Podcast
Questions and Answers
What is a common symptom experienced by patients with HIV infection?
What is a common symptom experienced by patients with HIV infection?
- Prolonged exposure to the sun
- Rash
- Generalized flu-like symptoms (correct)
- Skin rash
What is a crucial aspect of nursing care for patients with SLE?
What is a crucial aspect of nursing care for patients with SLE?
- Monitoring the patient's pain level and medication use (correct)
- Providing diagnosis and treatment options
- Performing diagnostic tests
- Administering immunosuppressive therapy
What is the primary mechanism by which HIV destroys immune cells?
What is the primary mechanism by which HIV destroys immune cells?
- By penetrating the body through blood and body fluids
- Through direct destruction of macrophages and T4 helper cells
- Through infusion of genetic material into host cells (correct)
- By impairing the immune response
What is the duration of the latent stage of HIV infection?
What is the duration of the latent stage of HIV infection?
What is the purpose of encouraging patients with SLE to avoid prolonged exposure to the sun?
What is the purpose of encouraging patients with SLE to avoid prolonged exposure to the sun?
Why is it essential to provide accurate and consistent information to patients with SLE?
Why is it essential to provide accurate and consistent information to patients with SLE?
What is the typical CD4 cell level that indicates a patient has AIDS?
What is the typical CD4 cell level that indicates a patient has AIDS?
What is the name of the antiretroviral drug regimens used to treat HIV?
What is the name of the antiretroviral drug regimens used to treat HIV?
What is a common symptom of HIV infection?
What is a common symptom of HIV infection?
What is a risk factor for HIV infection?
What is a risk factor for HIV infection?
What is a complication of HIV infection?
What is a complication of HIV infection?
During which stage of HIV infection does the patient begin to experience opportunistic infections?
During which stage of HIV infection does the patient begin to experience opportunistic infections?
What is a common opportunistic infection experienced by patients with AIDS?
What is a common opportunistic infection experienced by patients with AIDS?
What is the term for the stage of HIV infection where the patient is asymptomatic and CD4 cells continue to decline?
What is the term for the stage of HIV infection where the patient is asymptomatic and CD4 cells continue to decline?
What is the primary mode of transmission of Healthcare-Associated Infections (HAIs)?
What is the primary mode of transmission of Healthcare-Associated Infections (HAIs)?
What is the recommended duration of hand rubbing with a waterless antiseptic?
What is the recommended duration of hand rubbing with a waterless antiseptic?
What is the primary clue to immunodeficiency?
What is the primary clue to immunodeficiency?
What is the goal of desensitization in allergy treatment?
What is the goal of desensitization in allergy treatment?
What is the first step in the Be Safe guide for patients with allergies?
What is the first step in the Be Safe guide for patients with allergies?
What is the treatment for anaphylaxis?
What is the treatment for anaphylaxis?
What is the purpose of immunosuppressive therapy in organ transplantation?
What is the purpose of immunosuppressive therapy in organ transplantation?
What is the purpose of contact precautions?
What is the purpose of contact precautions?
What is the purpose of airborne infection isolation?
What is the purpose of airborne infection isolation?
What is the recommended daily fluid intake for patients with an infection?
What is the recommended daily fluid intake for patients with an infection?
