Podcast
Questions and Answers
What is the primary mechanism by which antiamebic drugs eliminate cysts in the intestinal lumen?
What is the primary mechanism by which antiamebic drugs eliminate cysts in the intestinal lumen?
- Directly penetrating and destroying the cyst walls.
- Enhancing the host's immune response to clear the cysts.
- Inhibiting the formation of new cysts by targeting trophozoites. (correct)
- Preventing the excystation process, rendering cysts non-infective.
Which of the following factors is NOT a typical consideration when differentiating between amebic and bacterial liver abscesses?
Which of the following factors is NOT a typical consideration when differentiating between amebic and bacterial liver abscesses?
- Presence of a history of recent travel to endemic areas. (correct)
- Response to specific antibiotics.
- Characteristics of the aspirated abscess material.
- Abruptness of onset and acuity of symptoms.
Why is it recommended to avoid alcohol consumption during and for a short period after treatment with 5-nitroimidazoles?
Why is it recommended to avoid alcohol consumption during and for a short period after treatment with 5-nitroimidazoles?
- Alcohol interferes with the absorption of the medication.
- Alcohol enhances the carcinogenic effects of the drug.
- The combination can lead to a disulfiram-like reaction. (correct)
- Alcohol increases the risk of liver damage.
In the context of amebiasis, what is the significance of identifying anti-amoebic antibodies in an asymptomatic individual's stool sample?
In the context of amebiasis, what is the significance of identifying anti-amoebic antibodies in an asymptomatic individual's stool sample?
What mechanism primarily protects against amebic invasion in individuals exposed to the pathogenic species without developing tissue invasion?
What mechanism primarily protects against amebic invasion in individuals exposed to the pathogenic species without developing tissue invasion?
Which statement accurately reflects current understanding of fatality with amebiasis?
Which statement accurately reflects current understanding of fatality with amebiasis?
When should healthcare providers strongly consider surgical intervention alongside medical therapy for a patient with amebic liver abscess?
When should healthcare providers strongly consider surgical intervention alongside medical therapy for a patient with amebic liver abscess?
Why are stool samples collected via rectal swabs or sigmoidoscopy considered advantageous in diagnosing intestinal amebiasis?
Why are stool samples collected via rectal swabs or sigmoidoscopy considered advantageous in diagnosing intestinal amebiasis?
Why are multiple stool examinations recommended when testing for intestinal amebiasis?
Why are multiple stool examinations recommended when testing for intestinal amebiasis?
A patient is diagnosed with a liver abscess in the right lobe of the liver, elevated liver enzymes, and fever. Which of the following is the most appropriate next step in management?
A patient is diagnosed with a liver abscess in the right lobe of the liver, elevated liver enzymes, and fever. Which of the following is the most appropriate next step in management?
What is the underlying feature common to all amebicides, irrespective of their mechanism of action?
What is the underlying feature common to all amebicides, irrespective of their mechanism of action?
A patient with severe amebic dysentery is not responding to metronidazole. Which of the following would be the most appropriate next step?
A patient with severe amebic dysentery is not responding to metronidazole. Which of the following would be the most appropriate next step?
Which of the following protozoa is most likely responsible for the infection if a microscopic exam reveals a ciliated protozoan?
Which of the following protozoa is most likely responsible for the infection if a microscopic exam reveals a ciliated protozoan?
What is a key consideration regarding the use of corticosteroids in cases of suspected ulcerative colitis in endemic regions?
What is a key consideration regarding the use of corticosteroids in cases of suspected ulcerative colitis in endemic regions?
What explains why individuals harboring a pathogenic species in their intestines might not experience tissue invasion?
What explains why individuals harboring a pathogenic species in their intestines might not experience tissue invasion?
Which method can effectively ensure that water is safe for drinking in areas where amebiasis is of concern?
Which method can effectively ensure that water is safe for drinking in areas where amebiasis is of concern?
What is the primary rationale behind routinely treating asymptomatic individuals who test positive for E. histolytica/E. dispar?
What is the primary rationale behind routinely treating asymptomatic individuals who test positive for E. histolytica/E. dispar?
What diagnostic information from stool microscopy warrants suspicion for a non-amebic infection?
What diagnostic information from stool microscopy warrants suspicion for a non-amebic infection?
The pathogenesis of amebiasis can be summarized by which of the following statements?
The pathogenesis of amebiasis can be summarized by which of the following statements?
How does Entamoeba histolytica initiate its adherence to target cells lining the colon?
How does Entamoeba histolytica initiate its adherence to target cells lining the colon?
