Podcast
Questions and Answers
Which of the following is NOT a cell type involved in innate immunity?
Which of the following is NOT a cell type involved in innate immunity?
- Natural Killer cells
- Mast cells
- T cells (correct)
- Macrophages
What is the primary function of phagocytes in innate immunity?
What is the primary function of phagocytes in innate immunity?
- To produce antibodies
- To engulf and destroy extracellular antigens (correct)
- To activate complement proteins
- To present antigens to T cells
Which of the following is a characteristic of innate immunity?
Which of the following is a characteristic of innate immunity?
- Specificity for individual antigens
- Development of immunological memory
- Rapid response to infection (correct)
- Production of antibodies
What is the role of C-reactive protein (CRP) in innate immunity?
What is the role of C-reactive protein (CRP) in innate immunity?
Which of the following is an example of an anatomical barrier in innate immunity?
Which of the following is an example of an anatomical barrier in innate immunity?
Which of the following statements is TRUE about the cells of the immune system?
Which of the following statements is TRUE about the cells of the immune system?
What is the role of resident flora in innate immunity?
What is the role of resident flora in innate immunity?
Which of the following is a characteristic of acute-phase reactants?
Which of the following is a characteristic of acute-phase reactants?
Which of the following cell types are classified as antigen presenting cells?
Which of the following cell types are classified as antigen presenting cells?
What is the main function of CD8+ T cells?
What is the main function of CD8+ T cells?
Which MHC class presents antigens to CD4+ T cells?
Which MHC class presents antigens to CD4+ T cells?
What is the primary role of CD4+ T cells in the immune response?
What is the primary role of CD4+ T cells in the immune response?
Which of the following statements accurately describes the relationship between T cells and MHC molecules?
Which of the following statements accurately describes the relationship between T cells and MHC molecules?
What is the primary role of natural killer cells in the immune system?
What is the primary role of natural killer cells in the immune system?
Which of the following cells are MOST responsible for the release of histamine, a key mediator of allergic reactions?
Which of the following cells are MOST responsible for the release of histamine, a key mediator of allergic reactions?
Which of the following cells is primarily involved in the elimination of parasitic worms (helminths)?
Which of the following cells is primarily involved in the elimination of parasitic worms (helminths)?
Which of the following cell types is the LEAST abundant in circulating blood?
Which of the following cell types is the LEAST abundant in circulating blood?
What is the primary function of MHC molecules in antigen presentation?
What is the primary function of MHC molecules in antigen presentation?
Which of the following cell types is NOT considered an antigen-presenting cell (APC)?
Which of the following cell types is NOT considered an antigen-presenting cell (APC)?
Which of the following cells is responsible for increasing vascular permeability, contributing to inflammation?
Which of the following cells is responsible for increasing vascular permeability, contributing to inflammation?
Which of the following is TRUE about macrophages?
Which of the following is TRUE about macrophages?
Where do B cells differentiate in mammals?
Where do B cells differentiate in mammals?
What is the primary function of cytotoxic T cells?
What is the primary function of cytotoxic T cells?
Which of the following is NOT a characteristic of the adaptive immune system?
Which of the following is NOT a characteristic of the adaptive immune system?
Which of these cells are NOT considered phagocytes?
Which of these cells are NOT considered phagocytes?
What type of T cell is involved in activating B cells during an adaptive immune response?
What type of T cell is involved in activating B cells during an adaptive immune response?
Which of the following statements is TRUE regarding PRRs and PAMPs?
Which of the following statements is TRUE regarding PRRs and PAMPs?
What is the primary function of antibodies?
What is the primary function of antibodies?
Which of the following statements accurately describes a thymocyte?
Which of the following statements accurately describes a thymocyte?
Flashcards
Immune System Cells
Immune System Cells
Cells arising from pluripotent stem cells, including lymphocytes and phagocytes.
Lymphoid Lineage
Lymphoid Lineage
Produces lymphocytes; main types are T cells and B cells.
Innate Immunity
Innate Immunity
Generic, non-specific immune response without memory.