Study Notes
Infections
- Asymptomatic persons may be more contagious than those exhibiting symptoms
- Symptoms of localized infections:
- Redness
- Pain
- Warmth
- Swelling
- Pus may form
- Patients with generalized infections may not show all signs of infection
- Pain and swelling severity depend on location
- Warmth is expressed as fever in generalized infections
- Other symptoms of generalized infections:
- Malaise
- Anorexia
- Prostration
Types of Infections
- Community Acquired Infections:
- Acquired in day-to-day contact with the public
- Examples: childhood illnesses, TB, HIV/AIDS, foodborne illnesses, STIs
- Prevention methods:
- Ensure childhood immunizations are complete
- Adult immunizations
- Hand washing and proper food handling
- Sanitation of water supplies
- Proper hygiene
- Use of personal barriers like condoms
- Staying home when sick
- Health-Care Associated Infections (HAIs):
- Occur within a healthcare facility
- More serious due to virulent and resistant bacteria
- Examples: VRE, MRSA
- Prevention methods:
- Contact precautions
- Standard precautions
- Use of single patient rooms when available
Care of Patients with Infections
- Medical Asepsis:
- Limiting the spread of microorganisms
- Also known as clean technique
- Practices:
- Changing bed linens
- Sanitizing bed linens
- Using personal equipment for each patient
- Frequent hand hygiene
- Hand Hygiene:
- Soiled hands are the primary mode of transmission of HAIs
- Effective hand hygiene methods:
- Soap and water
- Waterless antiseptic with at least 60% alcohol
- Surgical scrub
- Rub hands together for at least 20 seconds
- Rub waterless antiseptic until dry
- Surgical Asepsis:
- Sterile technique
- Elimination of microorganisms through chemical or physical sterilization
- Techniques to prevent unsterile surfaces from coming into contact with the patient
- Standard Precautions:
- Used for all patients in the hospital
- Practices:
- Use of gloves, gowns, and masks
- Hand hygiene
- Cleaning and disinfecting surfaces
- Respiratory hygiene and cough etiquette
- Airborne Infection Isolation:
- For patients with diseases that spread through the air
- Examples: TB, SARS, varicella, rubeola
- Practices:
- Use of negative pressure rooms
- Properly fitted N95 masks
- Patients with airborne infections require a surgical mask when leaving their rooms
- Droplet Precautions:
- For patients with diseases that spread through droplets
- Examples: COVID-19, rubella, mumps, diphtheria, influenza
- Practices:
- Use of surgical masks
- Placing patients in private rooms
- Staff and visitors must wear a surgical mask when within 3 feet of the patient
- Contact Precautions:
- For patients with diseases that spread through direct or indirect contact
- Practices:
- Use of gloves and gowns
- Use of dedicated patient care equipment
- Cleaning and disinfecting surfaces
- Examples of diseases that require contact precautions: GI infections, respiratory tract infections, skin and wound infections
Nursing Care of the Patient with an Infection
- Urge patients to consume adequate fluids (at least 2L per day)
- Encourage patients to consume high protein and high vitamin foods
- Isolate patients to prevent spread of infection
- Lab tests used to screen patients for infection:
- White blood cell count
- Erythrocyte Sedimentation Rate (ESR)
- Iron Level
- Cultures of urine, blood, and sputum
- White blood cell differential count
- Caution patients not to stop taking medication when they start feeling better
Immunodeficiency
- Definition: When the body's self-defenses against foreign invaders fail to function normally
- Types of immunodeficiencies:
- Congenital
- Acquired
- Causes of acquired immunodeficiency:
- Infections
- Malignancies
- Autoimmune diseases
- Chronic diseases
- Drugs
- Aging
- Stress
- Malnutrition
- Treatment of immunodeficiency:
- Congenital: replacement therapy of the deficient immune component
- Acquired: correcting the underlying condition
- Nursing care for immunocompromised patients:
- Use good hand hygiene
- Encourage adequate nutrition
- Perform effective skin, mouth, perineal, wound, and IV site care
- Encourage patient to turn, cough, and deep breathe
- Use protective isolation
- Use disposable equipment
- Educate patient on signs and symptoms of infection
- Provide a supportive listening environment
Hypersensitivity and Allergy
- Definition: An atypical immune response that is activated by a foreign substance that is normally inoffensive
- Causes of hypersensitivity:
- Genetic predisposition
- Environmental factors
- Examples of allergens:
- House dust
- Animal dander
- Pollens
- Molds
- Foods
- Pharmacologic agents
- Cigarette smoke
- Feathers
- Insect venoms
- Local manifestations of allergic reactions:
- Urticaria
- Pruritus
- Conjunctivitis
- Rhinitis
- Laryngeal edema
- Bronchospasm
- Dysrhythmia
- GI cramps
- Malabsorption
- Angioedema
- Medical treatment of patients with allergies:
