stem cells into mature erythrocytes, platelets, and WBCs.
- Plasma contains water, sugars, lipids, vitamins, minerals, electrolytes, and over 500 identified proteins, including clotting factors from the liver.
Hematopoiesis and Related Clinical Correlate
- Hematopoietic stem cell transplants are commonly used for leukemia and lymphoma treatment.
- Stem cells can differentiate into other cell types, including muscle and bone.
Erythrocytes (Red Blood Cells)
- Erythrocytopoiesis process takes approximately 7 days; RBC lifespan in circulation is about 120 days.
- Driven by erythropoietin from kidneys in response to hypoxia.
- Reticulocytes: immature RBCs released post-nuclear extrusion; identifiable via special stains.
- Normal marrow replaces about 1% of RBCs daily (~2-4 x 10^9 RBCs/kg/day).
- Reticulocyte count aids in determining anemia type.
Anemia
- Defined as a reduction in RBC count and/or hemoglobin, leading to decreased oxygen transport and organ hypoxia.
- Classification based on mechanism or RBC morphology, particularly mean corpuscular volume (MCV).
- Common causes: blood loss, increased RBC destruction (hemolysis), decreased production.
Platelets
- Formation of platelets (megakaryocytopoiesis) takes 5-10 days; platelets last about 10 days in circulation.
- Megakaryocytes undergo endomitotic division and shed cytoplasmic fragments (platelets) into blood.
Hemostasis System
- Functions: Stop bleeding (clot formation) and prevent excessive clotting (counter-regulatory mechanisms).
- Normal hemostasis involves vessel wall integrity, platelets, and the coagulation cascade.
Clinical Features of Hemostasis Disorders
- Bleeding patterns and severity vary based on defective components:
- Coagulation factor deficiencies lead to deep tissue hematomas and hemarthrosis.
- Disorders of primary hemostasis often result in mucosal bleeding (hematuria, menorrhagia, epistaxis) and skin-related symptoms (purpura, petechiae, ecchymoses).
- Petechiae: minute capillary bleeding indicators of primary hemostasis defects.
- Ecchymoses and purpura: related to either primary or secondary hemostasis disorders.
Timing of Bleeding
- Immediate bleeding post-trauma suggests primary hemostasis defects (thrombocytopenia).
- Delayed bleeding indicates coagulation factor deficiencies.
Thrombocytopenia
- Most common acquired bleeding disorder, with causes including decreased production and increased destruction.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.