After diagnosing patient with amebic liver abscess and starting treatment, the provider notes the source of infection is likely the water, what advice is best?
After diagnosing patient with amebic liver abscess and starting treatment, the provider notes the source of infection is likely the water, what advice is best?
What is one of the many effects of metronidazole?
What is one of the many effects of metronidazole?
The best treatment option for extraintestinal amebiasis are ______.
The best treatment option for extraintestinal amebiasis are ______.
In endemic regions especially, what test is useful in diagnosing liver abscesses?
In endemic regions especially, what test is useful in diagnosing liver abscesses?
Which is more useful test in determining the E. histolytica species?
Which is more useful test in determining the E. histolytica species?
What should be done once test results are in and it is known that amoebas is in the colon?
What should be done once test results are in and it is known that amoebas is in the colon?
Which parasite can only be observed in the trombozoites?
Which parasite can only be observed in the trombozoites?
Amebiasis can be detected by a variety of tests, which of the tests has to be carefully reviewed by trained personnel to detect parasites in any samples?
Amebiasis can be detected by a variety of tests, which of the tests has to be carefully reviewed by trained personnel to detect parasites in any samples?
What is a common cause of why some areas are prone to diarrhea and other stomach related ailments?
What is a common cause of why some areas are prone to diarrhea and other stomach related ailments?
In what situations might a doctor consider surgical intervention for the liver?
In what situations might a doctor consider surgical intervention for the liver?
Some patients are more susceptible to amebiasis if they are ____.
Some patients are more susceptible to amebiasis if they are ____.
True or False: A patient receiving antibiotics is not susceptible to amebiasis?
True or False: A patient receiving antibiotics is not susceptible to amebiasis?
What part of the world is most susceptible to becoming infected with amebiasis?
What part of the world is most susceptible to becoming infected with amebiasis?
Which factors support invasion into tissues with pathogenic cells?
Which factors support invasion into tissues with pathogenic cells?
Name a food or drink related variable that allows more infections to occur?
Name a food or drink related variable that allows more infections to occur?
Which approach most reduces the risk of transmission of amebiasis in highly endemic areas?
Which approach most reduces the risk of transmission of amebiasis in highly endemic areas?
What describes the nature to consider treating as an outpatient with the following?
What describes the nature to consider treating as an outpatient with the following?
Flashcards
Amebiasis
Amebiasis
Infection caused by Entamoeba histolytica, a parasite infecting the large intestine, potentially causing ulcers and extraintestinal spread.
How is amebiasis transmitted?
How is amebiasis transmitted?
Ingestion of cysts through fecal contamination of hands, water or food causes this
Where is amebiasis primarily found?
Where is amebiasis primarily found?
Primarily found in poorer nations
Who is at higher risk?
Who is at higher risk?
Signup and view all the flashcards
Amebiasis: symptoms range
Amebiasis: symptoms range
Signup and view all the flashcards
What is the E. histolytica adhesions?
What is the E. histolytica adhesions?
Signup and view all the flashcards
What is the host resistance?
What is the host resistance?
Signup and view all the flashcards
Lesions in submucosa
Lesions in submucosa
Signup and view all the flashcards
How can you control amebiasis?
How can you control amebiasis?
Signup and view all the flashcards
Which medications act in the colon?
Which medications act in the colon?
Signup and view all the flashcards
Which medications act on tissular amebas?
Which medications act on tissular amebas?
Signup and view all the flashcards
Alternative to Metronidazole
Alternative to Metronidazole
Signup and view all the flashcards
Secnizadole has
Secnizadole has
Signup and view all the flashcards
Infection with amebiasis by .
Infection with amebiasis by .
Signup and view all the flashcards
Infection and invasison.
Infection and invasison.
Signup and view all the flashcards
The disease causing for .
The disease causing for .
Signup and view all the flashcards
What kind of antibodies to search?
What kind of antibodies to search?
Signup and view all the flashcards
What genus does it include?
What genus does it include?
Signup and view all the flashcards
Cycle begins as.
Cycle begins as.
Signup and view all the flashcards
Where is situated?
Where is situated?
Signup and view all the flashcards
Quisite form has.
Quisite form has.
