Podcast
Questions and Answers
Which feature distinguishes Crohn disease from ulcerative colitis?
Which feature distinguishes Crohn disease from ulcerative colitis?
- Disease is limited to the mucosa
- Can cause transmural inflammation (correct)
- Always involves the rectum
- Extraintestinal manifestations overlap with those of Crohn disease
What is a common extraintestinal manifestation shared by both Crohn disease and ulcerative colitis?
What is a common extraintestinal manifestation shared by both Crohn disease and ulcerative colitis?
- Fistulas
- Primary sclerosing cholangitis
- Clubbing of the fingertips (correct)
- Mucosal bridges
Which of the following is NOT a clinical feature of Crohn disease?
Which of the following is NOT a clinical feature of Crohn disease?
- Abdominal pain
- Fever
- Mild diarrhea
- Continuous proximal extension (correct)
What histopathological finding is associated with ulcerative colitis?
What histopathological finding is associated with ulcerative colitis?
Which statement about the disease pattern of ulcerative colitis is accurate?
Which statement about the disease pattern of ulcerative colitis is accurate?
What is the primary determinant of the severity in ischemic bowel disease?
What is the primary determinant of the severity in ischemic bowel disease?
Which phase of ischemic bowel disease involves the greatest damage related to blood supply restoration?
Which phase of ischemic bowel disease involves the greatest damage related to blood supply restoration?
Transmural infarction in ischemic bowel disease can lead to which serious condition?
Transmural infarction in ischemic bowel disease can lead to which serious condition?
In ischemic bowel disease, which area is specifically noted for being particularly vulnerable to ischemic damage?
In ischemic bowel disease, which area is specifically noted for being particularly vulnerable to ischemic damage?
Which morphological feature is characteristic of mucosal infarcts in ischemic bowel disease?
Which morphological feature is characteristic of mucosal infarcts in ischemic bowel disease?
What is the main cause of diverticular disease?
What is the main cause of diverticular disease?
Which area of the colon is most commonly affected by diverticulosis?
Which area of the colon is most commonly affected by diverticulosis?
What characteristics are associated with acquired pseudo-diverticula?
What characteristics are associated with acquired pseudo-diverticula?
Which dietary factors contribute to the abnormal colonic contractions leading to diverticulosis?
Which dietary factors contribute to the abnormal colonic contractions leading to diverticulosis?
In which imaging modality would sigmoid diverticula typically be observed?
In which imaging modality would sigmoid diverticula typically be observed?
What are the primary causes of mechanical intestinal obstruction?
What are the primary causes of mechanical intestinal obstruction?
What is the most commonly affected area by intestinal obstructions?
What is the most commonly affected area by intestinal obstructions?
Which statement accurately describes a hernia?
Which statement accurately describes a hernia?
What condition occurs when a hernia becomes permanently trapped?
What condition occurs when a hernia becomes permanently trapped?
Which symptom is NOT typically associated with intestinal obstruction?
Which symptom is NOT typically associated with intestinal obstruction?
Which of the following statements is true about strangulated hernias?
Which of the following statements is true about strangulated hernias?
Which process often leads to intestinal obstruction following abdominal surgery?
Which process often leads to intestinal obstruction following abdominal surgery?
What complication arises from impaired venous drainage in an incarcerated hernia?
What complication arises from impaired venous drainage in an incarcerated hernia?
What are the most significant prognostic factors for colorectal adenocarcinoma survival?
What are the most significant prognostic factors for colorectal adenocarcinoma survival?
What does the TNM classification represent in colorectal carcinoma?
What does the TNM classification represent in colorectal carcinoma?
What is the reported overall 5-year survival rate for colorectal cancer in the US?
What is the reported overall 5-year survival rate for colorectal cancer in the US?
Which type of carcinoma is the most common in tumors of the anal canal?
Which type of carcinoma is the most common in tumors of the anal canal?
What commonly initiates acute appendicitis?
What commonly initiates acute appendicitis?
What is the typical lifetime risk percentage for developing acute appendicitis?
What is the typical lifetime risk percentage for developing acute appendicitis?
Which of the following is less commonly associated with luminal obstruction in acute appendicitis?
Which of the following is less commonly associated with luminal obstruction in acute appendicitis?
Which structure is commonly affected by the inflammatory response during acute appendicitis?
Which structure is commonly affected by the inflammatory response during acute appendicitis?
Flashcards
Intestinal Obstruction
Intestinal Obstruction
A blockage in the intestines, often caused by physical obstructions (mechanical) or issues with intestinal function (functional).
Mechanical Obstruction
Mechanical Obstruction
Physical blockages in the intestines, frequently due to hernias, adhesions, intussusception, or volvulus.
Functional Obstruction
Functional Obstruction
Problems with intestinal function causing a blockage, such as ileus (often after surgery).