Humoral Factors
Humoral Factors
Signup and view all the flashcards
C-reactive Protein (CRP)
C-reactive Protein (CRP)
Signup and view all the flashcards
Phagocytes
Phagocytes
Signup and view all the flashcards
Resident Flora
Resident Flora
Signup and view all the flashcards
MHC Antigens
MHC Antigens
Signup and view all the flashcards
Monocytes
Monocytes
Signup and view all the flashcards
Macrophages
Macrophages
Signup and view all the flashcards
Neutrophils
Neutrophils
Signup and view all the flashcards
Basophils
Basophils
Signup and view all the flashcards
Eosinophils
Eosinophils
Signup and view all the flashcards
Mast Cells
Mast Cells
Signup and view all the flashcards
Natural Killer Cells
Natural Killer Cells
Signup and view all the flashcards
Antigen Presenting Cells (APCs)
Antigen Presenting Cells (APCs)
Signup and view all the flashcards
T cells
T cells
Signup and view all the flashcards
CD4+ T cells
CD4+ T cells
Signup and view all the flashcards
CD8+ T cells
CD8+ T cells
Signup and view all the flashcards
Major Histocompatibility Complex (MHC)
Major Histocompatibility Complex (MHC)
Signup and view all the flashcards
Cytokines
Cytokines
Signup and view all the flashcards
PRRs
PRRs
Signup and view all the flashcards
PAMPs
PAMPs
Signup and view all the flashcards
Adaptive Immunity
Adaptive Immunity
Signup and view all the flashcards
Cytotoxic T cells
Cytotoxic T cells
Signup and view all the flashcards
Memory response
Memory response
Signup and view all the flashcards
Study Notes
Innate Immunity
- Innate responses are generally non-specific and generic.
- Innate immune cells lack immunological memory.
- Innate defenses include humoral factors, cells, anatomical barriers, resident flora, and secretions.
Host Defenses in Innate Immunity
- Humoral factors and Acute-Phase Reactants: Complement proteins, C-reactive protein (CRP), lactoferrin, lysozyme, pepsin (stomach acidity).
- Anatomical barriers: Cilia, mucus, skin.
- Resident flora: Many non-pathogenic bacteria.
- Cells: Antigen-presenting cells (APCs), basophils, eosinophils, mast cells, natural killer cells, phagocytes.
Types of Acute-Phase Reactants
- C-reactive protein (CRP): Response time: 4-6 hours; Normal concentration: 0.5 mg/dL; Increase: 1000x; Function: Opsonization, complement activation.
- Serum Amyloid A: Response time: 24 hours; Normal concentration: 5 mg/dL; Increase: 1000x; Function: Activates monocytes and macrophages.
- Alpha1-antitrypsin: Response time: 24 hours; Normal concentration: 200-400 mg/dL; Increase: 2-5x; Function: Protease inhibitor.
- Fibrinogen: Response time: 24 hours; Normal concentration: 200-400 mg/dL; Increase: 2-5x; Function: Clot formation.
- Haptoglobin: Response time: 24 hours; Normal concentration: 40-290 mg/dL; Increase: 2-10x; Function: Binds hemoglobin.
- Ceruloplasmin: Response time: 48-72 hours; Normal concentration: 20-40 mg/dL; Increase: 2x; Function: Binds copper and oxidizes iron.
- Complement C3: Response time: 48-72 hours; Normal concentration: 60-140 mg/dL; Increase: 2x; Function: Opsonization, lysis.
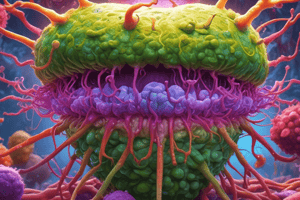
Cells of Innate Immunity
- Phagocytes: Engulf extracellular antigens into vacuoles, destroying them. Monocytes in blood are phagocytic. Including but not limited to:
- Monocytes: Circulate in the blood, have some phagocytic capability but not as effective as macrophages, can migrate to tissues but are short-lived.
- Macrophages: Develop from blood monocytes in tissues, long-lived;
- Neutrophils: Phagocytic; over 90% of circulating granulocytes.
- Basophils: Least common granulocyte; release histamine and heparin.
- Eosinophils: Granulocyte found mostly in tissues; Parasite fighter, release toxic proteins for helminths.
- Mast cells and Basophils: Increase vascular permeability; reside in connective tissue and mucous membranes, regulate inflammatory response.
- Natural killer (NK) cells: Destroy infected cells (e.g., viral, transformed). Found without exposure to antigens.
Receptors: PRRs and PAMPS
- Pathogen-Recognition Receptors (PRRs): On immune cells, recognize molecules (PAMPs) unique to infectious organisms.
- PRRs are found on: Macrophages, dendritic cells, neutrophils, eosinophils, monocytes, mast cells, and epithelial cells.