Signup and view all the flashcards
Study Notes
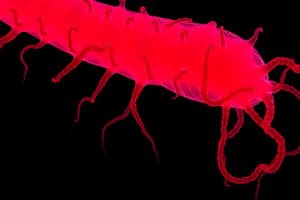
Unit 2: Intestinal Parasitosis by Protozoa
- Unit 2 covers intestinal parasitosis caused by protozoa
- It includes intestinal amebiasis and other intestinal protozooses
Capítulo 2. Intestinal Amebiasis
- The chapter focuses on the study of intestinal amebiasis
Hepatic Amebiasis
- Preventative measures are difficult to establish for amebic hepatic abscess
- Recommendations focus on preventing intestinal amebiasis, which precedes hepatic invasion
Treatment of Amebiasis
- 5-nitroimidazoles are the drugs of choice, acting directly on the trophozoites in the abscess wall
- Treatment duration is generally 5-10 days
- Surgical intervention to drain the abscess is rarely required
- Hepatic amebic abscess treatment is mainly chemotherapy
- Evacuating punctures and surgical drainage have specific indications
- Antiamebic therapy adjustments are made based on needs and severity
- Surgeon assistance is considered if chemotherapy is inefficient
Managing Persistent Cases
- Suspect a pyogenic abscess and culture necrotic material or start antibiotics if antiamebic therapy fails
- 5-nitroimidazoles are highly effective, curing 90% as a single medication
- Remaining cases need puncture or surgery
Metronidazole Usage
- The oldest 5-nitroimidazole, is used at 30-50 mg/kg/day orally, about 2 g daily for adults, split into three doses with meals
- Treatment lasts 5-10 days
- Intravenous metronidazole is an option when oral is unfeasible, presented at 5% in venous perfusion, with doses dependent on volume
- Dosage is 10 mg/kg for over 12s and 7.5 mg/kg for younger, administered every 8 hours for 5-10 days
Other Nitroimidazoles
- Ornidazole comes in 500 mg tablets and injectable form, using similar metronidazole doses
- Tinidazole is given at 2 g daily for adults, 50-60 mg/kg for children, single dose after meal for 3-5 days
- Secnidazole is also effective at 30 mg/kg/day for multiple days
- Chapter on intestinal amebiasis covers precautions, side effects, toxicity, and other medication details
Second-Line Treatments
- Dehydroemetine is dosed at 1 mg/kg/day for 5-10 days, although discontinued in some countries due to toxicity limitated use
- Antibiotics are not routine unless a superimposed bacteria exists or diagnostic uncertainty exists
- Non-absorbable amebicides are added to the regimen in conjunction with amebiasis to eliminate parasites from the colon and prevent returns
Surgical Procedures
- Evacuating puncture is prone to overuse, which induces secondary infections
- It remains essential when symptoms worsen with medication after 5 days and when abscesses present as large/ rupture likely
- Surgery takes place in the surgical ward under guaranteed aseptic conditions
- Surgical intervention only occurs if symptoms worsen, persist
Chronic Amebiasis/ Non-Dysenteric Amebic Colitis
- It is defined as the case in which colitis-like symptoms are present in the absence of dysentery
- Symptoms are long-lasting and may follow an acute attack
- Primarily causes abdominal pain, alterations in bowel habits which causes diarrhea, mucus in stool, rarely blood
- Effort and urge to defecate are less frequent than in acute amebiasis
- Spasmodic pain intensifies before and during bowel movements
- Bowel habit changes can reflect changes in the frequency or number of bowel movements
- Bowel changes have variable duration and intensity
- Stools are diarrheic that can contain trophozoites and sometimes cysts
Additional Symptoms of Chronic Amebiasis
- The amebic will often experience post-eating fullness, nausea, bloating, and borborygmi
- Colon and sigmoid palpation produces palpable pain during clinical examination
- Chronic phase may evolve into other forms or spontaneous healing through symptoms will still show
Acute Amebiasis/ Dysenteric Amebic Colitis
- Primary symptom: excessive intestinal evacuations lead to copious, loose stools then smaller stools with mucus and blood
- Patients require a great deal of effort to evacuate
- Stool diminishes each bowel movement until only sanguinolent mucus, known as rectal sputum, is eliminated
- Bowel evacuation prompts burning sensations which leads to cramping rectal spasms
- Tenesmus: prompts the perceived need to continue defecating in the absence of stool
- Daily bowel movements vary, usually six or more
- Fecal matter has hematophagous trophozoites
- Mucosal ulcers are discernable through endoscopy which causes pain and cramps
Complications
- Complications can arise if the patient's general condition is compromised
- Without resolution fever is absent and can indicate infection
- Hyperthermia causes general symptoms like weakness and dehydration along with rectitis
Post-Amebic Diarrheic Syndrome
- Condition where parasites are not found after treatment has concluded
Fulminant Amebic Colitis
- Exceedingly hyperacute amebiasis
- Intense abdominal pain, diarrhea, urge to purge, anorexia and emaciation lead to the infection
