Podcast
Questions and Answers
What distinguishes the term 'microbiota' from 'microbiome'?
What distinguishes the term 'microbiota' from 'microbiome'?
- Microbiota includes viruses present in an area.
- Microbiota refers to the total number of microorganisms in an area. (correct)
- Microbiota refers to the genetic material of bacteria.
- Microbiota only includes beneficial bacteria.
What is the primary distinction between resident and transient microbiota?
What is the primary distinction between resident and transient microbiota?
- Resident microbiota are pathogenic while transient are not.
- Transient microbiota are always beneficial to the host.
- Transient microbiota are permanent residents of an area.
- Resident microbiota are fixed types found consistently, while transient microbiota are temporary. (correct)
How many species of microbes are typically found in the large intestine of an adult body?
How many species of microbes are typically found in the large intestine of an adult body?
- 99.9%
- 350 (correct)
- 1013
- 3.3 million
Which component is most critical for the formation of ecological niches within the human body?
Which component is most critical for the formation of ecological niches within the human body?
What percentage of genetic similarity is found among humans?
What percentage of genetic similarity is found among humans?
Which of the following statements about the intestinal microbiota is true?
Which of the following statements about the intestinal microbiota is true?
What is the common misconception about the term 'microflora'?
What is the common misconception about the term 'microflora'?
Which statement is correct regarding the uniqueness of an individual's microbiome?
Which statement is correct regarding the uniqueness of an individual's microbiome?
Which of the following microorganisms is typically found in the gut of healthy subjects?
Which of the following microorganisms is typically found in the gut of healthy subjects?
What is the main cause of enamel demineralization in dental caries?
What is the main cause of enamel demineralization in dental caries?
What is the main function of the lysozyme secreted by sweat glands?
What is the main function of the lysozyme secreted by sweat glands?
Which microorganisms contribute to the formation of the microbe pellicle on teeth?
Which microorganisms contribute to the formation of the microbe pellicle on teeth?
Which component of the skin microbiome represents the majority of fungal species?
Which component of the skin microbiome represents the majority of fungal species?
Which of the following pathogens is NOT typically associated with oral microbiota?
Which of the following pathogens is NOT typically associated with oral microbiota?
How does the pH level influenced by lactic acid secreted from sweat glands affect microbial colonization?
How does the pH level influenced by lactic acid secreted from sweat glands affect microbial colonization?
What role do Lactobacillus species play in the development of dental caries?
What role do Lactobacillus species play in the development of dental caries?
What is one of the ways that resident microbiota can be reduced according to the content?
What is one of the ways that resident microbiota can be reduced according to the content?
How does the microbe pellicle contribute to the pathogenicity of dental caries?
How does the microbe pellicle contribute to the pathogenicity of dental caries?
What is the relationship between carbohydrate cleavage and the acidic environment created by oral bacteria?
What is the relationship between carbohydrate cleavage and the acidic environment created by oral bacteria?
What characteristic best describes the skin's initial defense against microbial invasion?
What characteristic best describes the skin's initial defense against microbial invasion?
What role do sebaceous glands play in the skin's microbiome?
What role do sebaceous glands play in the skin's microbiome?
Which of the following best describes dental caries?
Which of the following best describes dental caries?
What is the effect of the anaerobic conditions promoted by extensive bacterial metabolism?
What is the effect of the anaerobic conditions promoted by extensive bacterial metabolism?
Which of the following statements about the human virome is true?
Which of the following statements about the human virome is true?
Which group of bacteria is typically found at higher concentrations in dental plaque compared to saliva?
Which group of bacteria is typically found at higher concentrations in dental plaque compared to saliva?
What is the typical microbe concentration observed in the oropharynx?
What is the typical microbe concentration observed in the oropharynx?
Which of the following is NOT associated with the Malassezia genus?
Which of the following is NOT associated with the Malassezia genus?
What is the typical concentration of microbes in saliva?
