Podcast
Questions and Answers
What is the main function of the hepatic portal vein in the human circulatory system?
What is the main function of the hepatic portal vein in the human circulatory system?
To carry blood from the gastrointestinal tract and spleen to the liver.
Define the term 'arterial pulse' and describe how it is measured.
Define the term 'arterial pulse' and describe how it is measured.
Arterial pulse refers to the alternating expansion and recoil of blood vessel walls as the heart beats, measured at superficial arteries.
What are the primary components that determine blood pressure in the circulatory system?
What are the primary components that determine blood pressure in the circulatory system?
Blood pressure is determined by the force exerted by circulating blood on the vessel walls and the resistance of the blood vessels.
How does the inferior vena cava function in the cardiovascular system?
How does the inferior vena cava function in the cardiovascular system?
Explain the significance of measuring respiratory rate as part of vital signs.
Explain the significance of measuring respiratory rate as part of vital signs.
Identify the blood vessels where a pulse can be most easily palpated and explain their significance.
Identify the blood vessels where a pulse can be most easily palpated and explain their significance.
Discuss the role of the spleen in relation to the hepatic portal system.
Discuss the role of the spleen in relation to the hepatic portal system.
What is the normal resting heart rate range in a healthy individual, and how does it relate to cardiovascular health?
What is the normal resting heart rate range in a healthy individual, and how does it relate to cardiovascular health?
What is the role of the sympathetic nervous system during a crisis stressor?
What is the role of the sympathetic nervous system during a crisis stressor?
How do changes in blood volume influence venous return?
How do changes in blood volume influence venous return?
Describe the function of capillary beds in the circulatory system.
Describe the function of capillary beds in the circulatory system.
What hormonal changes occur when the crisis has passed?
What hormonal changes occur when the crisis has passed?
What are the primary vessels involved in transporting blood away from the heart?
What are the primary vessels involved in transporting blood away from the heart?
How does exercise impact blood pressure and cardiac output?
How does exercise impact blood pressure and cardiac output?
Explain the effect of the vagus nerve on heart function.
Explain the effect of the vagus nerve on heart function.
What is the relationship between stroke volume and cardiac output?
What is the relationship between stroke volume and cardiac output?
What is the primary mechanism by which oxygen and nutrients are exchanged between blood and tissue cells?
What is the primary mechanism by which oxygen and nutrients are exchanged between blood and tissue cells?
Explain how blood pressure and osmotic pressure influence fluid movement at capillary beds.
Explain how blood pressure and osmotic pressure influence fluid movement at capillary beds.
List the four routes through which substances can diffuse into and out of capillaries.
List the four routes through which substances can diffuse into and out of capillaries.
What role does interstitial fluid play in the exchange of substances between blood and tissue?
What role does interstitial fluid play in the exchange of substances between blood and tissue?
How do concentration gradients affect the movement of carbon dioxide and other waste products from tissue cells to the blood?
How do concentration gradients affect the movement of carbon dioxide and other waste products from tissue cells to the blood?
Describe the significance of fenestrated capillaries in the context of nutrient and gas exchange.
Describe the significance of fenestrated capillaries in the context of nutrient and gas exchange.
In what way does direct diffusion through membranes differ from other diffusion mechanisms in capillaries?
In what way does direct diffusion through membranes differ from other diffusion mechanisms in capillaries?
Discuss the impact of blood pressure regulation on overall tissue health and function.
Discuss the impact of blood pressure regulation on overall tissue health and function.
What initiates each heartbeat in the intrinsic conduction system of the heart?
What initiates each heartbeat in the intrinsic conduction system of the heart?
Describe the pathway of the electrical impulse from the SA node to the ventricles.
Describe the pathway of the electrical impulse from the SA node to the ventricles.
What role does the Atrioventricular (AV) node play in the conduction system of the heart?
What role does the Atrioventricular (AV) node play in the conduction system of the heart?
What are the Purkinje fibers and where are they located?
What are the Purkinje fibers and where are they located?
What is the significance of the AV bundle (bundle of His) in the heart's conduction system?
What is the significance of the AV bundle (bundle of His) in the heart's conduction system?
What does it mean when the blood pressure cuff is inflated above 120 mm Hg?
What does it mean when the blood pressure cuff is inflated above 120 mm Hg?
Why can no sounds be heard when the cuff pressure is above 120 mm Hg?
Why can no sounds be heard when the cuff pressure is above 120 mm Hg?
What is the significance of feeling no brachial pulse when the cuff is inflated?
What is the significance of feeling no brachial pulse when the cuff is inflated?
What happens when the cuff pressure is released gradually?
