Podcast
Questions and Answers
Which of the following is a common cause of fractures?
Which of the following is a common cause of fractures?
- Lack of exercise
- Infection
- Trauma (correct)
- Poor diet
Bone fractures and bone bruises are essentially the same type of injury.
Bone fractures and bone bruises are essentially the same type of injury.
False (B)
In describing fractures, what does 'pattern' refer to?
In describing fractures, what does 'pattern' refer to?
- The age of the patient
- The location of the bone in the body
- The shape or appearance of the fracture line (correct)
- The event that caused the break
Which type of fracture occurs at an angle across the bone?
Which type of fracture occurs at an angle across the bone?
A transverse fracture runs parallel to the direction of the bone.
A transverse fracture runs parallel to the direction of the bone.
What distinguishes a greenstick fracture from other types of fractures?
What distinguishes a greenstick fracture from other types of fractures?
Which of the following describes a comminuted fracture?
Which of the following describes a comminuted fracture?
In a segmental fracture, what happens to the fractured bone?
In a segmental fracture, what happens to the fractured bone?
Which type of fracture results from a twisting motion?
Which type of fracture results from a twisting motion?
Stress fractures are most commonly found in which part of the body?
Stress fractures are most commonly found in which part of the body?
What occurs in an avulsion fracture?
What occurs in an avulsion fracture?
Buckle fractures are most commonly seen in which population?
Buckle fractures are most commonly seen in which population?
What is unique about a displaced clavicle fracture?
What is unique about a displaced clavicle fracture?
Which diagnostic tool is most commonly used to identify a bone fracture?
Which diagnostic tool is most commonly used to identify a bone fracture?
What is the primary goal of traction in treating fractures?
What is the primary goal of traction in treating fractures?
Skin traction involves inserting a K-wire directly into the bone.
Skin traction involves inserting a K-wire directly into the bone.
What is a critical nursing responsibility regarding traction equipment?
What is a critical nursing responsibility regarding traction equipment?
What is the purpose of the padding used under a cast?
What is the purpose of the padding used under a cast?
How frequently should a nurse assess neurovascular status in a patient with a cast?
How frequently should a nurse assess neurovascular status in a patient with a cast?
Why is it important to avoid getting a cast wet?
Why is it important to avoid getting a cast wet?
Which of the following is a primary nursing intervention to prevent skin breakdown under a cast?
Which of the following is a primary nursing intervention to prevent skin breakdown under a cast?
What is the surgical cutting of the fascia to relieve tension or pressure commonly associated with?
What is the surgical cutting of the fascia to relieve tension or pressure commonly associated with?
A procedure to realign a broken bone without surgery is called a ______ reduction.
A procedure to realign a broken bone without surgery is called a ______ reduction.
After a closed reduction, what is typically used to maintain the bone's alignment during healing?
After a closed reduction, what is typically used to maintain the bone's alignment during healing?
What is a potential complication following a bone fracture?
What is a potential complication following a bone fracture?
What is the primary purpose of internal fixation?
What is the primary purpose of internal fixation?
Which assessment finding is an indication of a potential infection at the pin sites of an external fixator?
Which assessment finding is an indication of a potential infection at the pin sites of an external fixator?
What is arthroplasty designed to do?
What is arthroplasty designed to do?
What is an essential nursing action when preparing a bed for a patient returning from arthroplasty?
What is an essential nursing action when preparing a bed for a patient returning from arthroplasty?
Which of the following is a common complication of arthroplasty?
Which of the following is a common complication of arthroplasty?
What is the primary cause of sprains?
What is the primary cause of sprains?
Which of the following activities places individuals at a higher risk for ACL injuries?
Which of the following activities places individuals at a higher risk for ACL injuries?
What is the main purpose of exercises in reducing ACL injury risk?
What is the main purpose of exercises in reducing ACL injury risk?
In the case scenario provided, the patient's femur fracture was initially stabilized using skin ______, also known as Buck’s traction.
In the case scenario provided, the patient's femur fracture was initially stabilized using skin ______, also known as Buck’s traction.