What is the typical concentration of microbes in saliva?
Which type of gland is primarily active after puberty and secretes sweat along with nutrients?
Which type of gland is primarily active after puberty and secretes sweat along with nutrients?
What defines an acute carrier of infectious pathogens?
What defines an acute carrier of infectious pathogens?
Which pathogen is classified as a strict pathogen?
Which pathogen is classified as a strict pathogen?
Which of the following is NOT a risk factor for opportunistic infections?
Which of the following is NOT a risk factor for opportunistic infections?
What differentiates opportunistic pathogens from strict pathogens?
What differentiates opportunistic pathogens from strict pathogens?
Which skin microbiota is considered to be constant and found in deeper parts of the skin?
Which skin microbiota is considered to be constant and found in deeper parts of the skin?
What percentage of skin microbiota is typically composed of Staphylococcus epidermidis?
What percentage of skin microbiota is typically composed of Staphylococcus epidermidis?
What effect do detergents have on skin microbiota?
What effect do detergents have on skin microbiota?
Which of the following is a common opportunistic pathogen?
Which of the following is a common opportunistic pathogen?
Which group of microorganisms are classified as chronic carriers infecting a significant number of people?
Which group of microorganisms are classified as chronic carriers infecting a significant number of people?
What is a characteristic of microbes that permanently colonize a human host?
What is a characteristic of microbes that permanently colonize a human host?
What role does gut microbiota play in neuropsychiatric disorders?
What role does gut microbiota play in neuropsychiatric disorders?
Which of the following bacteria are found in the colon's microbiota?
Which of the following bacteria are found in the colon's microbiota?
What is the pH level in the jejunum and ileum of the small intestine?
What is the pH level in the jejunum and ileum of the small intestine?
What is the potential impact of antibiotic courses on patients with gastrointestinal diseases regarding mental health?
What is the potential impact of antibiotic courses on patients with gastrointestinal diseases regarding mental health?
Which of the following is NOT identified as a neuroactive compound produced by gut microbes?
Which of the following is NOT identified as a neuroactive compound produced by gut microbes?
Which bacteria are commonly found in the urogenital microbiota of the urethra?
Which bacteria are commonly found in the urogenital microbiota of the urethra?
Flashcards are hidden until you start studying
Study Notes
Human Microbiome Terminology
- Microflora is an outdated term used when only two kingdoms (Animalia and Planta) were recognized.
- Microbiota refers to the total number of microorganisms found in a specific area.
- Microbiome encompasses the genomes of the microbiota, studied through genome examination.
- Metagenomics is the direct study of genetic material from microbial communities, analyzing DNA from multiple bacteria simultaneously.
Human Microbiome Facts
- The intestinal microbiota harbors 3.3 million genes, vastly exceeding the approximately 22,000 genes in the human genome.
- Humans share 99.9% genetic similarity, but their intestinal and skin microbiomes differ by 80-90%, highlighting the unique individuality of individual microbiomes.
- The human microbiome exhibits regional diversity, with E. coli prevalent in the gut of most healthy individuals and Staphylococcus epidermitis inhabiting the skin.
Microbiota Classification
- Resident or constant (obligatory) microbiota: Fixed types of microorganisms permanently residing in a given area at a specific age.
- Transient microbiota (facultative): Non-pathogenic or potentially pathogenic microorganisms temporarily inhabiting the skin or mucous membranes for hours, days, or weeks.
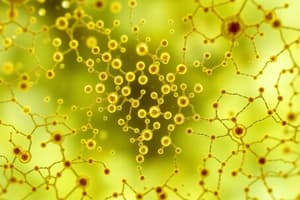
Ecological Niches
- Each body region with a characteristic set of microbes constitutes an ecological niche.
- The types of microorganisms vary across different areas of the body.
- The human body harbors an estimated 10^13 bacteria, with 350 species in the large intestine.