What happens when the cuff pressure is released gradually?
What does wrapping the cuff snugly around the arm ensure during measurement?
What does wrapping the cuff snugly around the arm ensure during measurement?
How does Starling’s law of the heart influence stroke volume (SV)?
How does Starling’s law of the heart influence stroke volume (SV)?
What are the primary neural controls modifying heart rate and their effects?
What are the primary neural controls modifying heart rate and their effects?
Explain the role of the muscular pump in regulating venous return.
Explain the role of the muscular pump in regulating venous return.
Discuss how physical factors influence heart rate variability.
Discuss how physical factors influence heart rate variability.
What is the impact of hormones like epinephrine on heart rate?
What is the impact of hormones like epinephrine on heart rate?
What major arteries supply most of the cerebrum?
What major arteries supply most of the cerebrum?
What structure forms from the joining of the vertebral arteries within the skull?
What structure forms from the joining of the vertebral arteries within the skull?
What physiological changes occur during ventricular systole?
What physiological changes occur during ventricular systole?
What is the significance of isovolumetric relaxation in the cardiac cycle?
What is the significance of isovolumetric relaxation in the cardiac cycle?
Which arteries form the posterior cerebral arteries?
Which arteries form the posterior cerebral arteries?
How are the anterior and posterior blood supplies of the brain connected?
How are the anterior and posterior blood supplies of the brain connected?
How are heart sounds produced during the cardiac cycle?
How are heart sounds produced during the cardiac cycle?
What is the common name for the cerebral arterial circle?
What is the common name for the cerebral arterial circle?
Define cardiac output and explain how it is calculated.
Define cardiac output and explain how it is calculated.
What role do heart murmurs play in cardiac health assessment?
What role do heart murmurs play in cardiac health assessment?
Which artery is primarily responsible for supplying the temporal lobe?
Which artery is primarily responsible for supplying the temporal lobe?
What role does the anterior communicating artery play in the blood supply to the brain?
What role does the anterior communicating artery play in the blood supply to the brain?
What are the typical values for stroke volume and heart rate used in cardiac output calculations?
What are the typical values for stroke volume and heart rate used in cardiac output calculations?
In the context of the cardiac cycle, what occurs when atrial pressure exceeds intraventricular pressure?
In the context of the cardiac cycle, what occurs when atrial pressure exceeds intraventricular pressure?
Which two structures do the internal carotid and vertebral arteries nourish?
Which two structures do the internal carotid and vertebral arteries nourish?
What is the relationship between blood ejection during ventricular systole and the cardiac cycle events?
What is the relationship between blood ejection during ventricular systole and the cardiac cycle events?
What is the purpose of the ductus venosus in fetal circulation?
What is the purpose of the ductus venosus in fetal circulation?
How does blood flow through the heart change at birth?
How does blood flow through the heart change at birth?
What is the role of the ductus arteriosus during fetal development?
What is the role of the ductus arteriosus during fetal development?
What anatomical structure replaces the foramen ovale after birth?
What anatomical structure replaces the foramen ovale after birth?
What happens to the ductus arteriosus after birth?
What happens to the ductus arteriosus after birth?
Why is it necessary for fetal blood to bypass the lungs?
Why is it necessary for fetal blood to bypass the lungs?
Which shunt directly links the right atrium to the left atrium in a fetus?
Which shunt directly links the right atrium to the left atrium in a fetus?
How does the ductus venosus contribute to fetal circulation?
How does the ductus venosus contribute to fetal circulation?
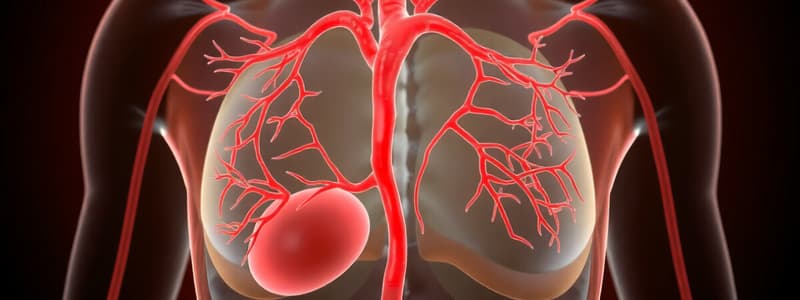
What is the function of the brachiocephalic trunk in the human circulatory system?
What is the function of the brachiocephalic trunk in the human circulatory system?
Describe the path that blood takes from the right atrium to the lungs.
Describe the path that blood takes from the right atrium to the lungs.
How do the left and right coronary arteries differ in their supply to the heart?