- Bacterial infections can occur causing higher sensitivity on physical exams
Symptoms of Hepatic Amebiasis
- While not entirely consistent, symptoms can be categorized as follows
- Rarely a magnitude of lesions can persist without symptoms
- General discomfort and low energy are prominent in hepatic lesions
- Liver's pain fluctuates in severity but is typically higher in upper right abdominal quadrant and worsens during inhaling
Fever
- Fever arises with intermittent intensity
- Can be confused with parasitical conditions
Hepatomegaly
- Enlargement will depend on the severity of the tumor
- Lungs can experience pulmonary issues due to hepatic compression
Dissemination
- Via hematogenous introduction to other organs
- Cases generally occur among general health compromised
Hepatitis
- From anatomical perspective this condition isn't recognizable
- Considered initial process, but always in transition
Diagnosis
- Hepatic abscess closely mimics wide-scale illness and produces severe pain
- Imaging occurs through eschemia, blood samples are obtained through ELISA
Diagnostic Scenarios for Differential Illnesses
- Hepatitis and tumors produce hepatic masses
- Atypical pathogens incite perihepatic ache
- Spherocytes give rise to febrile
Complications From Disease Progression
- Shock is frequently the precursor
- Metronidazole treatment with surgical interventions increased survival outcomes from 0%-40%
Additional Complications
- More advanced forms of the condition include gangrenous colitis and intestinal rupture
- Occurs with malnutrition and defensive immunologic response compromise
Amebiasis Perforation
- Rupture occurs in necrotic fulminate forms
- Perforation can slowly advance to retroperitoneum
Ameboma Manifestation
- Occurs as tangible painful mass of varying size found most frequently with the sigmoid and rectum
- The parasitic infection may be mistaken for carcinoma
Amebiasis Appendicitis
- Mimics manifestations of bacterial appendicitis
- Histological study clarifies the diagnosis
Symptomatic Diagnosis
- Many varying etiologies stem from colon
- Coprologic exams prevent full diagnosis because positivity is variable
Enhanced Diagnosis
- Can be achieved through increased collection of a stool samples
- Additional culture testing can be facilitated with better detection
Differential Diagnoses
- Intestinal amebiasis is diverse and can share traits across various medical condition
- 70% of infectious agents can now be discerned by experts
Acquired Resistance
- Individuals in at risk areas can be exposed with lesser frequency
- Trials imply development, which is dependent upon the parasite
Immune Response
- Tissue damage by amoeba invokes host immune reactions
- This is demonstrated by greater IgG levels
Positive reactions
- Can arise years following parasitic infection
- Prevents over-estimation and is a serological index
Cellular Immunity
- Infections determine lesion control
- Initial amoebic infection isn't influenced by cell mediated pathways in gut
Fecal Samples
- Must be taken at specified intervals
- Saline solutions must be used to preserve for longer examination
Microscopic Testing
- Primary use is to highlight trophozoites
- This provides analysis of amebic characteristics
- Trophozoites must be differentiated by the type of colitis presented
Other Microscopic Factors
- Stool type as a feature to find cysts
- Lugol preparation to look at trophozoite
- Hematoxylin is used study morphology
- Quists are mainly found in solid stool
Accurate Detection
- Can occur when stool exams take place over a 10-day period
- This process enables enhanced parasite recovery between 85%-95%
Diagnoses
- Lab settings must confirm presence of diarrhea
- Fecal sample collection must be done before barium use via rectum
Diagnostic Laboratory Collection Standards
- Enema use can only facilitate collection with saline
- Trophozoites can change with altered pH
Infection
- Can occur through direct exposure from the large intestines
- Infection requires lab analysis to ensure correct etiology
Stool Samples
- Stool must analyzed with lab testing
- Clinical difference in shigellosis can be made with microscopic testing
Precautionary Methods
- Can prevent negative consequences from use
- Colon cancer can present as the result
Laboratory Diagnosis
- Requires stool removal when spontaneous
- Stool sample can be taken 24 hours after release
Three Primary causes
- Are composed of giardiasis amebiasis cryptosporidiosis
Biopsies
- In colon infections amoeba can be classified with standard staining _E. histolytica only exists between amoeba form
Fecal Immunological Testing
- Modern technique is a method differentiation _Antibodies are a type protein to detect
Serological Testing
- Test can confirm reactions
- The serum creates new interactions
The Three Primary Causes of Parasitic Diarrhea
-Giardiasis, amebiasis, cryptosporidiosis are tested through lab testing
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.