- Bacterial adherence (via adhesins) and exposure to microorganisms influence the formation of ecological niches.
- Individuals can be categorized as carriers, carrying microorganisms that may or may not cause disease, and classified into two groups:
- Acute carrier: Exhibiting a short-term carrier state.
- Chronic carrier: Carrying specific microbes for prolonged periods, for example, individuals carrying Staphylococcus aureus (20-40%), Streptococcus pneumoniae (40-70%), or Salmonella typhi (a lower percentage).
- Exposure to a microorganism can result in:
- Transient colonization: The microbe temporarily resides in the individual.
- Permanent colonization: The microbe becomes a permanent resident.
- Disease: The interaction between the microbe and the human host leads to a pathogenic process, causing damage to the host.
Causative Agents of Infectious Diseases
- Strict pathogens: Microorganisms consistently associated with disease in humans, such as Mycobacterium tuberculosis, Neisseria gonorrhoeae, Francisella tularensis, Plasmodium species, and Rhabdoviruses.
- Opportunistic pathogens: Typically harmless members of the normal microbiota that can cause disease when introduced into vulnerable sites (e.g., bloodstream, tissues), examples include Staphylococcus aureus, Escherichia coli, and Candida albicans.
Risk Factors for Opportunistic Infections
- Immunodeficiency
- Chronic diseases (e.g., diabetes)
- Gastric ulcers
- Stress
- Antibacterial treatment
- Malnutrition
- Avitaminosis
Skin Microbiota
- Transient microbiota: Superficial, temporary residents.
- Resident microbiota: Constant inhabitants of deeper skin layers.
- Approximately 10^3-10^4 microbes reside per square centimeter.
- Common skin microbiota members include:
- Staphylococcus epidermidis (90%)
- Corynebacterium
- Cutibacterium acnes
- Malassezia
- Candida
Factors Influencing Skin Microbiota
- Detergents: Reduce transitory and superficial microbiota by 90%, with recolonization occurring within 8 hours.
- Disinfectants: Eliminate resident microbiota.
- Sex
- Age
- Climate
- UV rays
- Hygiene
- Profession
- Diseases
Skin as a Defense Barrier
- Intact skin serves as the first line of defense against microbial invasion.
- Skin's dryness makes it unsuitable for many microbial growth.
- Skin microbiota is sustained by nutrients provided by sweat and sebaceous glands.
- Sweat glands:
- Eccrine glands: Secrete sweat.
- Apocrine glands: Secrete sweat and nutrients, more active after puberty.
- Sweat contains:
- Lysozyme: Breaks down peptidoglycan, a bacterial cell wall component.
- Lactic acid: Lowers pH to 3-5, inhibiting bacterial colonization.
- Sebaceous glands:
- Attached to hair follicles.
- Secrete sebum, supporting microbial growth up to 10^6 per square centimeter.
Skin Mycobiome
- The skin mycobiome refers to the fungal species inhabiting the skin.
- Fungi constitute 30% of the skin microbiota, with Malassezia strains dominating.
- Malassezia species, including M. globosa, M. restricta, and M. furfur, represent over 90% of fungal populations in most skin niches.
- The role of Malassezia on the skin is controversial, linked to both healthy skin and conditions like dandruff and eczema.
Human Virome
- The human virome encompasses all viruses residing within or on human organs, including the skin.
- Human stools contain at least 10^9 virus-like particles (VLPs) per gram.
- Bacteriophages comprise 96.1% of the human gut viral populations.
- The human virome potentially influences human health, beyond disease.
Microbiota of Nasopharynx and Oropharynx
- Nasopharynx:
- Microbe amount: 10^5 per milliliter.
- Microbes: Staphylococcus epidermidis, Corynebacterium, Propionibacterium, Haemophilus parainfluenzae.
- Pathogens: Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Neisseria meningitidis.
- Oropharynx:
- Microbe amount: 10^7 per milliliter.