How do the left and right coronary arteries differ in their supply to the heart?
What is the role of the ligamentum arteriosum in the anatomy of the heart?
What is the role of the ligamentum arteriosum in the anatomy of the heart?
Explain the significance of the apex of the heart.
Explain the significance of the apex of the heart.
What is the primary purpose of capillary beds in the lungs?
What is the primary purpose of capillary beds in the lungs?
Explain the difference between pulmonary arteries and pulmonary veins.
Explain the difference between pulmonary arteries and pulmonary veins.
What role does the left atrium play in the pulmonary circuit?
What role does the left atrium play in the pulmonary circuit?
How does the systemic circuit differ from the pulmonary circuit?
How does the systemic circuit differ from the pulmonary circuit?
Identify the significance of the venae cavae in the circulatory system.
Identify the significance of the venae cavae in the circulatory system.
What is the primary function of capillary beds found throughout the body's tissues?
What is the primary function of capillary beds found throughout the body's tissues?
Describe how the aorta is connected to the systemic circuit.
Describe how the aorta is connected to the systemic circuit.
Explain the relationship between the heart's right ventricle and the pulmonary arteries.
Explain the relationship between the heart's right ventricle and the pulmonary arteries.
What are the two types of blood pressure measured during the cardiac cycle?
What are the two types of blood pressure measured during the cardiac cycle?
Explain the blood pressure gradient as blood travels away from the heart.
Explain the blood pressure gradient as blood travels away from the heart.
How is blood pressure typically expressed in clinical settings?
How is blood pressure typically expressed in clinical settings?
What does an indirect method of measuring systemic arterial blood pressure involve?
What does an indirect method of measuring systemic arterial blood pressure involve?
What physiological process causes blood to flow from the arteries to the veins?
What physiological process causes blood to flow from the arteries to the veins?
What occurs during the ejection phase of ventricular systole?
What occurs during the ejection phase of ventricular systole?
Describe the events that characterize isovolumetric relaxation.
Describe the events that characterize isovolumetric relaxation.
Describe the relationship between systolic and diastolic pressure.
Describe the relationship between systolic and diastolic pressure.
What are the characteristics of the 'Lub' and 'Dup' heart sounds?
What are the characteristics of the 'Lub' and 'Dup' heart sounds?
What happens to the blood pressure as it enters the capillaries?
What happens to the blood pressure as it enters the capillaries?
How is cardiac output (CO) calculated, and what are its normal values?
How is cardiac output (CO) calculated, and what are its normal values?
What is the significance of measuring blood pressure regularly?
What is the significance of measuring blood pressure regularly?
What does turbulent blood flow indicate, and how is it related to heart murmurs?
What does turbulent blood flow indicate, and how is it related to heart murmurs?
Explain the role of atrial pressure in relation to intraventricular pressure during the cardiac cycle.
Explain the role of atrial pressure in relation to intraventricular pressure during the cardiac cycle.
What is the stroke volume (SV), and how much blood is typically pumped from the left ventricle each heartbeat?
What is the stroke volume (SV), and how much blood is typically pumped from the left ventricle each heartbeat?
During which phase of the cardiac cycle are the ventricles fully closed chambers, and what is its significance?
During which phase of the cardiac cycle are the ventricles fully closed chambers, and what is its significance?
What does a blood pressure cuff reading of 120 mm Hg signify during measurement?
What does a blood pressure cuff reading of 120 mm Hg signify during measurement?
At what pressure is no sound audible in the stethoscope when measuring blood pressure?
At what pressure is no sound audible in the stethoscope when measuring blood pressure?
Describe the significance of the first soft tapping sounds heard during blood pressure measurement.
Describe the significance of the first soft tapping sounds heard during blood pressure measurement.
What happens to the sounds detected by the stethoscope as the cuff pressure is gradually released past the systolic level?
What happens to the sounds detected by the stethoscope as the cuff pressure is gradually released past the systolic level?
What physiological state is represented by a cuff pressure below 70 mm Hg?
What physiological state is represented by a cuff pressure below 70 mm Hg?
How is systolic pressure measured using a stethoscope during the blood pressure assessment?
How is systolic pressure measured using a stethoscope during the blood pressure assessment?
What is the role of the stethoscope in blood pressure measurement?
What is the role of the stethoscope in blood pressure measurement?
Why is it important to monitor the pressure range of 70 mm Hg to 120 mm Hg during blood pressure assessment?
Why is it important to monitor the pressure range of 70 mm Hg to 120 mm Hg during blood pressure assessment?
What dietary components are commonly believed to prevent hypertension?