- Activation: PRRs bind to PAMPS, triggering phagocytic cell activation.
- Example: Toll-like receptors (TLRs).
Adaptive Immunity
- Adaptive immunity adapts to the encountered antigens.
- Key players: Phagocytes (innate), B cells (lymphocytes), antibodies (adaptive) when the antigen is extracellular.
- B cell activation requires specific CD4+ T cells (TH2) and their cytokines.
- Characterized by a more rapid, stronger memory response.
Lymphocytes
- Two types: T cells and B cells.
- T cells: Differentiate in the thymus.
- B cells: Differentiate in mammals (fetal liver, spleen, and adult bone marrow); in avians differentiate in the bursa of Fabricius.
Cells of Adaptive Immunity
- B cells and Plasma cells: Produce antibodies (anamnestic or secondary immune response).
- CD4+ T cells: Produce cytokines that enhance cytotoxic molecule production in phagocytes (TH1), regulate antigen-presenting cell activation (innate), and induce NK cell proliferation (innate).
- Cytotoxic T cells: Lyse infected cells (virally infected cells).
B Cells
- B cell antigen-specific receptor is an antibody molecule on the B cell surface.
- Recognizes whole antigens without antigen processing.
- Membrane immunoglobulin.
T Cell Thymocyte
- Progenitor T cells migrate to the thymus to become mature T cells, called thymocytes.
- Some seed secondary lymphoid tissue, while others recirculate between blood and lymphoid tissue until they encounter antigens.
- Leave the thymus as CD4+ T or CD8+ T cells.
T Cells
- Take part in cell-mediated and humoral immunity.
- In humoral immunity, antibodies play a subordinate role.
- Important for all other aspects of immunity.
T Cells Classification
- CD4+ T cells: Main function: secreting cytokines needed for regulating all immune responses and combating extracellular pathogens (Helper T cells).
- CD8+ T cells: Main role: destroying infected (intracellular pathogens) cells (Killer T cells or Cytotoxic T cells).
T Cells and MHC
- T cells recognize ("non-self") pathogens by detecting processed antigens presented in conjunction with "self" MHC (major histocompatibility complex) molecules.
- Antigen-presenting cells:
- Dendritic cells
- Macrophages
- B cells
- CD8+ T cells: Recognize antigens coupled to Class I MHC molecules (self).
- CD4+ T cells: Recognize antigens coupled to Class II MHC molecules (self).
- Class I MHC: found on variety of cell types.
- Class II MHC: primarily found on antigen-presenting cells.
CD8+ T Cell
- Kill cells infected with intracellular pathogens or those that are otherwise damaged or dysfunctional.
CD4+ T Cell
- Release cytokines that influence the activities of various cell types.
- Cytokines produced enhance macrophage's microbicidal function and killer T cell activity.
Adaptive Immunity: Humoral and Cellular Responses
- T cell receptors only recognize antigens presented on MHC molecules.
- Cellular immunity involves killing infected cells.
- Humoral immunity involves antibody production.
Regulatory T Cells (Tregs)
- Suppressor T cells produce chemicals (cytokines) to "turn off" other immune system cells when an infection is brought under control.
Normal IR: Process of Inflammation
- Body's overall response to tissue injury (physical, chemical, or infectious).
- Cardinal signs:
- Rubor (redness): vasodilation.
- Calor (heat): increased blood flow.
- Tumor (swelling): increased fluid/exudate.
- Dolor (pain): stimulation of nerve endings.
Initiation of Local Inflammatory Response
- Tissue damage and bacteria activate resident sentinel cells to release chemoattractants and vasoactive factors.
- This triggers increased blood flow and capillary permeability.
- Permeable capillaries allow fluid (exudate) and cells to flow into the affected area.
- Phagocytes and antibacterial substances destroy bacteria.
- Neutrophils and other phagocytes migrate to the site of inflammation.
Hypersensitivity
- Four types, all involving initial sensitization.
- Type I (Allergy): IgE-mediated; immediate response.
- Type II (Cytotoxic): IgG or IgM-mediated cell destruction.
- Type III (Immune Complex): Immune complexes depositing, triggering complement activation.
- Type IV (Delayed): Cell-mediated; T-cells activated, leading to inflammatory response.
Diseases Manifesting Delayed Type Hypersensitivity
- Chronic diseases in humans linked to infectious agents (e.g., tuberculosis, leprosy, leishmaniasis).
- Also linked to Deep fungal infections and helminthic infections.
- Activate T cells and macrophages.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.