Abdominal Hernia
Abdominal Hernia
Signup and view all the flashcards
Incarcerated Hernia
Incarcerated Hernia
Signup and view all the flashcards
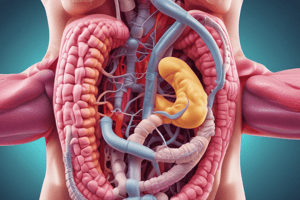
Ischemic Bowel Disease
Ischemic Bowel Disease
Signup and view all the flashcards
Crohn Disease
Crohn Disease
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Diverticular Disease
Diverticular Disease
Signup and view all the flashcards
Diverticulosis
Diverticulosis
Signup and view all the flashcards
Colorectal Adenocarcinoma
Colorectal Adenocarcinoma
Signup and view all the flashcards
Acute Appendicitis
Acute Appendicitis
Signup and view all the flashcards
Study Notes
Intestinal Obstruction
- Small intestine is most often involved due to its narrow lumen
- Can be mechanical or functional
- Hernias, intestinal adhesions, intussusception, & volvulus are responsible for 80% of mechanical obstruction
- Functional obstruction: ileus (especially post-surgical), infarction, etc.
- Clinical manifestations: abdominal pain and distention, vomiting, and constipation
Abdominal Hernia
- A weakness or defect in the peritoneal cavity wall allows a serosa-lined pouch (hernia sac) to protrude
- Acquired hernias commonly occur through the inguinal and femoral canals, umbilicus, or surgical scars
- Risk of visceral protrusion (external herniation), most occur in inguinal hernias
- Small bowel loops typically herniate, but omentum or large bowel can also herniate
Incarcerated Hernia
- Pressure on the neck of the herniated loop can impair venous drainage, leading to stasis and edema
- Increased bulk from edema can lead to permanent entrapment (incarceration)
- Over time, arterial and venous compromise (strangulation) can occur, potentially leading to infarction
Ischemic Bowel Disease
- Acute compromise of a major vessel (thrombosis or embolism) leads to intestinal infarction
- Severity depends on the severity of vascular compromise, duration, and affected vessels
- Two phases: hypoxic injury and reperfusion injury
- Areas particularly vulnerable to ischemia: watershed zone (splenic flexure) and intestinal microvessels
Morphology: Ischemic Bowel Disease
- Mural infarction: mucosal and submucosal infarction
- Acute vascular obstruction: transmural infarction, leading to purulent serositis and perforation
Crohn Disease
- Variable symptoms, including mild diarrhea, fever, and abdominal pain
- Remissions and reactivations are associated with stress, diet, NSAID use, and smoking
- Complications: iron deficiency anemia, malabsorption, strictures, fistulas
- Extraintestinal manifestations: uveitis, polyarthritis, sacroiliitis, ankylosing spondylitis, erythema nodosum, clubbing
Ulcerative Colitis
- Limited to the colon and rectum
- Extraintestinal manifestations overlap with Crohn disease
- Always involves the rectum and extends proximally in a continuous fashion
- Backwash ileitis: mild mucosal inflammation of the distal ileum
Histopathology: Ulcerative Colitis
- Crypt abscesses
- Pseudopyloric metaplasia
- Disease limited to the mucosa
- High-grade dysplasia and invasive adenocarcinoma
Diverticular Disease
- Acquired pseudo-diverticula (not true diverticula)
- Outpouchings of the colonic mucosa and submucosa
- 50% of Western adults over 60 years old have diverticulosis
- Multiple diverticula, most commonly in the sigmoid colon
Pathogenesis: Diverticular Disease
- Develop from elevated intraluminal pressure
- Increased pressure forces mucosa and submucosa through structural weaknesses
- Most diverticula occur in the sigmoid colon due to high pressures during peristalsis
Prognostic Factors: Colorectal Adenocarcinoma
- Depth of invasion and lymph node metastases are the most important prognostic factors
- Invasion into the muscularis propria significantly reduces survival, further decreased by lymph node metastases
- TNM classification is used to define tumor stage
- Five-year survival rates vary worldwide, with overall 5-year survival in the US at 65%.
Tumors of the Anal Canal
- Squamous cell carcinoma (SCC) is the most common, associated with high-risk HPV 16 and 18
- Basaloid or cloacogenic carcinoma.
- Condyloma acuminatum (low-risk HPV related)
Acute Appendicitis
- Most common in adolescents and young adults, lifetime risk of 7%
- Preoperative diagnosis can be difficult, potentially confused with other conditions
- Often associated with obstruction by a fecalith, gallstone, tumor, or worms
Pathogenesis: Acute Appendicitis
- Increased intraluminal pressure compromises venous outflow
- Obstruction triggers inflammatory responses, leading to tissue edema, neutrophilic infiltration, and bacterial proliferation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.