What dietary components are commonly believed to prevent hypertension?
What is the normal systolic blood pressure range for humans?
What is the normal systolic blood pressure range for humans?
Define hypotension and its associated systolic blood pressure threshold.
Define hypotension and its associated systolic blood pressure threshold.
What constitutes hypertension, and what systolic and diastolic readings define it?
What constitutes hypertension, and what systolic and diastolic readings define it?
How do chemicals like renin affect blood pressure?
How do chemicals like renin affect blood pressure?
What role does the sympathetic nervous system play concerning blood pressure?
What role does the sympathetic nervous system play concerning blood pressure?
What physiological changes occur that lead to increased cardiac output?
What physiological changes occur that lead to increased cardiac output?
Explain the significance of postural changes in blood pressure regulation.
Explain the significance of postural changes in blood pressure regulation.
Study Notes
Cardiovascular System
- A closed system of the heart and blood vessels
- The heart pumps blood
- Blood vessels allow blood to circulate to all parts of the body
- Functions of the cardiovascular system include transporting oxygen, nutrients, cell wastes, and hormones to and from cells
Anatomy of the Heart
- Size of a human fist, weighing less than a pound
- Located in the thoracic cavity, between the lungs in the inferior mediastinum
- Orientation:
- Apex is directed toward the left hip and rests on the diaphragm
- Base points toward the right shoulder
Coverings of the Heart
- Pericardium-a double-walled sac
- Fibrous pericardium is loose and superficial
- Serous membrane is deep to the fibrous pericardium and composed of two layers:
-
- Parietal pericardium: outside layer that lines the inner surface of the fibrous pericardium
-
- Visceral pericardium: next to heart; also known as the epicardium
-
- Serous fluid fills the space between the layers of pericardium, called the pericardial cavity
Functions of the Pericardium
- Keeps the heart contained within the chest cavity
- Prevents the heart from overexpanding when blood volume increases
- Limits heart motion
- Reduces friction between the heart and surrounding tissues
- Protects the heart against infection
Walls of the Heart
- Epicardium (Pericardium):
- Outside layer; the visceral pericardium
- Myocardium:
- Middle layer; the thickest layer
- Mostly cardiac muscle
- The layer that contracts
- Endocardium:
- Inner layer known as endothelium
- Lines the inner heart chambers, covers heart valves and continuous with the endothelium of large blood vessels
Chambers and Associated Great Vessels
- Four chambers of the heart:
- Atria (right and left): Receiving chambers, assist with filling the ventricles, blood enters under low pressure
- Ventricles (right and left): Discharging chambers, thick-walled pumps of the heart, during contraction, blood is propelled into circulation
- Interatrial septum: Separates the two atria longitudinally
- Interventricular septum: Separates the two ventricles longitudinally
Heart Valves
- Allow blood to flow in only one direction, preventing backflow
- Valves open and close in response to pressure changes in the heart
- Atrioventricular (AV) valves-between atria and ventricles:
- Left AV valve: bicuspid (mitral) valve
- Right AV valve: tricuspid valve
- Function: Anchored by chordae tendineae to the walls of the ventricles. Open during heart relaxation, when blood passively fills the chambers. Closed during ventricular contraction
- Semilunar valves-between ventricle and artery:
- Pulmonary semilunar valve
- Aortic semilunar valve
- Function: Closed during heart relaxation. Open during ventricular contraction
Cardiac Circulation
- Blood in the heart chambers does not nourish the myocardium
- The heart has its own nourishing circulatory system consisting of:
- Coronary arteries: branch from the aorta to supply the heart muscle with oxygenated blood.