- Antihistamines
- Bronchodilators
- Corticosteroids
- O2 and breathing treatments
- Topical lotions and ointments
- Nursing care for patients with allergies:
- Post allergies on the patient's record
- Never give any drug that the patient is allergic to
- Alert pharmacy and dietary to the patient's allergies
- Notify the provider of patient allergies
- Ensure patients taking allergy medications continue to do so
- Teach patient to limit exposure or avoid allergens
- Teach proper use of allergy medications
- Teach actions and side effects of medications
- Teach patient to wear a ID band that identifies their allergies
Anaphylaxis
- Definition: A life-threatening allergic reaction
- Causes of anaphylaxis:
- Antimicrobials
- Medicines or serums from animal sources
- Insect venom
- Iodine radioactive contrast media
- Local anesthetic
- Blood products
- Symptoms of anaphylaxis:
- Anxiety
- Wheezing
- Difficulty breathing
- Cyanosis
- Hives
- Facial edema
- Arthralgia
- Dizziness
- Hypotension
- Cardiac arrest
- Treatment of anaphylaxis:
- O2
- IV epinephrine
- Dopamine or a volume expander (or both) to raise BP
- Nebulized bronchodilator
- Diphenhydramine
- Corticosteroids
- Nursing care for patients with anaphylaxis:
- Prevent anaphylaxis when possible
- Prompt recognition of anaphylaxis
- Minimize patient's anxiety
- Administer prescribed drugs
- Monitor vital signs
Autoimmune Diseases
- Definition: When the immune system reacts against and destroys its own tissues
- Causes of autoimmune diseases:
- Injury to tissue
- Infection
- Malignancy
- Treatment of autoimmune diseases:
- Corticosteroids
- NSAIDs
- Immunosuppressive therapies
- Nursing care for patients with autoimmune diseases:
- Adequate rest
- Optimal hydration and nutrition
- Prevention of infection
- Supportive caring atmosphere
Organ Transplantation
- Definition: When a patient's own healthy immune system may recognize the allograft (implanted organ or tissue) as foreign and try to destroy it
- Types of rejection:
- Acute rejection
- Chronic rejection
- Treatment of rejection:
- Immunosuppressant drugs
- Corticosteroids
- Methotrexate
- Cyclosporine
- Nursing care for patients with transplanted organs:
- Monitor for signs of rejection
- Administer immunosuppressant drugs
- Educate patient on the importance of taking medication
- Teach patient to recognize signs of rejection
Drugs Used to Treat Immunologic Disorders
-
Corticosteroids:
- Used to suppress the immune response
- Used to prevent rejection of grafted tissue
- Treats RA, SLE, and MS
-
Calcineurin Inhibitors (CI):
- Used to prevent rejection of trans### SLE (Systemic Lupus Erythematosus) Patient Care
-
Closely monitor the patient's pain level and medication use.
-
Encourage the patient to avoid prolonged sun exposure and use sunscreen with an SPF of at least 30 to prevent skin rash.
-
Allow patients to express their feelings and ask questions, as a diagnosis of SLE can be shocking.
-
Ensure accurate and consistent information from the healthcare team to facilitate patient understanding.
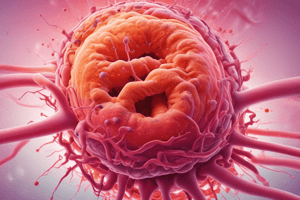
Human Immunodeficiency Virus (HIV)
- HIV causes immune cell destruction and is a retrovirus, transcribing genetic material in reverse.
- Infection occurs through blood and body fluids, and HIV attaches to macrophages and T4 helper cells, infusing its genetic material into the host cell.
- Over time, HIV destroys CD4+T cells faster than the body can replace them, leading to opportunistic infections when the immune response is severely impaired.
Stages of HIV Infection
- Initial stage: lasts 4-8 weeks from exposure, with 50% of people experiencing flu-like symptoms and the other 50% being asymptomatic.
- Latent stage: virus is inactive in infected resting CD4 host cells, lasting 2-12 years, during which the patient is asymptomatic and CD4 cells decline.
- Third stage: patient experiences opportunistic infections, with declining CD4 cell levels (<500) and increasing virus levels in the blood.
HIV Complications and Characteristics
- Opportunistic infections occur when CD4 cell levels fall below 200, and the patient is considered to have AIDS, with high virus levels in the blood.
- Antiretroviral drug regimens are abbreviated as ART or HAART.
- Clinical manifestations of HIV include malaise, nausea/vomiting, decreased appetite, rash, diarrhea, fever, night sweats, and others.
- Risk factors for HIV include unprotected sexual contact, IV drug use with shared needles, and blood transfusions before 1989.
HIV Complications
- Opportunistic infections, wasting, secondary cancers, and dementia.
- Patients with AIDS are at high risk for opportunistic fungal, parasitic, and viral infections, including oral candidiasis, pneumonia, herpes simplex, meningitis, and toxoplasmosis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the symptoms and signs of localized and generalized infections, including inflammation and contagiousness.