A contraindication in caring for a patient in skin traction is to remove the traction periodically to prevent skin breakdown.
A contraindication in caring for a patient in skin traction is to remove the traction periodically to prevent skin breakdown.
If a patient with a cast complains of numbness and tingling in the toes, which complication should the nurse suspect?
If a patient with a cast complains of numbness and tingling in the toes, which complication should the nurse suspect?
Describe three key components that are included within an external bone structure.
Describe three key components that are included within an external bone structure.
What is the potential risk for clients who are claustrophobic and immobilized in large casts?
What is the potential risk for clients who are claustrophobic and immobilized in large casts?
During an isometric exercise, what adjustments are needed in the upper body?
During an isometric exercise, what adjustments are needed in the upper body?
Flashcards
What is a fracture?
What is a fracture?
A break in the continuity of a bone, usually caused by trauma, falls, car accidents, or sports injuries.
How are fractures classified?
How are fractures classified?
Fractures are classified by their pattern, cause and location on the body.
What is an oblique fracture?
What is an oblique fracture?
A fracture where the bone is broken at an angle., often affecting long bones.
What is a transverse fracture?
What is a transverse fracture?
Signup and view all the flashcards
What is a greenstick fracture?
What is a greenstick fracture?
Signup and view all the flashcards
What is a comminuted fracture?
What is a comminuted fracture?
Signup and view all the flashcards
What is a segmental fracture?
What is a segmental fracture?
Signup and view all the flashcards
What is a spiral fracture?
What is a spiral fracture?
Signup and view all the flashcards
What is a stress fracture?
What is a stress fracture?
Signup and view all the flashcards
What is an avulsion fracture?
What is an avulsion fracture?
Signup and view all the flashcards
What is a buckle/impacted fracture?
What is a buckle/impacted fracture?
Signup and view all the flashcards
What is a clavicular fracture?
What is a clavicular fracture?
Signup and view all the flashcards
What is a shoulder fracture?
What is a shoulder fracture?
Signup and view all the flashcards
What are treatments for fractures?
What are treatments for fractures?
Signup and view all the flashcards
What is traction?
What is traction?
Signup and view all the flashcards
What are types of traction?
What are types of traction?
Signup and view all the flashcards
What are nursing responsibilities in traction?
What are nursing responsibilities in traction?
Signup and view all the flashcards
What do you consider when applying a cast?
What do you consider when applying a cast?
Signup and view all the flashcards
What are the types of casts?
What are the types of casts?
Signup and view all the flashcards
What to assess before/after a cast?
What to assess before/after a cast?
Signup and view all the flashcards
Nursing Diagnoses related to casts?
Nursing Diagnoses related to casts?
Signup and view all the flashcards
What is nursing management for casts?
What is nursing management for casts?
Signup and view all the flashcards
How to relieve cast syndrome?
How to relieve cast syndrome?
Signup and view all the flashcards
What is Acute Compartment Syndrome?
What is Acute Compartment Syndrome?
Signup and view all the flashcards
What are the 5 P's of compartment syndrome?
What are the 5 P's of compartment syndrome?
Signup and view all the flashcards
What is a fasciotomy?
What is a fasciotomy?
Signup and view all the flashcards
What is closed reduction?
What is closed reduction?
Signup and view all the flashcards
What is internal fixation?
What is internal fixation?
Signup and view all the flashcards
What is the nursing care for internal fixation?
What is the nursing care for internal fixation?
Signup and view all the flashcards
What is an external fixation?
What is an external fixation?
Signup and view all the flashcards
What is the nursing care for external fixation?
What is the nursing care for external fixation?
Signup and view all the flashcards
What is Arthroplasty?
What is Arthroplasty?
Signup and view all the flashcards
What are possible arthroplasty complications?
What are possible arthroplasty complications?
Signup and view all the flashcards
What are sports injuries?
What are sports injuries?
Signup and view all the flashcards
What are types of sports injuries?
What are types of sports injuries?
Signup and view all the flashcards
What is ACL injury?
What is ACL injury?
Signup and view all the flashcards
How do you reduce and prevent injuries?