- Cardiac veins: drain the myocardium of blood
- Coronary sinus: a large vein on the posterior of the heart; receives blood from cardiac veins. Blood empties into the right atrium via the coronary sinus
Gross Anatomy of Blood Vessels
-
Major arteries of systemic circulation:
- Aorta: Largest artery, leaves from the left ventricle of the heart. Regions include ascending aorta, aortic arch, thoracic aorta, and abdominal aorta
- Arterial branches of the ascending aorta: Right and left coronary arteries serve the heart
- Arterial branches of the aortic arch: Brachiocephalic trunk, Right common carotid artery, Right subclavian artery, Left common carotid artery, Left internal and external carotid arteries, Left subclavian artery, Vertebral artery
- Arterial branches of the thoracic aorta: Intercostal arteries supply the muscles of the thorax wall, Lungs (bronchial arteries), Esophagus (esophageal arteries), Diaphragm (phrenic arteries)
- Arterial branches of the abdominal aorta: Celiac trunk (left gastric artery, splenic artery, common hepatic artery), Superior mesenteric artery, Left and right renal arteries, Left and right gonadal arteries (ovarian arteries in females, testicular arteries in males), Lumbar arteries
- Arterial branches of the abdominal aorta (continued): Inferior mesenteric artery, Left and right common iliac arteries, Internal iliac arteries, External iliac arteries, Femoral artery, Popliteal artery, Anterior tibial artery, Posterior tibial artery, Dorsalis pedis artery, Arcuate artery
-
Major veins of systemic circulation:
- Superior vena cava and inferior vena cava enter the right atrium of the heart, the superior vena cava drains the head and arms, and the inferior vena cava drains the lower body
- Veins draining into the superior vena cava: Radial and ulnar veins, Cephalic vein, Basilic vein, Subclavian vein, Vertebral vein, Internal jugular vein, Brachiocephalic veins
- Veins draining into the inferior vena cava: Anterior and posterior tibial veins, Great saphenous veins, Common iliac vein, Internal iliac arteries, External iliac vein, Femoral vein, Popliteal vein, Posterior tibial veins, Anterior tibial vein, Small saphenous vein, Dorsal venous arch, Dorsal metatarsal veins, Hepatic portal vein, Hepatic veins, Splenic vein, Gastric veins, Inferior mesenteric vein, Superior mesenteric vein, Renal veins, Left and right gonadal veins
-
Arterial supply of the brain and the circle of Willis:
- Internal carotid arteries divide into Anterior and middle cerebral arteries
- These arteries supply most of the cerebrum
- Vertebral arteries join to form the Basilar artery
- Basilar artery serves the brain stem and cerebellum
- Posterior cerebral arteries are formed from the division of the basilar artery and supply the posterior cerebrum
- Anterior and posterior blood supplies to the brain are united by small communicating arterial branches which form the cerebral arterial circle, or circle of Willis
-
Hepatic portal circulation:
- Formed by veins draining the digestive organs which empty into the hepatic portal vein. The digestive organs, spleen, and pancreas drain into the portal vein before draining into the liver
Physiology of Circulation
- Vital signs: Measurements of arterial pulse, blood pressure, respiratory rate, and body temperature
- Arterial pulse: Alternate expansion and recoil of a blood vessel wall, where pulse is easily palpated
- Blood pressure: The pressure the blood exerts against the inner walls of blood vessels, the force that causes blood to continue to flow in the blood vessels
- Blood pressure gradient: When the ventricles contract, blood is forced into elastic arteries close to the heart, the pressure decreases in the blood vessels as distance from the heart increases. Pressure is high in arteries, lower in capillaries, and lowest in veins
- Measuring blood pressure: Systolic/diastolic pressure (e.g., 120/80 mm Hg), Auscultatory method
- Effects of various factors on blood pressure: Factors include cardiac output, peripheral resistence, neural, renal, temperature, chemical, and diet
Capillary Exchange
- Interstitial fluid (tissue fluid) is found between cells
- Substances move to and from the blood and tissue cells through capillary walls
- Exchange is due to concentration gradients
- Oxygen and nutrients leave the blood and move into tissue cells
- Carbon dioxide and other wastes exit tissue cells and enter the blood
- Substances take various routes entering or leaving blood including direct diffusion through membranes, diffusion through intercellular clefts, and diffusion through pores in fenestrated capillaries
- Fluid moves out of capillaries at the arterial end and is reclaimed at the venous end of the bed and fluid movement is dependent upon blood pressure and osmotic pressure
Developmental Aspects of the Cardiovascular System
- In an embryo, the heart develops as a simple tube and pumps blood by week 4, becoming a four-chambered organ capable of acting as a double pump over the next 3 week
- Umbilical cord-Carries nutrients and oxygen from maternal blood to fetal blood. Fetal wastes move from fetal blood to maternal blood. One umbilical vein carries nutrient and oxygen-rich blood to the fetus. Two umbilical arteries carry wastes and carbon dioxide-rich blood from the fetus to the placenta
- Shunts bypassing the lungs and liver are present in a fetus:
- Blood flow bypasses the liver through the ductus venosus and enters the inferior vena cava → right atrium of the heart
- Blood flow bypasses the lungs: Blood entering right atrium is shunted directly into left atrium through the foramen ovale (becomes fossa ovalis at or after birth). Ductus arteriosus connects aorta and pulmonary trunk, becomes ligamentum arteriosum at birth
Age-related problems
- Weakening of venous valves
- Varicose veins
- Progressive arteriosclerosis
- Hypertension
- Coronary artery disease
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.