- Microbes: Staphylococcus, Streptococcus, *Corynebacterium, Propionibacterium, Neisseria species, Branhamella catarrhalis, Bacteroides, Fusobacterium, Enterococcus.
- Pathogens: Streptococcus (α-hemolytic), Corynebacterium diphtheriae, Klebsiella pneumoniae, Pseudomonas aeruginosa.
Microbiota of Oral Cavity
- Microbe amount in saliva: 10^8 per milliliter.
- Microbe amount in teeth plaque: 10^11 per gram.
- Microbes: Streptococcus salivarius, S. sanguis, S. milleri, S. mutans, Staphylococcus, Enterococcus, Veilonella, Neisseria, Bacteroides orale, Fusobacterim nucleatum, Leptrotrichia buccalis, Actinomyces, Vibrio, Spirocheta (including Treponema orale, Borrelia buccalis, Leptospira dentium), Candida albicans, Saccharomyces, Prevotella malinogenica, Porphyromonas gingivalis, etc.
Dental Caries
- Polyaethiologic disease, meaning multiple factors contribute to its development.
- Caries refers to tooth disintegration, starting at the surface and progressing inward.
- Demineralization of the enamel surface is caused by acidic byproducts of bacterial fermentation.
- Subsequent decomposition of the dentin and cement follows.
Microbial Mechanism of Caries
- After a meal, a thin layer of saliva (microbe pellicle, around 0.1 micrometer) forms on the tooth surface.
- The microbe pellicle provides a site for bacteria to attach.
- Over time, microbes multiply and ferment carbohydrates, producing glucan and fructan, lowering pH and promoting anaerobic conditions.
- The resulting environment favors facultative anaerobes and even anaerobes.
- Lactobacillus bacteria, producing lactic acid, further acidify the environment.
- The high concentration of lactic acid leads to demineralization, initiating dental caries.
- Dental caries is also a biofilm, shielding bacteria from immune cells and antibiotics.
Gastrointestinal Microbiota
- Stomach:
- pH: 1-3.
- Microbe amount: 10^1-10^3 colony-forming units per milliliter (CFU/ml).
- Oxygen partial pressure (PO2): 77 mmHg.
- Microbes: Lactobacillus, Streptococcus, Staphylococcus, Enterobacteriaceae.
- Duodenum:
- Microbe amount: 10^1-10^3 CFU/ml.
- PO2: 33 mmHg.
- Microbes: Lactobacillus, Streptococcus, Staphylococcus, Enterobacteriaceae.
- Small Intestine (jejunum and ileum):
- pH: 6-7.
- Microbe amount: 10^4-10^7 CFU/ml.
- PO2: 33 mmHg.
- Microbes: Bifidobacterium, Bacteroides, Lactobacillus, Streptococcus, Enterobacteriaceae.
- Colon:
- pH: 7.
- Microbe amount: 10^10-10^11 CFU/ml.
- PO2: < 33 mmHg.
- Microbes: Fusobacterium, Eubacterium, Clostridium, Peptostreptococcus, Bifidobacterium, Streptococcus, Bacteroides, Lactobacillus, Enterobacteriaceae.
Gut-Brain-Microbiota Axis
- Variations in gut microbiota play a significant role in the development of neuropsychiatric disorders.
- Communication along this axis is bidirectional.
- Antibiotic treatment for gastrointestinal diseases can increase the risk of depression and anxiety symptoms.
- Gut microbes provide neuroactive compounds and immune modulators, including serotonin, dopamine, γ-aminobutyric acid, acetylcholine, histamine, and short-chain fatty acids.
Urogenital Microbiota
- Vagina:
- Microbe amount: 10^9 per milliliter.
- Microbes: Staphylococcus epidermidis, Peptostreptococcus, Neisseria species, Corynebacterium species.
- Urethra:
- Microbes: Staphylococcus epidermidis, Streptococcus, Corynebacterium species.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.