How do you reduce and prevent injuries?
Signup and view all the flashcards
Study Notes
Injuries and Altered Coordination
- Fractures are typically caused by trauma, falls, car accidents, or sports injuries
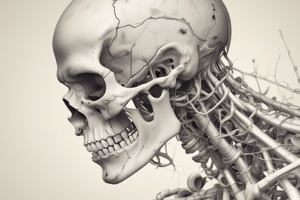
Review of the Skeletal System
- The skeletal system involves bones, joints, cartilage, and ligaments
- It provides structural support, enables movement through muscle interaction, and protects vital organs
- It also produces blood cells in bone marrow and stores minerals like calcium
- Bones are the skeleton's main structural units, consisting of compact, cancellous bone, and the periosteum
Bone Fractures Explained
- Bone fractures and broken bones are the same injury that describes a broken bone
- Bone fractures and bruises are painful injuires caused by strong forces; the difference is the severity of the bone damage
- Common sports injuries include bone fractures and sprains
- A sprain occurs when ligaments are stretched or torn
Classifications of Fractures
- Fractures can be classified by pattern, cause, and body part
Oblique Fractures
- Occur when a bone breaks at an angle and are referred to as complete fractures
- The break line goes all the way through the bone
- Oblique fractures commonly affect long bones like the femur, tibia, fibula, humerus, radius, ulna, and clavicle
Transverse Fractures
- These fractures run horizontally, perpendicular to the bone's direction
- They are also referred to as complete fractures because the break line goes through the bone
- Commonly affect long bones such as the femur, tibia, fibula, humerus, radius, ulna, and clavicle
Greenstick Fractures
- This type of fracture occurs when a bone bends enough to crack but doesn't break entirely into multiple pieces
- Greenstick fractures usually affect longer bones, including the humerus, radius, ulna, phalanges, femur, and fibula
Comminuted Fractures
- This type are fractures where the bone is broken into at least two places
- These fractures can affect any large or long bone in the body
- Some common bones that can be affected are the femur, tibia, fibula, humerus, radius, ulna, clavicle, and skull
Segmental Fractures
- They occur when a bone breaks in at least two places, creating a segment fully separated by the breaks
- Segmental fractures tend to affect long bones like the femur, tibia, fibula, humerus, radius, and ulna
Spiral Fractures
- These fractures happen when a bone breaks due to a twisting motion, creating a corkscrew-like fracture line
- They are also referred to as complete fractures as the break runs completely through the bone
- Spiral fractures usually occur in long bones in the body like the femur, tibia, fibula, talus, humerus, radius, ulna, phalanges and metacarpals
Stress Fractures
- Stress fractures involve small cracks in a bone
- Stress fractures are fractures that happen when something puts too much stress on your bone
- They are most likely to happen in the lower leg (tibia and fibula), foot and heel
Avulsion Fractures
- They’re fractures where a small piece of bone attached to a tendon or ligament gets pulled away from the main part of the bone
- Avulsion fractures may occur in the elbow, ankle, foot, knee, fingers, wrist, pelvis, spine and hip
Buckle/Impacted Fractures
- These fractures usually affect children
- They're incomplete fractures where the break doesn't go completely through the bone
- Buckle fractures are possible in the femur, tibia, fibula, or humerus
Clavicular Fracture
- The clavicle can crack in one or several regions
- If broken in multiple locations, it is called a comminuted fracture
- Displacement of fractured collarbone pieces determine if it its called a displaced fracture
Shoulder Fracture
- Occurs in a broken bone of the shoulder joint
Oblique Fracture Symptoms
- Symptoms may include pain, swelling, tenderness, loss of function, bruising, discoloration, and deformity
Treatment for Fractures
- Immobilization with traction and casting
- Closed reduction
- Surgical intervention such as internal and external fixation
- Arthroplasty
- Bone grafting
Traction
- In medical terms, traction is the application of a pulling force to a body part to treat injuries or disorders
- It is used to treat bone and muscle injuries like fractures, dislocations, and muscle spasms
- It is utilized on the arms, legs, pelvis, or spine for short-term or long-term treatment
- Pulling force is balanced by an opposing force
Purpose of Traction
- It is to realign broken or dislocated joints
- To keep a joint stable, prevents or controls muscle spasms
- Treats long-term issues such as spinal stenosis, degenerative disk disease, and scoliosis
Types of Traction
- Skin traction (buck traction) involves strapping the affected limb and attaching weights
- Skeletal traction involves inserting a K-wire through a bone
Nursing Responsibilities for Patients in Traction
- Inspecting/cleaning skin and pin sites, applying dressings, and preventing soft-tissue breakdown
- Ensuring a patient is positioned correctly
- Assisting with range of motion exercises for unaffected body parts
- Monitoring nutritional status, encouraging a balanced diet, and ensuring hydration
- Providing client education and promoting deep-breathing exercises
- Monitoring vital signs for the patient
- Ensuring the traction weight bag is hanging freely, replacing frayed ropes, and keeping the rope in the pulley tracks
- Keeping blankets and sheets away from traction ropes, keeping bed side rails up and locked, and preventing patient movement in bed
Casts
- Casts are used to immobilize a broken bone or injured area to help it heal
- Padding and stockinette should apply light pressure
- Consider adding extra padding to swollen forearms to alleviate pressure spots
- If numbness, tingling, or tightness develops after discharge, seek immediate medical attention
Application of Casts
- To immobilize a body part in a specific position
- To put uniform compression on soft tissue
- Provides early mobilization of unaffected body parts
- To keep the bone in place and stabilizes unstable joints
Cast Materials
- Plaster casts mold very smoothly but take 24-72 hours to dry, giving off heat
- Fiberglass casts are dry in 10–15 minutes and can bear weight in 30 minutes
- Polyester-cotton knit casts take 7–10 minutes to dry and can withstand bearing weight
Cast Types
- Short arm casts are for wrist and forearm fractures
- Long arm casts are for upper arm, elbow, or forearm fractures
- Shoulder spica casts are for shoulder dislocations or after shoulder surgery
- Short leg casts are for lower leg fractures, ankle fractures, or severe ankle sprains
- Leg cylinder casts are for knee or lower leg fractures, knee dislocations, or after leg or knee surgery
- Cast braces are made of hard plastic with soft pads
- Splints are made of plaster or fiberglass slabs that hold the injury still
Assessment for Patients with Casts
- Evaluate the client's pain with a focus on severity, nature, location, source and the exacerbating factors
- Assess neurovascular status
- Inspect and document any skin lesions, discoloration, or removable foreign material
- Evaluate the client ability to learn essential procedures
Possible Nursing Diagnosis for Patients with Casts
- Deficient knowledge related to the treatment regimen may be necessary
- Acute pain related to the musculoskeletal disorder related to the injury
- Physical immobility may lead to bathing,hygiene, and dressing deficit
- Related skin issues may occur due to lacerations
- Risk of neurovascular dysfunction
Nursing Management of Casts
- Clean the skin of the affected part thoroughly, explain the procedure and obtain informed consent if surgery is required
- Support an exposed cast to prevent indentations
- Ensure that the stockinet is free and clear of the area
- Elevate the casted extremity above the heart and expose the affected portion
- Refrain from wetting cast, and dry patient's synthetic cast with a hair dryer on cool setting
Management Steps for Cast Care after Application
- Encourage position changes
- Elevate the affected area & administer prescribed pain medications
- Promote non-pharmacological pain relief measures, such as guided I magery, relaxation and distraction
- Observe for signs and symptoms of cast syndrome
Observations for Cast Syndrome
- Note any reports of abdominal pain and distension
- Note any reports elevated blood pressure, tachycardia, and tachypnea among other issues due to cast syndrome
- Note any client who is claustrophobic as they may be at risk for psychological cast syndrome.
- Provide care for compartment syndrome and notify health care workers regarding neurovascular complications
Important Steps to Teach Clients with Casts
- Isometric exercises to strengthen muscles covered by the cast
- The importance of promptly reporting cast breaks, warning patients about sharp objects, and teaching appropriate cast care
Acute Compartment Syndrome
- It results from increased pressure in a muscle compartment
- It can lead to muscle and nerve damage and problems with blood flow
- Thick layers of tissue, called fascia, separate groups of muscles in the arms and legs, and muscles, blood vessels, and nerves are located here
- Fascia does not expand, which leads to increased pressure
Symptoms of Acute Compartment Syndrome
- Pain: Out of proportion to an injury and worsened with passive stretch
- Paresthesia: Tingling or a pins and needles feeling
- Pallor: Pale skin as a result of reduced blood flow
- Pulselessness: Occurs in only late stages when pulses may still be present
- Paralysis: Sign of late stages
Treatment for Acute Compartment Syndrome
- Prevent permanent damage and immediate surgery
- The surgery that will be performed is called a fasciotomy
- Important nursing considerations are if a cast or bandage is too tight, stopping repetitive exercises, and raising the affected area above the heart
Closed Reduction
- A non-surgical procedure that realigns a broken or dislocated bone without surgery
- It is performed by an orthopedic surgeon within emergency room or primary care provider
- Healthcare professional will apply force in traction to the affected area
- The broken bone is manipulated and placed in its normal position
After Care for Closed Reduction
- A cast or splint is placed to promote healing and can take 8–12 weeks
- May experience some mild bone pain and may have nerve damage
Possible Complications and Concerns for Closed Reduction
- Nerve damage and vascular injury
- Movement of fat particles and development of blood clots
When to Contact a Doctor After A Closed Reduction
- Report any Persistent pain, swelling, redness and changes to skin
Internal Fixation
- A surgical procedure that uses metal implants to stabilize broken bones
- It is often part of an open reduction (ORIF) procedure
- Techniques include rods placed through the bone that holds everything together, along with pins and wires
Aspects of Nursing Care for Internal Fixation Patients
- Assessment and monitoring of surgical sites, vital signs, and the neurovascular status
- Manage pain with pain killers and non-pharmacological treatments/techniques
- Maintain clean and dry dressings on the site and patient education is crucial
Mobility and Psychosocial Aspects In Nursing Care Post Internal Fixation
- Assist with ambulation and physical therapy
- Explain postoperative plans and educate the patient
- Address anxiety and provide reassurance
External Fixation
- A surgical procedure that uses a rigid frame to stabilize broken or dislocated joints
- The frame is attached with pins or wires through the skin
- Important to educate and ensure families care and clean the affected external area
Care for Patients with an External Fixator
- Change dressings as needed and Elevate the limb to reduce swelling
- Remove crusting and adhere to treatment plans given
- Consider the impact of this device on the patient, their mental health
- Provide patients with proper direction, support, and specialist
Arthroplasty
- Surgical procedure that replaces a damaged joint with an artificial joint
Common Types of Arthroplasty
- Hip and knee replacement
- Total joint replacement of the ankle including elbow
- Also finger replacements and should arthroplasty available
Important Nursing Actions in Arthroplasty Care
- Prepare for the surgery & rigorously check all bed linens
- Check Balkan frame to ensure it is suitable
Possible Complications That May Result From Osteoplasty
- Infections may occur if post-operative care is not followed
- Issues with dislocation and fractures may occur due to movement
Sports Injuries
- Sports injuries can be caused by trauma or from overuse of muscles, including sprains/strains, and fractures
- Bruises are caused by blunt force and sprains
- These are stretches or tears of the ligaments that affect the ankles, knees, or wrists
- Strains will cause the twisting or tearing the muscles, fractures that cracked the bone, dislocations, mild brain injury will lead to concussions
Anterior Cruciate Ligament Tear (ACL)
- ACL is a tearing of a ligament that connects the ligaments to the femur to the tibia
- Commonly occurs in sports because of sudden changes in direction and movement can cause a large shock to your musculoskeletal frame
Risk Factors for Causing ACL:
- Gender - the most prominent risk factor caused by difference in structure or hormone levels
- Poor conditioning & footwear are other important points that may result in ACL
- You can prevent ACL injury by working on exercises and leg strength
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.